Hip and knee prosthetic replacements have proven to be the most appropriate treatment in the joints that do not benefit from medical or arthroscopic interventions; however, infections are the most feared complication. It is recommended that the incidence of infection should not exceed 2%.
Material and methodsThis was an observational, prospective, longitudinal and observational study conducted in patients fitted with a prosthetic joint from August 2011 to July 2012. Patients were followed up pre and post-surgery for one year to identify a prosthetic infection, diagnosed using international parameters. We calculated the incidence of prosthetic infection, as well as the incidence density.
ResultsA total of 339 patients (179 hip and 160 knee) were included. Variations in the time of pre-operative antibiotics’ administration were observed. Six prosthetic infections were identified with an incidence rate of 1.79/339 arthroplasties, 2.2/179 hip procedures, and 1.25/160 knee arthroplasties. An incidence density of 0.02/year for hip arthroplasties and 0.11/year for knee procedures was identified. There were 4 infections of hip and 2 of knee. Five infections were acute and one chronic. The isolated microorganisms were Enterococcus faecalis, Staphylococcus epidermidis (2), Streptococcus mitis, Staphylococcus aureus and Pasteurella stomatis.
ConclusionsThe incidence of prosthetic joint infection in the first year of follow-up at our centre is within the recommended parameters. Surgical techniques and organisational practices influence the results.
Las artroplastias de cadera y rodilla han demostrado ser el tratamiento óptimo para las articulaciones que no se benefician de intervenciones médicas o artroscópicas; sin embargo, la infección de la prótesis articular es la complicación más temida. Se estima que la incidencia de las infecciones no debe exceder del 2%.
Material y métodosSe llevó a cabo un estudio observacional, longitudinal, prospectivo en pacientes tratados mediante prótesis articular de agosto de 2011 a julio de 2012. Se les realizó un seguimiento pre- y posquirúrgico anual para identificar un proceso infeccioso articular. Se reconocieron las infecciones de prótesis utilizando los estándares internacionales acostumbrados. Se calculó la incidencia de infecciones de prótesis, así como la densidad de incidencia.
ResultadosSe incluyó a 339 pacientes (179 de cadera y 160 de rodilla). Se observaron alteraciones en la hora de aplicación de antibióticos preoperatorios. Se identificaron 6 infecciones protésicas, con una tasa de incidencia de 1.79/339 artroplastias, de 2.2/179 para cadera y de 1.25/160 para rodilla. Una densidad de incidencia de 0.02/año para cadera y de 0.11/año para rodilla. Hubo 4 infecciones de cadera y 2 de rodilla, 5 de ellas infecciones agudas y una crónica. Los microorganismos aislados fueron E. faecalis, S. epidermidis (2), S. mitis, S. aureus y P. stomatis.
ConclusionesLa incidencia de infección de prótesis articular de cadera y rodilla en nuestro centro está dentro de los parámetros recomendados dentro del primer año de seguimiento. Las prácticas organizacionales y técnicas quirúrgicas influyen en los buenos resultados.
Arthroplasties have been demonstrated to be the most effective treatment for patients with serious joint disease or end-stage joints.1 The indication for the procedure depends on the functional impact and pain caused by joint degeneration and, moreover, on the quality of the reconstruction expected and its maintenance over time.2 The number of primary total knee and hip arthroplasties has increased over the past decade, as shown in a study in the United States, with almost 800,000 procedures in 2006.3 This type of treatment is considered to have a survival rate from 10 to 23 years for 75–98% of the procedures, and therefore is considered appropriate treatment to reduce pain and promote functionality.4
The causes of failure include aseptic weakening, infection, dislocation and fracture of the bone or prosthesis. The frequency of infection has been observed to increased in relation to the number of primary arthroplasties.5 Infection, although rare, is the most serious complication: it occurs in 0.8–1.9% of knee arthroplasties and in 0.3–1.7% of hip arthroplasties.6 Mexican data from retrospective studies over a period of 5–10 years report from 3.7% to 4.3%, respectively, in knee arthroplasties.7,8
Various risk factors have been identified associated with the infectious process, such as: revision arthroscopy, previous infection associated with a prosthesis in the same site, smoking, obesity, rheumatoid arthritis, cancer, immunosuppression and diabetes mellitus. And finally, postoperative factors such as surgical wound complications (for example, superficial infection, haematoma, necrosis and wound dehiscence), atrial fibrillation, myocardial infarction, urinary tract infection, prolonged hospital stay, and Staphylococcus aureus bacteriaemia.9–13
Often skin bacteria are inoculated into the implant; however, in some cases, microorganisms infect the prosthesis by haematogenous spread or through local compromised tissues. Infections associated with joint prostheses can be classified as early (within the first 3 months following surgery) or delayed (from 3 to 24 months postoperatively).14 It is vitally important to diagnose a prosthetic infection. However, this is challenging for many reasons: pathogenic bacteria of less virulence, the pathogenesis and response of the patient. Although there is no universally accepted definition for this type of infection, a consensus has been recently formulated to standardise diagnostic behaviours.15 The treatment of prosthetic infections is usually both medical and surgical. The time and type of treatment depends on the cause, time of infection and the condition of the host. Since multiple surgical treatments are required and prolonged medical treatment, the cost of this disease can exceed 50,000 dollars when sensitive microorganisms are involved, and 100,000 dollars with resistant microorganisms.16
Since there are no national data on the incidence of infectious complications of these types of joint procedures, by means of strict follow-up of patients and a well-established diagnosis, the objective of this study was to determine the incidence and the risk factors associated with primary hip and knee prosthetic infections.
Material and methodsAll the patients aged over 18 years who underwent placement of a primary hip or knee prosthesis in the hip and knee reconstruction department of the Instituto Nacional de Rehabilitación during the period 1 August 2011–31 July 2012.
General information on the patients was taken from their assessment and follow-up period. During their hospitalisation, data were gathered that might have been implicated in the development of infection. The patients were followed up with visits after their discharge from hospital at 15, 30, 90, 180 and 360 days. An intentional search was carried out for erythema, oedema, hyperthermia, pain or secretion from the surgical wound.
In the event that the patients had not attended one of their follow-up sessions, they were contacted by telephone to assess their progress, and the cases with the possibility of infection were advised to attend an assessment.
Primary hip or knee prosthetic infection was defined according to the latest international consensus,15 with the following criteria:
- 1.
Isolation of the same microorganism in 2 periprosthetic cultures, or
- 2.
A tract communicating between the prosthesis and the outside (fistula), or
- 3.
The presence of at least 3 of the following criteria:
- a)
Elevated C reactive protein and erythrocyte sedimentation rate,
- b)
Elevated leucocyte count or positive leucocyte esterase in synovial fluid,
- c)
Elevated polymorphonuclear neutrophil count in synovial fluid,
- d)
Positive biopsy for periprosthetic tissue infection or,
- e)
Positive periprosthetic tissue culture.
An infectious disease specialist was included at all times in the assessment of the cases. If a prosthetic infection process was identified, treatment was given according to the clinical presentation of each patient and as stipulated in the department's clinical guidelines, with microbiological isolation of each case.
Statistical analysisDescriptive analysis of the data was performed using measures of central tendency and dispersion (mean±deviation; median and minimum–maximum values) for the quantitative variables (continual or dimensional), in which initially the normality of the distribution used was evaluated using bias and kurtosis indicators. Absolute and relative frequencies (percentages) were used for the qualitative variables. The cumulative incidence and density of incidence were calculated.
Ethical considerationsThe protocol was assessed and approved by the Research Committee of the Instituto Nacional de Rehabilitación with number 22/12.
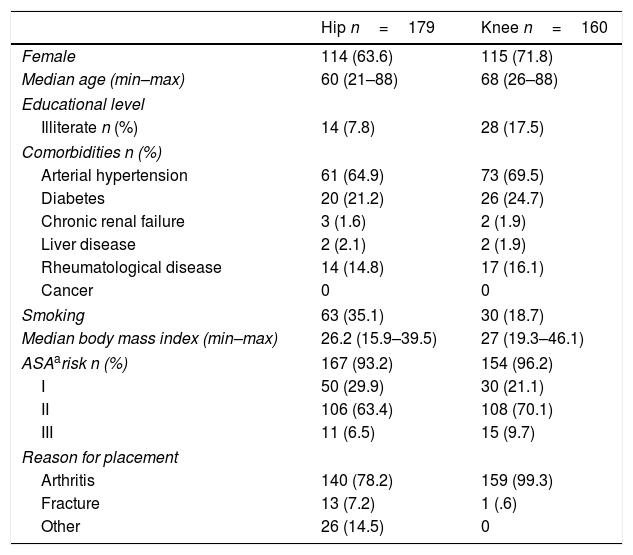
ResultsFrom the period between August 2011 and July 2012, 339 patients with primary arthroplasties of the hip and knee were included, who underwent 179 to 160 procedures, respectively. One hundred and fourteen (63.6%) hip prostheses were placed and 115 (71.8%) knee prostheses in females. Hip arthroplasty was performed more often in younger patients than knee arthroplasty, with a median of 60 years. In terms of educational level, those who underwent hip arthroplasty more often were educated to intermediate or higher level and higher level compared to those who underwent arthroplasty of the knee (116 vs 64). Of the foreign patients included in the cohort, 22.3% underwent arthroplasty of the hip and 21.8% of the knee.
In terms of history, 94 (52.5%) hip and 105 knee (65%) patients presented comorbidities; high blood pressure and diabetes mellitus predominated. Patients with rheumatoid disease underwent knee arthroplasties more frequently. Thirty-five percent of the hip patients were active smokers compared to 18.7% of the knee patients. There were more patients with surgical risk ii or greater according to the American Society of Anaesthesiologists (ASA) among those who underwent knee than those who underwent hip arthroplasty (79.8 vs 69.9%).
There was a mean body mass index of below 30 in both procedures.
The principal cause for prosthesis placement was arthrosis. We observed that there were other causes for the patients with hip arthroplasties; the most frequent was fracture and its sequelae (18; 10%), as well as congenital hip dysplasia (10; 5.5%) (Table 1).
Demographic variables of the patients.
| Hip n=179 | Knee n=160 | |
|---|---|---|
| Female | 114 (63.6) | 115 (71.8) |
| Median age (min–max) | 60 (21–88) | 68 (26–88) |
| Educational level | ||
| Illiterate n (%) | 14 (7.8) | 28 (17.5) |
| Comorbidities n (%) | ||
| Arterial hypertension | 61 (64.9) | 73 (69.5) |
| Diabetes | 20 (21.2) | 26 (24.7) |
| Chronic renal failure | 3 (1.6) | 2 (1.9) |
| Liver disease | 2 (2.1) | 2 (1.9) |
| Rheumatological disease | 14 (14.8) | 17 (16.1) |
| Cancer | 0 | 0 |
| Smoking | 63 (35.1) | 30 (18.7) |
| Median body mass index (min–max) | 26.2 (15.9–39.5) | 27 (19.3–46.1) |
| ASAarisk n (%) | 167 (93.2) | 154 (96.2) |
| I | 50 (29.9) | 30 (21.1) |
| II | 106 (63.4) | 108 (70.1) |
| III | 11 (6.5) | 15 (9.7) |
| Reason for placement | ||
| Arthritis | 140 (78.2) | 159 (99.3) |
| Fracture | 13 (7.2) | 1 (.6) |
| Other | 26 (14.5) | 0 |
Antibiotic prophylaxis was given before surgery for 153 (93.8%) hip and for 125 (89.2%) knee patients. The main drug used was a first generation cephalosporin (cephalotin); the patients who were allergic to penicillin were given levofloxacin for prophylaxis. The median administration time of antibiotic prophylaxis was 93min (9–300) for the hip and 78min (1–315) for the knee, before the start of surgery. The median postsurgical duration of said antibiotic was 12 days. The patients who underwent hip arthroplasties received more transfusions than those who underwent knee arthroplasty, who most often suffered hypothermia and more incidents during the surgery. The hospital stay was a median of 6 days (4–22) for the hip and 4 days (3.12) for the knee. Twenty visits were recorded to the emergency department by the hip patients, of which 10 (5.5%) were associated with the surgery, such as dislocation, trauma, surgical wound condition and others.
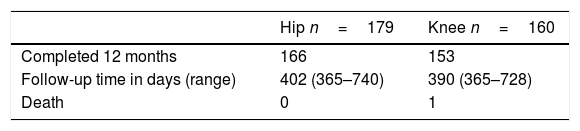
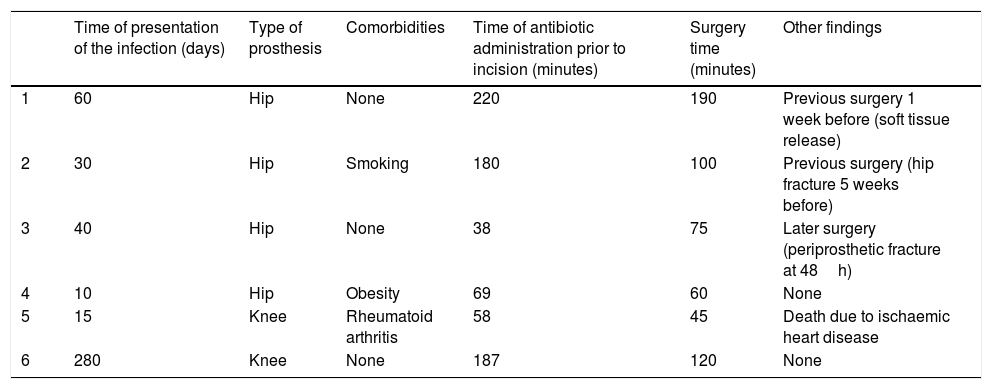
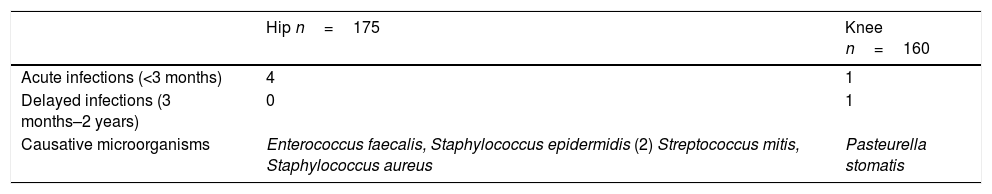
Two patients had surgical wound infection after hip arthroplasty and 3 patients after knee arthroplasty. It was possible to record the complete progress of 166 (92.7%) patients who underwent hip arthroplasty and 153 (95.6%) who underwent knee arthroplasties over one year's follow-up; with a median total follow-up of 402 days (365–740) and 390 days (365–728), respectively. Twenty censorings were obtained. Follow-up after discharge from hospital is described in Table 2. Infection developed in the prostheses of 6 patients, 4 hip and 2 knee, which are described in detail in Table 3. In the 5 (83%) patients with infection, the infection occurred during the acute period. Table 4 shows the microorganisms involved. The other infections that it was possible to document were 5 surgical wound infections and one urinary tract infection that was complicated with bacteriaemia.
Description of the relevant characteristics associated with the infectious process in the 6 patients with prosthetic infection.
| Time of presentation of the infection (days) | Type of prosthesis | Comorbidities | Time of antibiotic administration prior to incision (minutes) | Surgery time (minutes) | Other findings | |
|---|---|---|---|---|---|---|
| 1 | 60 | Hip | None | 220 | 190 | Previous surgery 1 week before (soft tissue release) |
| 2 | 30 | Hip | Smoking | 180 | 100 | Previous surgery (hip fracture 5 weeks before) |
| 3 | 40 | Hip | None | 38 | 75 | Later surgery (periprosthetic fracture at 48h) |
| 4 | 10 | Hip | Obesity | 69 | 60 | None |
| 5 | 15 | Knee | Rheumatoid arthritis | 58 | 45 | Death due to ischaemic heart disease |
| 6 | 280 | Knee | None | 187 | 120 | None |
Types of prosthetic infections and microorganisms involved.
| Hip n=175 | Knee n=160 | |
|---|---|---|
| Acute infections (<3 months) | 4 | 1 |
| Delayed infections (3 months–2 years) | 0 | 1 |
| Causative microorganisms | Enterococcus faecalis, Staphylococcus epidermidis (2) Streptococcus mitis, Staphylococcus aureus | Pasteurella stomatis |
The general cumulative incidence of prosthetic infection was 1.79/339 (CI 0.3–2.3%); for hip 2.2/179 (CI 0.5–2.5%) and for knee arthroplasty 1.25/160 (CI 0–2%).
The density of incidence was 0.02/year for hip arthroplasties and 0.011/year for knee arthroplasties.
DiscussionJoint wear causes pain and dysfunction long term, which affects quality of life. When conservative treatment fails to relieve hip or knee joint pain or dysfunction, total arthroplasty is indicated. This is an elective procedure that can considerably improve pain and function.17–19 More than 168,000 hip and more than 267,000 knee arthroplasties are performed annually in the United States and it is expected that 571,000 hip arthroplasties will be performed by 2030 according to projections.20 Improved surgical techniques, reduced operating time and prophylactic antibiotics have reduced the (infection) incidence to 1–2%.5 Using the data from patients hospitalised nationally in the United States, Kurtz et al.21 found an incidence (of infection) ranging between 2.0% and 2.4% of total arthroplasties of the hip and knee respectively.21 Participation by hospitals in the nosocomial infections surveillance system (NNIS) in the United States is voluntary, therefore the data in this system might have selection bias: the NNIS index might not ensure appropriate stratification of this type of surgery's risk of infection.1 Data from other studies performed in individual hospitals have shown very varied gross incidences of surgical infection after the implantation of prostheses, between 1.25% and 8.2%.22,23
The information reported in Latin American hospitals is scarce. In Chile, a report from 2007 showed a 2.5% incidence in a period of 5 years for hip arthroplasties.24 A report from Brazil mentions 34 infected knee prostheses over a year in a 150 active-bed hospital, however, they did not specify the amount of procedures undertaken in a year.25 There are only reports of retrospective studies in Mexico with joint infection figures from 4.2% to 8.4%7,26 in the Instituto Nacional de Rehabilitación and in the Mexican Social Security Institute, respectively, which do not provide a complete overview of what is happening in Mexico, even though the studies were performed in 2 high speciality centres in our country, with wide experience in prosthesis placement. Therefore, creating a cohort enables long term follow up of the cases included, which offers a broader view of the presentation time and possible factors that might influence a disease presenting in an institution and enable an evaluation of its applicability to other areas of our country.27
In this study we observed that the general cumulative incidence for both procedures during the first year of follow-up in these patients is below 2%: very much below that reported by other Latin American hospitals and very similar to those reported by hospitals in the United States. However, it is slightly more for hip procedures. Acute prosthetic infections were the most frequently encountered in terms of time of presentation at 83%. Reports from other series show that the clinical presentation of infections can vary according to the classification (acute or chronic), since some reports used the classification by Tsukuyama et al.28 and others that of Del Pozo et al.,29 which makes accurate comparison in terms of time of presentation impossible.
Different microorganisms were found in this study that were integral to the normal skin flora as well as from the digestive tract, even with no history of gastroenterological infection in the period during which the infection was diagnosed, and therefore there might well have been a wound infection due to faecal contamination. The case of prosthetic infection by Pasteurella stomatis had no history of living with animals, and it was not possible to assess the likely entry route of the microorganism. On assessment of the history of the patients with acute hip infections, 50% had been treated by previous surgical procedures or after the prosthesis placement, therefore having had previous surgery or later manipulation might have influenced development of the periprosthetic infection. It was observed in another study that hip prosthesis infections are associated with the presence of haematoma due to a previous neck of femur fracture.30 However, prostheses were indicated in our study due to chronic arthropathy rather than fractures secondary to trauma.
It is striking that the antibiotic administration time was disproportionate in most of the patients, compared to that routinely recommended, since preoperative antibiotic prophylaxis should be given within 30–60min before beginning the surgical incision31–34 and the antibiotic of choice should be a first or second generation cephalosporin.34–37 It is poor practice to leave the responsibility to the anaesthetist, since they cannot achieve optimal administration as they receive and assess patients for anaesthesia. Therefore, we suggest that it should be given when the patient enters the operating room, and thus ensure the necessary time for the drug to reach a good concentration in the tissues. In order to ensure the appropriate concentration of the antimicrobial agent, both in serum and tissue, it is recommended to repeat the intraoperative dose for procedures that exceed 2 half-lives of the drug, or for procedures with excessive blood loss (1500ml).38 In general, repeating the antimicrobial dose after wound closure is not necessary and might increase antimicrobial resistance selection.39–43 In a systematic review of randomised trials, there was no difference in the surgical wound infection rate in patients who received a single dose of antibiotic compared to multiple dose regimens, given for less or more than 24h (OR 1.04, of 95%: .86–1.25). Therefore, giving antibiotics for longer than 24h is not necessary, as observed in this study where the patients received postoperative antibiotics for a median of 12 days.40
Comorbidities presented in half the patients treated with surgical procedures; arterial hypertension was the most frequently reported. It is striking that the great majority of the patients did not apparently have immunosuppressive disease, which might be a benefit for this cohort. However, it might be that there were patients in this series with systemic rheumatological diseases predominating in the joints and with little expression in other organs.
One death was documented, that was not associated with the infectious process, since it was secondary to an acute myocardial infarction. In this regard, Aynardi et al.44 observed in a retrospective study that .46% of the patients treated in one of 8261 hip arthroplasty procedures died within 90 days and that the main cause of death was cardiovascular in 32% and, of these, 26% were secondary to a myocardial infarction. Therefore appropriate preoperative assessment is recommended to identify the cardiovascular risk factors.44 This was undertaken in the Instituto Nacional de Rehabilitación, although not systematically, since the patients might have brought assessments from other care centres, and therefore the assessment was not homogeneous.
It can be seen that the infection rate in both procedures is within that recommended by the international standards, which is due to the good organisation programme of the hip and knee joint reconstruction department, which has been perfected over time, since patients are comprehensively assessed and the procedure is considered purely elective surgery that is not performed if there is any potential risk for the patients. It is always ensured that all the material is ready prior to commencing the procedure; if not, the surgery does not go ahead. It is important to mention that the staff who participate directly in the operation are experienced and that an attending physician is present; this ensures that the procedure is undertaken safely and appropriately.
The infections found were treated with debridement and antibiotic therapy targeted towards microbiological isolation and no prosthesis has had to be removed in the follow-up period to date.
The treatment of prosthetic infections is complex and requires strict collaboration between orthopaedic surgeons and infectious disease specialists.45 Protocolising the clinical treatment of this disease and undertaking clinical trials is made difficult due to the great variation in clinical circumstances, the difficulty in gathering sufficiently numerous series, and the need for prolonged follow-up. Beyond selected case series, we have few data on how prosthetic infections are treated overall in our country.7,8 Therefore studies are required on medical personnel's knowledge of this disease.
This is the first prospective study undertaken in a specialist prosthesis placement centre in Mexico with encouraging results. The results of this study offer an overall view of hip and knee prosthesis infections in our hospital, by analysing epidemiological aspects, risk factors, clinical presentation and the therapeutic treatment of cases, and providing an outline of the facts of the problem.
ConclusionsThe incidence of hip and knee joint prosthesis infection in the Instituto Nacional de Rehabilitación is within the recommended parameters in the first year of follow-up. The organisational practice and surgical techniques influence the good results obtained.
FundingThis manuscript had no source of financing.
Conflict of interestThe authors have no conflict of interest to declare.
We would like to give special thanks to the orthopaedic residents and nursing staff who participated directly and indirectly in this study, and the chemists and technicians from the infectious disease laboratory and Lic. Alicia Camacho for her unconditional administrative support.
Please cite this article as: Franco-Cendejas R, Contreras-Córdova EL, Mondragón-Eguiluz JA, Vanegas-Rodríguez ES, Ilizaliturri-Sánchez VM, Galindo-Fraga A. Incidencia de infecciones protésicas primarias de cadera y rodilla en un centro de la Ciudad de México. Cir Cir. 2017;85:485–492.