Caecal bascule is an infrequent type of caecal volvulus. It appears when the caecum folds upon itself, causing an intestinal obstruction. It is usually diagnosed using imaging techniques or intra-operatively. A constrictive band related to previous abdominal surgery is frequently present, and acts as an inflexion point that results in a closed loop obstruction of the ascending colon. It has been reported in young women and in elderly hospitalised patients.
The aim of this report is to describe the clinical features, diagnostic difficulties, and management strategies of this unusual entity.
Clinical caseAn 83-year-old male with concurrent acute neurological illness presented with history of intestinal obstruction. Because of a previous right nephrectomy, postoperative adhesions were suspected and conservative treatment initiated. As no improvement was seen, a computed tomography scan was obtained. Abdominal tomography showed an intestinal obstruction and a caecal bascule with vascular compromise. A right colectomy was performed.
ConclusionsCaecal bascule is a rare cause of intestinal obstruction. The suspicion should be heightened when caecal ectopic dilation is present. Computed tomography scan is the preferred imaging technique, especially for ill patients. Right colectomy and primary anastomosis is the most appropriate surgical technique. Awareness of this entity can prevent the high morbidity and mortality rates of this condition.
La báscula cecal es un tipo infrecuente de vólvulo cecal. Se produce al plegarse el ciego sobre el colon ascendente, causando una obstrucción intestinal. El diagnóstico suele ser radiológico o intraoperatorio. Es frecuente la existencia de una brida secundaria a intervenciones previas que obstruye el colon ascendente y actúa como eje de inflexión. Es frecuente en mujeres jóvenes y en pacientes ancianos hospitalizados.
El objetivo de este trabajo es resaltar las características clínicas y la dificultad en el diagnóstico de la báscula cecal como causa de obstrucción intestinal, así como las estrategias de tratamiento de esta inusual entidad.
Caso clínicoVarón de 83 años con enfermedad neurológica intercurrente, que presenta datos clínicos compatibles con obstrucción intestinal. Se sospecha que su origen es por adherencias, en relación con el antecedente de nefrectomía derecha, por lo que se instaura tratamiento conservador; debido a que no presenta mejoría, se le realizó una tomografía computada. Esta pone en evidencia una obstrucción intestinal, pero debida a una báscula cecal con compromiso vascular. El paciente requirió una intervención urgente con hemicolectomía derecha.
ConclusionesLa báscula cecal es una causa inusual de obstrucción intestinal. Su diagnóstico debe sospecharse siempre que exista dilatación cecal ectópica. La tomografía computada es la prueba de imagen de elección, especialmente en pacientes graves. La resección y anastomosis ilecólica es la opción quirúrgica más recomendable. Es necesario un alto índice de sospecha y un tratamiento precoz para evitar complicaciones.
Intestinal volvulus is caused by torsion of the mesentery and its vessels, producing symptoms of intestinal obstruction.
The most common location is the sigmoid colon (80%), followed by the caecum (15%), the least usual location is the transverse colon (5%).1
Caecal volvulus can be subdivided into 2 types, and the most common, at 90% of cases, is due to torsion of the caecum over its axial axis, usually in a clockwise direction. The second type is termed caecal bascule and represents 10% of caecal volvuli.2 Caecal bascule is characterised by a cephalic fold of the caecum, located in the upper part of the abdomen; there is no torsion of the mesentery, therefore vascular compromise is less likely.3,4
Diagnosis is usually radiological or intra-operative in the context of an intestinal obstruction. Right hemicolectomy is the technique of choice for treatment.
The aim of presenting this case is to describe the clinical features of this rare cause of intestinal obstruction and highlight the difficulty in its diagnosis and strategies for treatment.
Clinical caseAn 83-year-old male with a history of chronic obstructive pulmonary disease, chronic renal failure after right nephrectomy associated with a renal tumour, paroxysmal atrial flutter and ischaemic ictus, with no sequelae.
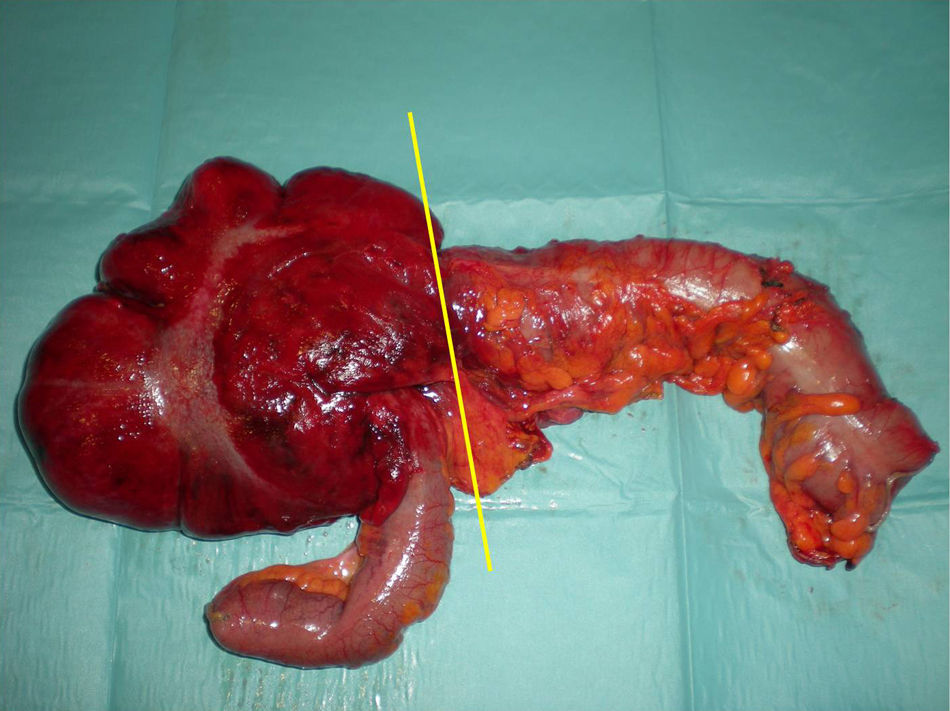
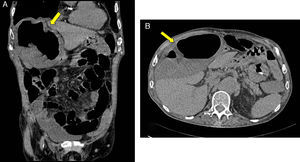
The patient was admitted to the Neurological Department with a left hemisphere syndrome, secondary to a haematoma in the posterior limb of the right internal capsule, probably due to high blood pressure and associated with an overdose of Sintrom®. During admission he started vomiting, colicky abdominal pain that became diffuse, associated with an absence of intestinal transit. The physical examination found moderate abdominal distension, more striking in the right hemi-abdomen, with increased bowel sounds. The laboratory tests showed: 13,500leukocytes with 87% neutrophils, creatinine 2.1mg/dl, urea 101mg/dl and C reactive protein 178mg/l. Plain chest X-ray showed major dilation of the small bowel loops in the right hypochondrium, as well as the mesogastrium and hypogastrium (Fig. 1). Given the history of laparotomy, adhesion syndrome was suspected and therefore conservative treatment was started. However the patient presented clinical deterioration and a CT scan was performed which showed the presence of perihepatic free fluid and free fluid in the right gutter, in addition to marked dilation of the caecum, which was ascending (Fig. 2). The patient presented a point of change in the calibre of the ascending colon; all of these signs indicated caecal volvulus. An urgent laparotomy was decided, and found a mobile, pendulous caecum that was very distended, and vascular compromise (Fig. 3); it was also folded over its own axis in a cranial direction in relation to a postoperative adhesion that was acting as an inflection point (Fig. 4). An urgent right hemicolectomy was performed with mechanical latero-lateral ileocolic anastomosis. The pathological anatomy result reported the presence of alterations compatible with an ischaemic process.
The post-operative period passed without incident, therefore the patient was discharged.
DiscussionAccording to Datta and Sakran,5 caecal bascule was first described by Treves in 1899, but it was Weinstein who later defined it as a subtype of caecal volvulus in 1938. It represents 10% of the cases of caecal volvulus,2,5,6 which occurs most commonly in young women7 and during the postpartum period, when the caecum is displaced upwards by the uterus.
Chronic constipation, high fibre consumption, laxative abuse and prolonged immobilisation are considered to be predisposing factors.2 Due to the latter factor, it frequently occurs in elderly patients and patients hospitalised for other reasons, since their intestinal mobility is reduced and there is greater colonic dilation.6 Other causes have also been associated in its aetiopathogeny, such as psychiatric and neurological diseases as they contribute towards gut immobility and their treatment can lead to constipation. Dystrophies, Parkinson's disease, Alzheimer's disease and cerebrovascular events, as in the patient in our clinical case, are present in up to 40% of caecal volvulus cases.1 In addition to the aforementioned conditions, a redundant caecum with excessive mobility, due to a lack of fixation to the retroperitoneum, can predispose the patient to volvulus.1,2 Another major factor is a history of abdominal surgery, this is the case in 25–53% of patients.7 The presence of adherences contributes towards the formation of points of fixation which act as rotation axes; this usually happens with caecal bascule. The presence of a band or adhesion occluding the ascending colon and encouraging the caecum to fold up on itself,5,8 which causes a closed-loop intestinal obstruction, as it impedes anterograde emptying of the caecum, and presence of a competent ileocaecal valve, which hinders retrograde emptying. Furthermore there are gas-producing bacteria which encourage caecal distension and cause venous obstruction. If this situation is maintained over time, it results in intestinal gangrene.3–5 Retrograde emptying is sometimes possible when the ileocaecal valve is incompetent that, added to absence of mesenteric torsion, makes vascular compromise in caecal bascule rare. However, this was not the case with our patient.
Caecal bascule is a difficult condition to diagnose and its clinical manifestations are similar to those of small bowel obstruction, with the presence of continuous abdominal pain exacerbated with colicky-type pain, related to peristaltic movement. There is also an absence of intestinal transit, nausea and vomiting.
It is common to find abdominal distension with tympanism and initially increased air-fluid sounds. As the clinical manifestations progress the absence of peristalsis is common, with abdominal silence on auscultation and the onset of signs of peritoneal irritation when there is vascular compromise with gangrene or perforation.1,4
There is usually leukocytosis with left deviation and elevated acute-phase reactants. Abdominal X-ray shows the presence of air-fluid levels, with dilation of the small bowel loops. Marked distension of the caecum is visible, which is usually displaced towards the right hypochondrium, in an anteromedial position to the transverse colon.9
The absence of clinical suspicion of this condition can result in misinterpreting the radiological findings and delaying diagnosis.5 In our clinical case caecal dilation was not suspected, the dilation that was visualised was attributed to dilation of the intestinal loops. The presence of dilated small bowel loops located laterally to ectopic caecal dilation is a radiological finding which may lead us to suspect this disorder.6,7 However, radiological studies only enable diagnosis in 20% of cases.9
Barium enema can be used for diagnosis, and it is possible to achieve spontaneous reduction. However, it should not be used for diagnostic assessment in seriously ill patients.
Abdominal CT scan is the best option to achieve a definitive diagnosis, as it enables several radiological signs to be identified, specific to this condition, such as: a coffee bean or comma sign seen on axial imaging of the dilated caecum filled with air and fluid, or the bird's beak sign which is associated with the progressive tapering of the afferent and efferent loop up to the point of torsion, and is therefore less common in caecal bascule than in other types of caecal volvulus. The same occurs with the whirlpool sign associated with torsion of the mesentery and pericolic soft tissue.2,7 CT scan enables the presence of mechanical intestinal obstruction, the obstruction site, and its severity to be demonstrated. The presence of wall thickening, mesenteric fat trabeculation, intestinal pneumatosis and free fluid are usual findings when there is ischaemia.
Diagnostic colonoscopy is sometimes useful, because it also enables the viability of the mucosa to be established and can achieve devolvulation. Colonoscopy is not recommended as treatment for caecal volvuli and our case in particular, due to its poor success rate in devolvulation, recurrence being common, and the major risk of perforation.1,2,5–7
The definitive treatment is surgery, and techniques have been employed such as devolvulation with or without caecopexy. Some authors even suggest laparoscopic caecopexy. However these techniques present high recurrence rates, varying from 0 to 40% for devolvulation associated with caecopexy to 0–70% for simple devolvulation. Caecostomy presents fewer recurrences, but has a morbidity and mortality rate of 40%.6,7 Right hemicolectomy with ileotransverse anastomosis is the preferred technique,6 since recurrence has not been described after this and the morbidity and mortality rate is lower than with other techniques, although variable according to the viability of the colon: 10–15% if the colon is viable and 30–40% if gangrene is present. If the patient's general condition does not allow an anastomosis, an ileostomy should be performed. It is common during laparotomy to find a similar adhesion to that found in our patient, which crossed the ascending colon acting as a point of basculation. This adhesion can be inflammatory, congenital or most often, an adhesion related to previous surgery, as in this clinical case.
ConclusionsCaecal bascule is a rare type of caecal volvulus that causes intestinal obstruction. Its aetiology is multifactorial and can be associated with an adhesion that causes caecal distension and acts as a point of inflection, folding the caecum upwards. Its diagnosis should be suspected whenever there is ectopic caecal dilation. CT scan is the imaging technique of choice, especially in seriously ill patients. Resection and ileocolic anastomosis is the most recommended surgical option whether the colon is ischaemic or whether it is viable, because it prevents recurrence and has lower morbidity and mortality rates compared to other techniques. A high level of suspicion and early treatment are essential to prevent complications.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ruiz de la Hermosa A, Ortega-Domene P, Fuenmayor-Valera ML, Pérez-Morera A, Seoane-González JB. Báscula cecal, una causa infrecuente de obstrucción intestinal. Cir Cir. 2016;84:513–517.