Hepatocellular carcinoma originating from the caudate lobe has a worse prognosis than other hepatocellular carcinomas in another segment of the liver. An isolated caudate lobe resection of the liver represents a significant technical challenge. Caudate lobe resection can be performed along with a lobectomy, or as an isolated liver resection. There are very few reports about isolated caudate lobe liver resection. The case is reported here of a successful isolated resection of hepatocellular carcinoma in the caudate lobe with excellent long-term survival.
Clinical caseA 74 year-old female with 8cm mass lesion in the caudate lobe with no clinical or biochemical evidence of liver cirrhosis (serum alpha-foetoprotein 3.7 U/l, and negative hepatitis serology), was evaluated for surgery. A complete resection of the lesion in 270minutes, with Pringle manoeuvre for 13minutes, was satisfactorily performed. The patient was discharged ten days after surgery without complications, and is currently asymptomatic, with no deterioration of liver function and 48 months tumour-free survival after the procedure.
ConclusionIsolated caudate lobe resection is an uncommon, but technically possible procedure. In order to achieve a successful resection, detailed knowledge of complete liver anatomy is essential. Tumour free margins must be obtained to provide long survival for these patients that have a malignancy in this anatomic location.
El hepatocarcinoma originado en el lóbulo caudado tiene un peor pronóstico que otros originados en otros sitios del hígado. La resección aislada del lóbulo caudado hepático representa un reto técnico importante y puede ser realizada junto con una lobectomía hepática o una resección aislada del mismo. De esta última existen muy pocos reportes al respecto. Presentamos el caso de una resección aislada exitosa de hepatocarcinoma en el lóbulo caudado con sobrevida a largo plazo.
Caso clínicoMujer de 74 años, con lesión ocupante de 8 cm en el lóbulo caudado, sin datos clínicos o bioquímicos de cirrosis hepática, alfafetoproteína sérica 3.7 U/l, y serologías de hepatitis negativas. Resección completa de la lesión en 270 min con maniobra de Pringle por 13 min, evolución satisfactoria, y alta al décimo día posquirúrgico. Asintomática, sin deterioro de la función hepática y sobrevida sin actividad tumoral 48 meses después del procedimiento.
ConclusiónLa resección aislada del lóbulo caudado es un procedimiento infrecuente y técnicamente posible. Para realizarse de forma exitosa, se debe de tener un conocimiento detallado de la anatomía hepática completa y en especial de este lóbulo. Se deben obtener márgenes negativos tumorales para otorgar la mayor sobrevida a los pacientes que tienen una neoplasia en esta localización anatómica.
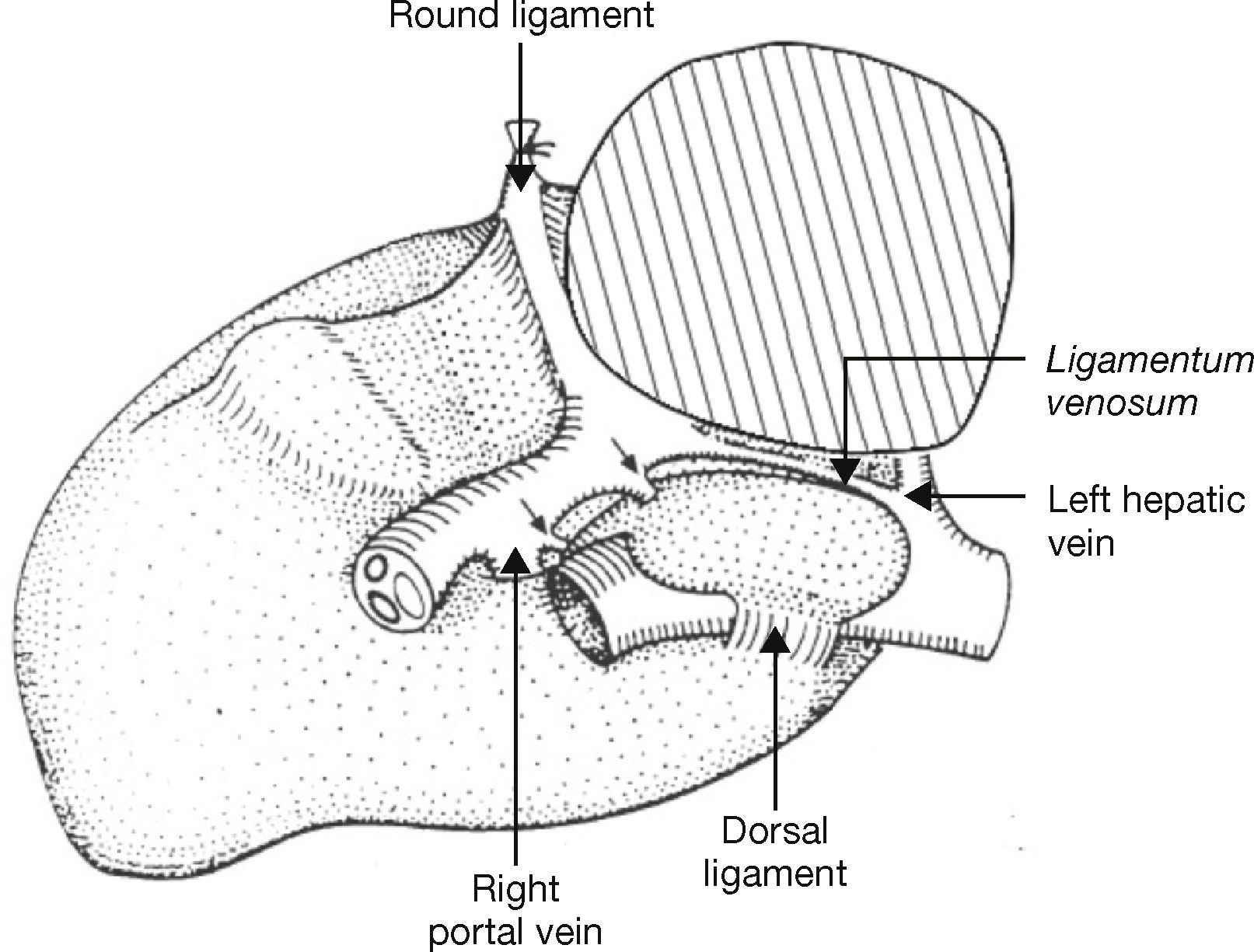
The caudate lobe (Couinaud segments I and IX) is located anterior to the inferior vena cava and can surround this structure in a circumferential pattern by means of the ligamentum venosum and the dorsal ligament. It stretches from the hepatic hilum, which is directly posterior to the bifurcation of the portal vein. In its cephalic aspect, the caudate lobe lies posterior to the conjunction of the middle and left hepatic veins, right when they drain into the inferior vena cava. The caudate lobe receives portal blood flow from both portal systems, but the greatest flow comes from the left side. Its venous drainage occurs along its posterior aspect, directly into the inferior vena cava, through multiple small branches of variable size and location. Biliary drainage includes small tributaries to the right hepatic duct, but it drains predominantly through the left hepatic duct. Arterial blood supply to the caudate lobe varies, although it mainly comes from a solitary branch from the left hepatic artery and a small posterior branch from the right sector (Fig. 1)1.
Hepatocarcinomas originating in the caudate lobe have a worse prognosis than those originating in other lobes, due to its proximity to the portal system and to the inferior vena cava, which facilitates early intrahepatic and systemic dissemination2,3. Although some surgeons have had success with transarterial embolization or local ablation performed using different methods4,5, hepatic resection is still the best surgical treatment. Resection of the caudate lobe poses a significant technical challenge. Resection of the caudate lobe can be performed as an extension of a hepatic lobectomy or as an isolated resection. From a surgical standpoint, this last option is probably the most demanding, and there are very few reports in this regard6–10.
Surgical approach for an isolated resection of the caudate lobe can be through a bilateral subcostal incision, or a midline incision if the patient had a previous surgery. Peritoneal metastases should always be ruled out and the entire liver should be examined through an intraoperative ultrasonography. A cholecystectomy may be performed, depending on the findings or in case of a pathology. Once it has been determined that an isolated caudate lobe resection must be performed, the gastrohepatic ligament must be opened and the ligamentum venosum must be dissected at the root of the left hepatic vein, which is facilitated by the anterior retraction of the left lateral segment of the liver. Some authors recommend a complete liver mobilisation prior to this step to have greater vascular control over the inferior vena cava in case of severe haemorrhage or if a reconstruction of it must be carried out1,8,9. The dorsal ligament is then dissected to fully mobilise the caudate lobe and expose the hepatic veins that run directly from it to the anterior surface of the inferior vena cava, for subsequent ligation. There are one to three veins of significant size, and multiple small veins. After the division of these veins, the caudate lobe is more mobile and can be retracted to the left, to better expose the left portal branch. At this point, the branches coming from the hepatic artery and the right portal branch can be distinguished and secured via ligation or nonabsorbable fine monofilament sutures6.
Liver parenchymal transection can be performed using different techniques (ultrasonic dissection, hydrojet and/or finger fracture with haemostasis using Kelly clamps) to separate the caudate lobe from the posterior side of the right hepatic lobe. The Pringle manoeuvre (occlusion of the hepatoduodenal ligament with interruption of blood flow in the hepatic artery and portal vein) and/or specific vascular control can be used. Bleeding can be controlled with absorbable monofilament sutures; the use of drainage will depend on what the surgeon determines. Although the technique above is the most common technique to perform an isolated resection of the caudate lobe, there are others, such as the anterior hepatic transection and right lateral surgical approaches to the liver7–9.
The objective of this study is to present the case of an isolated resection of the caudate lobe secondary to a hepatocarcinoma resulting in a 48-month survival, placing an emphasis on the surgical technique and the relatively low incidence of a hepatocarcinoma originating exclusively in the caudate lobe.
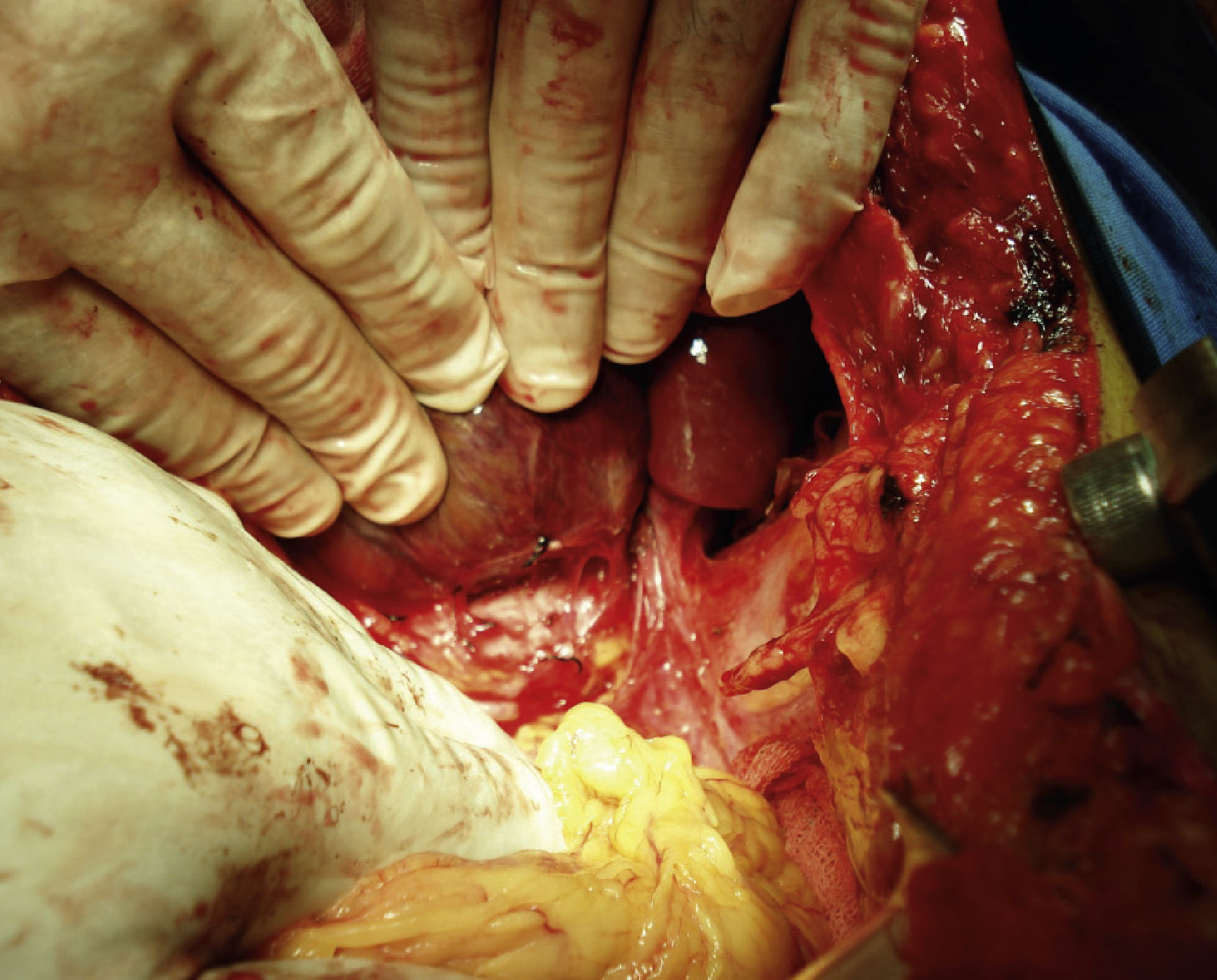
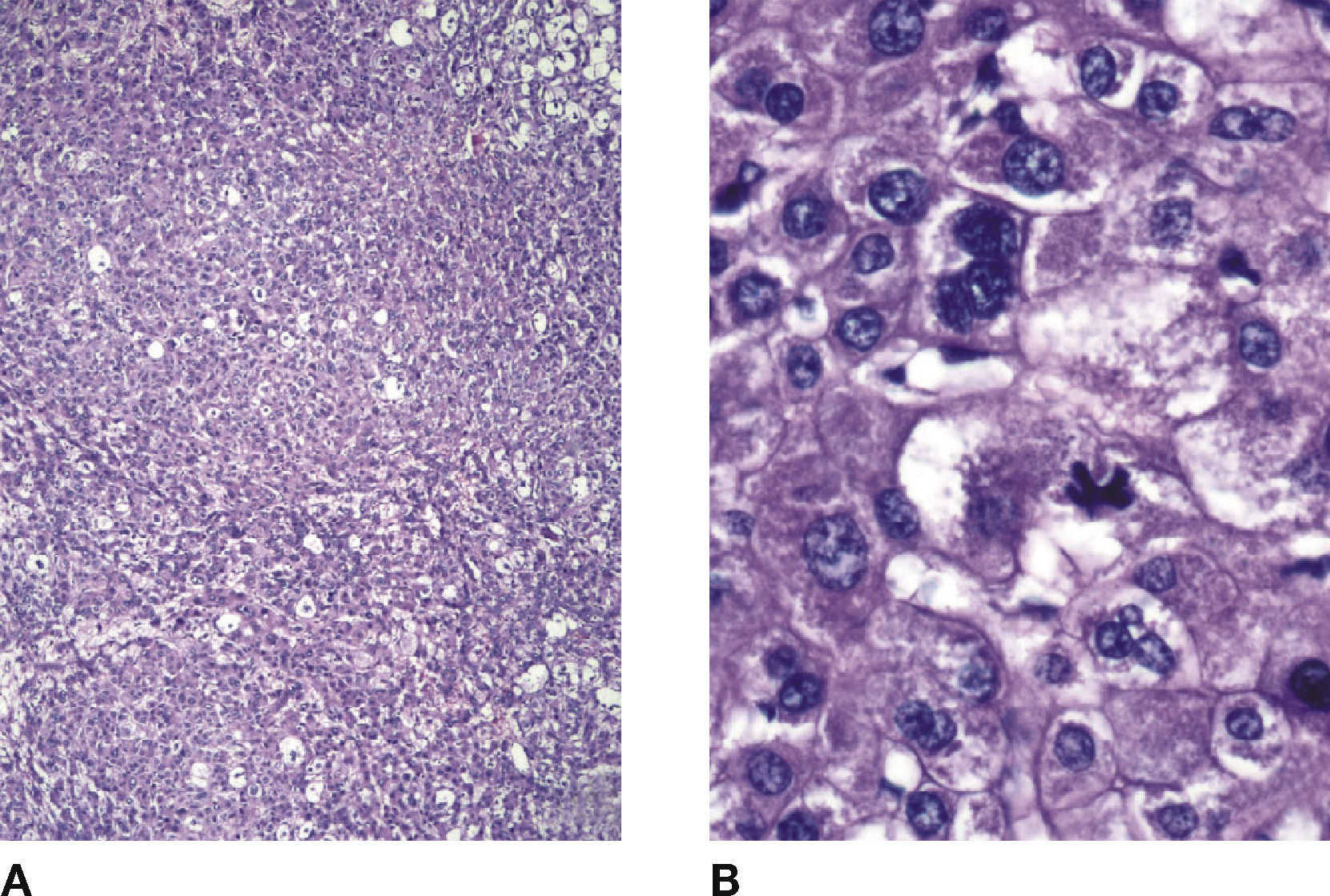
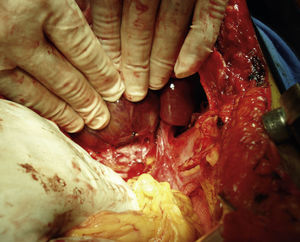
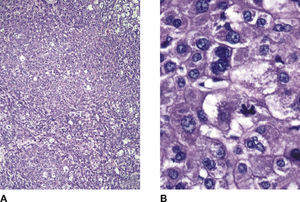
Clinical casePatient is a 74-year-old female who has been diabetic for 11 years. She is undergoing treatment with oral hypoglycemiants. She has an 8 cm lesion in the maximum diameter located in the caudate lobe, diagnosed by CT scan (Fig. 2). There are no clinical or biochemical data showing signs of hepatic cirrhosis (no signs of ascitis and encephalopathy, albumin 4.1 g/dl, total bilirubin 1.4 mg/dl, prothrombin time test 10.9, INR 0.93, platelets 228×103 cell/mm3) and serum alpha-fetoprotein 3.7 UI/l. Hepatic serology for hepatitis A, B and C was negative. She underwent exploratory laparotomy via a bilateral subcostal approach with intraoperative ultrasound. No other hepatic lesions were found. A complete resection of the lesion was performed, which lasted 270 minutes. Finger fracture and haemostasis with Kelly clamps were used, performing Pringle manoeuvre during 13minutes, with complete liver mobilization to expose the infrahepatic inferior vena cava prior mobilization of the tumour in the caudate lobe. There was also exposure of the hepatic veins that run directly into the anterior surface of the inferior vena cava to ligate them by means of retracting the liver anteriorly and executing close suction drainage of the surgical bed. Intraoperative bleeding was 3,000 ml and seven units of packed red cells were transfused (Figs. 3 and 4). Satisfactory postoperative evolution. Discharged ten days after surgery. The histological aspect of the lesion corresponds to a moderately differentiated hepatocarcinoma with solid pattern (haematoxylin and eosin, 5×). Neoplastic cells are large, polygonal with pleomorphic nuclei, with nucleoli, multinucleation and tetrapolar mitosis (haematoxylin and eosin, 40×) (Fig. 5 A and B). A negative margin of 4 mm was achieved.
Patient is asymptomatic, without deterioration of liver functions and shows no signs of tumour activity 48 months after the procedure.
DiscussionIsolated caudate lobe resection is a technically demanding procedure, since surgical access is complex due to the location. In large centres, isolated caudate lobe resections do not exceed 4% of the total amount of liver resections, and mortality rates as a result of this surgery can range from 5% to 14%3,8. Different techniques have been described for isolated caudate lobe resections, which have been defined and classified6. Three of these techniques include resections from other liver segments and only one refers to the isolated resection of it. The first approach involves resection of adjacent segments II and III, or II, III and IV7,8. The second approach involves total right hepatectomy, together with the caudate lobe. The third approach is central or transhepatic, which involves resection of segment IV and of the caudate lobe9. The last one is the left lateral approach (anteriorly), which is the one we used in this case. To determine the type of surgical approach, the magnitude of the disease and the degree of liver failure must also be taken into account. In patients with sufficient liver function, caudate lobe resection can be performed anatomically, together with adjacent segments. In the case of patients with decreased liver function (including cirrhosis), a partial resection of the caudate lobe following the portal triad, can be performed by ligation of portal branches that drain into the caudate lobe to generate a demarcation in order to identify the area to be resected8. In our case, we decided to perform an isolated caudate lobe resection, since the lesion was located exclusively there and, despite the fact that according to laboratory data the patient had sufficient liver function, we contemplated performing the least resection of liver tissue possible.
There are very few series of isolated caudate lobe resections in medical literature. Sarmiento et al.6 published a series of 19 isolated caudate lobe resections in patients with an average age of 52, caused by several disorders, where only two were secondary to hepatocarcinoma. The average operating room time was 211 minutes, with a level of blood loss of 760 ml, an average hospital stay of seven days, a morbility rate of 5%, and no mortality. Yamamoto et al.7 published a series of 402 hepatocarcinomas, where only 13 (3.2%) were isolated caudate lobe resections. There was no perioperative mortality and the survival rate was similar to that of other hepatocarcinomas, except where there was microscopic invasion of the portal system. Other authors have published series of 150 caudate lobe resections secondary to several disorders (hepatocarcinoma, 10% of the total), where only 14% (n=21) were isolated caudate lobe resections. Median tumour size was of 2.7 cm, average operating room time was 220 minutes, level of blood loss was 600 ml and average hospital stay was seven days, with no mortality8. Lastly, the largest series of hepatocarcinomas with isolated caudate lobe resection has been described by Liu et al.10 with no perioperative morbility or mortality, and the survival rate for five years after surgery was of 31.8%. The presence of cirrhosis, a subsegmental location of the lesion, a tumour free margin<5 mm and vascular invasion were associated with a worst prognosis. Our case involves a large hepatocarcinoma (8 cm), confined only to the caudate lobe, which is why it was possible to perform the isolated resection in a timeframe and with a hospital stay similar to the cases described. Additionally, the fact that our patient did not have cirrhosis, that we achieved negative tumour margins and because of the absence of vascular invasion, both in the portal system and in the inferior vena cava, has contributed to her survival, without signs of recurrent tumour activity.
ConclusionIsolated caudate lobe resection is a rare procedure, which is technically possible. To successfully perform it, detailed knowledge of the entire liver anatomy is crucial, and particularly of this lobe. Negative tumour margins must be achieved to offer a higher survival rate to patients with neoplasias in this anatomical location.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: G. Martínez-Mier et al. Hepatocarcinoma originado en el lóbulo caudado. Estrategia quirúrgica para su resección. A propósito de un caso. Cirugía y Cirujanos. 2015; 83: 51-55.