Small bowel volvulus is a rare cause of intestinal obstruction in adult patients. This disease is more common in children and its etiology and management is different to that in adults.
Clinical caseA 30 year-old male with sarcoidosis presents with acute abdomen and clinical data of intestinal obstruction. Small bowel volvulus is diagnosed by a contrast abdominal tomography and an exploratory laparotomy is performed with devolvulation and no intestinal resection. In the days following surgery, he developed a recurrent small bowel volvulus, which was again managed with surgery, but without intestinal resection. Medical treatment for sarcoidosis was started, and with his clinical progress being satisfactory, he was discharged to home.
ConclusionsMaking an early and correct diagnosis of small bowel volvulus prevents large intestinal resections. Many surgical procedures have been described with a high rate of complications. Therefore, conservative surgical management (no intestinal resection) is recommended as the best treatment with the lowest morbidity and mortality rate.
El vólvulo de intestino delgado representa una causa poco frecuente de oclusión intestinal en el paciente adulto. Esta patología es más frecuente en niños debido a su etiología, y el manejo suele ser diferente en el paciente adulto.
Caso clínicoMasculino de 30 años de edad, con antecedente de sarcoidosis, que acude a urgencias con abdomen agudo y datos clínicos de oclusión intestinal. Se realizó el diagnóstico de vólvulo de intestino delgado por tomografía helicoidal contrastada y se procedió a realizar laparotomía exploradora, se devolvula sin resección intestinal. Durante el postoperatorio cursó con íleo postquirúrgico tardío, recurriendo el vólvulo, por lo que se sometió a nueva devolvulación sin resección; se inició tratamiento médico para sarcoidosis por sospecha de actividad de esta última. La evolución del paciente fue satisfactoria, por lo que se egresó.
ConclusionesPara evitar resecciones intestinales amplias en casos de vólvulo de intestino delgado se debe establecer el diagnóstico temprano y reducir el vólvulo para restablecer el flujo sanguíneo. Se han descrito múltiples procedimientos quirúrgicos con alta tasa de complicaciones, por lo que consideramos que el tratamiento conservador quirúrgico sin resección intestinal, en la actualidad conlleva menor morbimortalidad.
Small bowel volvulus is a rare condition, and represents only 0.5–2.5% of intestinal obstruction in adult patients. The clinical presentation is that of an acute abdomen.1 Small bowel volvulus refers to an abnormal twisting of a loop of bowel around its own mesentery, leading to mechanical obstruction of the intestine. Mesenteric torsion also leads to occlusion of the mesenteric vasculature with intestinal ischemia, and finally necrosis.2 The mortality rate is between 9% and 35%, depending on the reference consulted, and although Roggo and Ottinger1 document a 0% mortality rate provided the intestine is viable, rates may increase from 20% to 100% when underlying intestinal necrosis is present.3,4
Depending on its etiology, we can divide small bowel volvulus into primary and secondary types.5 Primary volvulus occurs in abdominal cavities where there is no predisposing anatomical defect. This presents with greater frequency in Africa, India and Middle Eastern countries, with an annual rate of 24–60 cases per 100,000 inhabitants. High incidence rates are attributed to food habits, where it is standard practice to ingest large amounts of foods with high fiber content, after prolonged periods of fasting.6,7
Secondary small bowel volvulus, however, occurs in the presence of predisposing injuries, whether congenital or acquired; these include: malrotations, bands and adhesions, among others.8 It is important to point out that small bowel volvulus is not synonymous with intestinal malrotation, since there are no anatomical changes in intestinal and mesenteric adhesions.
Although surgery is always indicated in this case, there are no existing guidelines to establish what the treatment of choice would be. For this reason we put forward a case of recurrent small bowel volvulus in a patient with sarcoidosis and the review of surgical treatment.
Clinical caseA 30 year-old male who presented at the emergency unit with a 24-h history of general cramping abdominal pain, together with nausea, and vomiting with contents from the stomach and bile. He was a smoker who had been diagnosed with sarcoidosis in 2006 and was administered treatment based on metrotrexate and corticosteriods which had been suspended 3 weeks prior to hospital admittance. He had undergone several ophthalmologic operations for bilateral retinal detachment, cholycystectomy and pyloroplasty as a newborn.
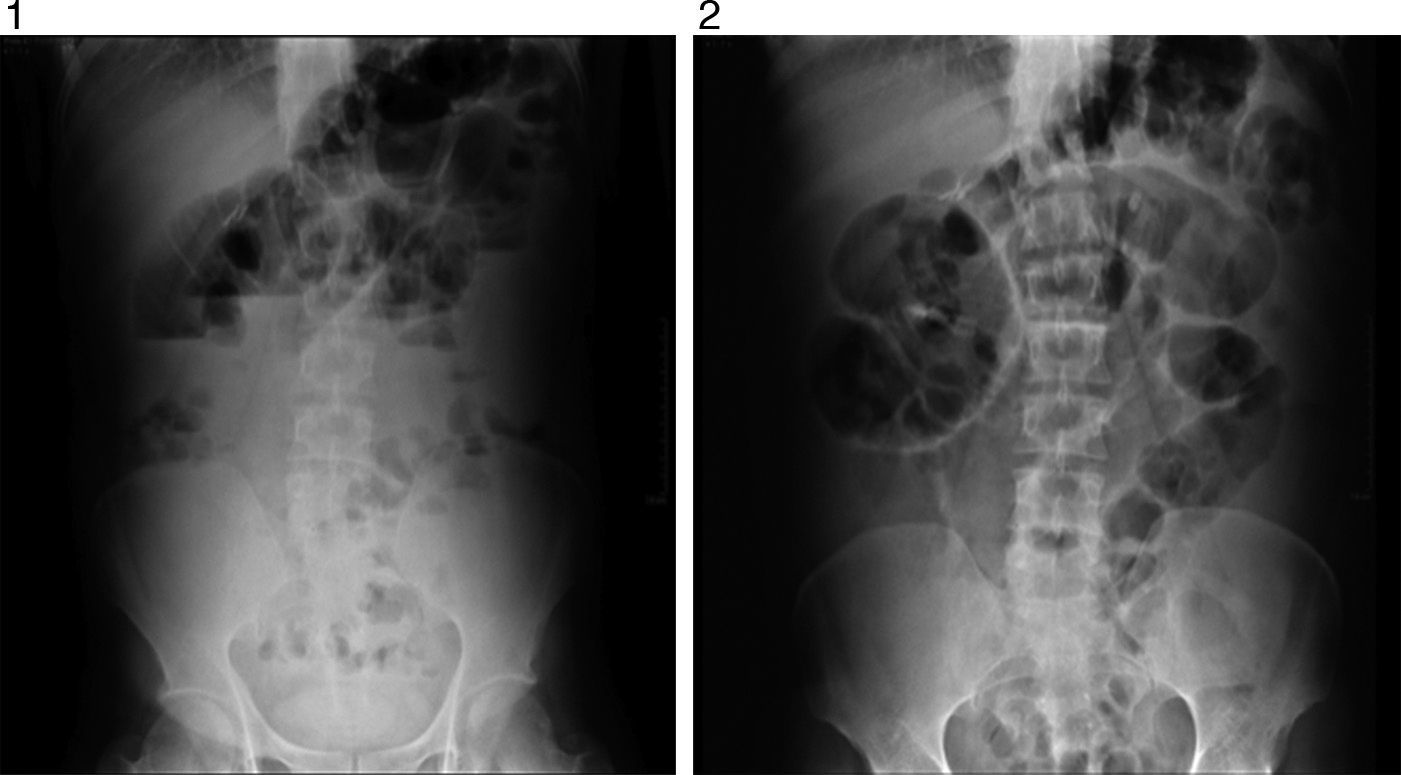
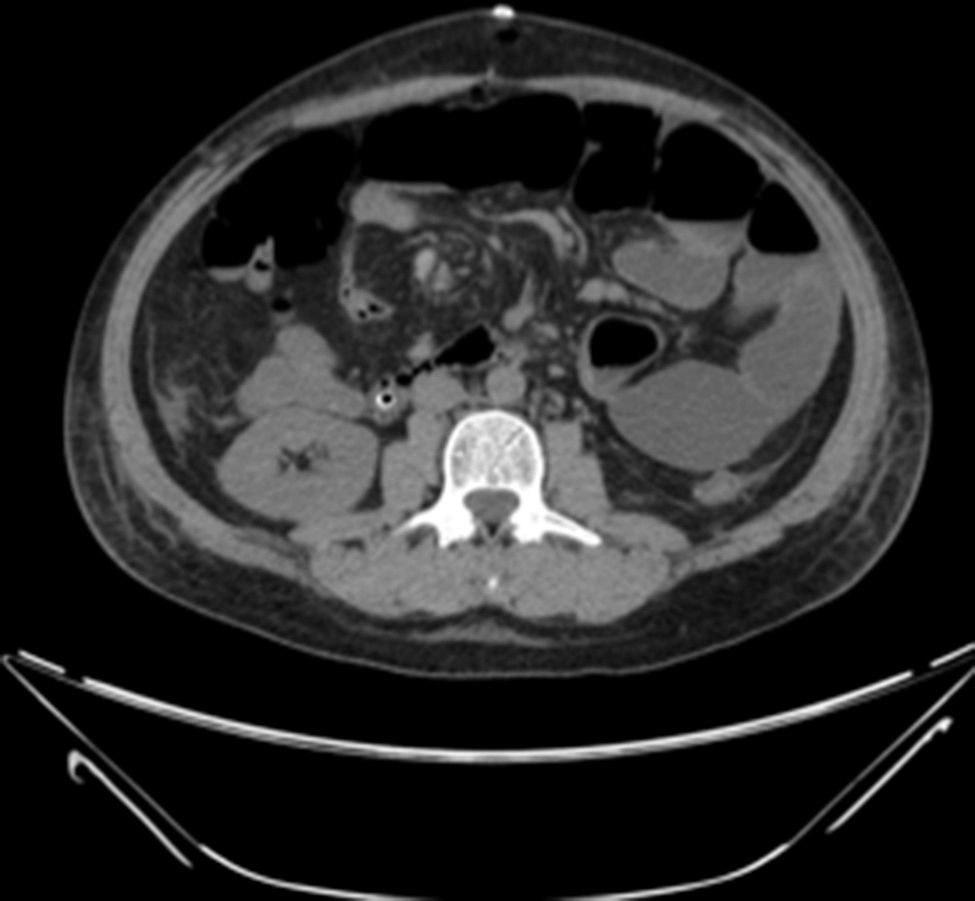
Examination revealed tachycardia, with extreme dehydration of mucosa, distended abdomen, and no peristalsis. Examination of the abdomen revealed suspected peritoneal irritation. Haematic biometry, blood chemistry and serum electrolytes were requested, which tested within normal parameters. The erect and decubitus abdominal X-rays showed important dilation of the small intestine flaps, suggestive of obstructive abdominal pattern (Figs. 1 and 2), and contrasted abdominal tomography showed enlarged lymph nodes and abnormal mesenteric vessels (Figs. 3 and 4).
Exploratory laparotomy revealed mesenteric torsion, leading to small bowel volvulus, with no ischemia or vascular compromise, with multiple mesenteric lymph nodes >2cm. The mesenteric torsion and volvulus were manually corrected, and a biopsy was taken of the mesenteric lymph nodes with histopathological report of chronic inflammation. During the postoperative period the patient presented with late post-surgical ileus, with the passing of flatus and stool accompanied by severe abdominal pain. He was monitored with arterial lactate and intra-abdominal pressure, progressing satisfactory up to the ninth post-operative day, when sudden intense abdominal pain presented, which did not yield with narcotics, accompanied by nausea and vomiting: a further X-ray of the abdomen was performed and dilated loops of small intestine with predominance in left abdomen were observed (Figs. 4–6).
A new exploratory laparotomy was performed, where mesenteric torsion which conditioned the small bowel volvulus was observed. The vascular compromise was corrected with mesenteric detortion. No intestinal resection or adhesion were performed, since no areas of adhesion, post-operative attachments or intrinsic causes (transoperative endoscopy) were in evidence. On the third post-operative day the patient presented with leucopenia, thrombocytopenia and anemia, and there was suspected reactivation of sarcoidosis, which in turn conditioned the recurrence of mesenteric torsion. Angiotensin converting enzyme serum levels were requested and tested normal. A gallium scan was also requested reporting compatible with post-operative procedure in inconclusive proximal jejunum loops. We decided to initiate treatment with pulsed steroids, observing notable improvement, and the patient was therefore discharged from hospital with no complications.
DiscussionClinical presentation of mesenteric torsion is an intestinal obstruction, presenting with an acute abdomen and a major systemic inflammatory response which may compromise hemodynamic status. Abdominal pain is the most common symptom in 94% of patients and may be very intense.1 The severity of the pain is directly related to the level of vascular occlusion and not to the level of intestinal obstruction, and the intensity of pain does not correspond with clinical findings, since only 26% of the patients present signs of peritoneal irritation.9 The laboratory findings are neither sensitive nor specific for the diagnosis of this pathology: only 66% of the patients presented with mesenteric torsion and leucocitosis, although 100% of the patients with intestinal necrosis had a leukocytes count over 10,000/cm3.1
Plain X-rays of the abdomen are non specific for the diagnosis of small bowel volvulus but are highly sensitive in the diagnosis of intestinal occlusion. The most frequent findings are loop dilation and hydro-aerial levels.10 Barium studies may be useful in certain cases, showing the Corskcrew sign or a spiral pattern.11 The abdominal CT scan with intravenous contrast material is used as the diagnostic method of choice; it is fast, non-invasive and has a sensitivity rate of between 89% and 100%.12 In the said study non specific data compatible with intestinal obstruction may be observed as may the signs characteristic of mesenteric torsion, such as the spiral or whirl sign, also known as the peacock's sign. These topographic data are observed because the bowel gyrates around mesenteric vessels, which generate this classical image.2,10,11,13
The treatment of small bowel volvulus involves surgery. The main aim is to reduce the volvulus and re-establish blood flow; early diagnosis is therefore of the utmost importance.1,2
Mesenteric distortion as a single therapeutic maneuver is successful in cases where there is no incidence of intestinal ischemia; however, in approximately 50% of cases, it is necessary to perform small bowel resection owing to vascular compromise.1
In cases of mesenteric torsion by adhesion, the initial surgical management, apart from detortion, is adherenciolisis. During the last century procedures to avoid the recurrence of intestinal obstructions were devised for the situations in which the intestinal adherences generated recurrence of intestinal volvulus and mesenteric torsion. The purpose of this adherence procedure, also known as “enteropexia” is to create controlled adherences and put the intestine in a certain position to prevent its volvulus or obstruction.1,2,14
The Noble procedure is one of the most well known and consists of folding the small bowel loops every 15–20cm in zigzag with catgut, leaving the first 15–20cm of the jejunum, to the ileocecal valve free. The Childs-Phillips procedure modified by McCarthy differs from the Noble procedure as the small bowel loops are not sutured, but where the mesentery is joined by sutures in a U shape perforating the mesentery proper 3 or 4cm from the intestinal loops. The theoretical advantage is that, because the bowel is not sutured, there is no change in peristalisis; however, the probability of vascular injury is greater. In the simplified Etala procedure the loops are folded similarly to the Noble procedure, but enteropexia is carried out with 3 or 4 stitches along the mesentery in the area of the adjoining loops. The Baker procedure involves adherence of the small bowel without sutures in the intestines or mesenterium: a long tube is inserted by gastrostomy which passes through the whole of the small bowel to the caecum. The end of the probe has a ball and this is inflated once it has passed through the ileocaecal valve. The probe enables continuity, avoiding bends or narrowing pathways, whilst the intestinal loops are fixed with new adherences. Extraction is made once the patient can tolerate oral feeding and an X-ray shows correct intestinal transit.11
ConclusionsAt present the folding of the intestine and the mesentery is only of interest due to the high rate of complications with enteroenteric or enterocutaneous fistulae, internal hernia and intestinal necrosis.12 Due to these complications, conservative surgical treatment, i.e. devolvulation and no intestinal resection, as in our case, has been used with greater frequency in cases where it is unnecessary to perform intestinal resection, achieving favorable results with lower morbidity and mortality.1,2,14
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Santín-Rivero J, Núñez-García E, Aguirre-García M, Hagerman-Ruiz-Galindo G, de la Vega-González F, Moctezuma-Velasco CR. Vólvulo de intestino delgado. Reporte de caso y revisión de la bibliografía. Cirugía y Cirujanos. 2015;83:522–526.