Splenic involvement secondary to blunt abdominal trauma is often treated by performing a splenectomy. The severity of the post-splenectomy syndrome is currently well known (blood loss, sepsis), so there is an increasing tendency to preserve the spleen. The case is presented of splenic preservation after blunt abdominal trauma with hilum involvement, emphasising the role of Floseal® as a haemostatic agent, as well as the use of resorbable meshes to preserve the spleen.
Clinical caseA 22-year-old woman presenting with a grade IV splenic lesion secondary to a blunt abdominal trauma after a traffic accident. Partial splenic resection was performed and bleeding was controlled with Floseal® and use of a reinforcing polyglycolic acid mesh. No postoperative complications occurred, being discharged on day 5. The long-term follow-up has been uneventful.
ConclusionThe use of haemostatic agents such as thrombin and the gelatine gel (FloSeal®) and the use of polyglycolic acid meshes enable spleen-preserving surgery, making it a feasible and reproducible procedure and an alternative to classical splenectomy.
La afectación esplénica secundaria a un traumatismo abdominal cerrado es frecuentemente tratada mediante esplenectomía. Ante la gravedad de las consecuencias del síndrome postesplenectomía (pérdidas hemáticas, sepsis, etc.) cada vez se tiende más a la preservación del órgano afectado. Presentamos un caso clínico de preservación de bazo tras traumatismo abdominal cerrado con implicación hiliar de dicho órgano, en el que se recurre al papel esencial del Floseal® como agente hemostático.
Caso clínicoMujer de 22 años que presenta traumatismo abdominal cerrado tras accidente de tráfico, con diagnóstico de lesión esplénica del polo inferior con compromiso hiliar que implica la vascularización de dicha región. Se procede a la intervención quirúrgica urgente con preservación esplénica mediante esplenectomía parcial y control del sangrado con Floseal® y con el empleo de una malla de refuerzo de ácido poliglicólico. La evolución postoperatoria es satisfactoria y sale del hospital al 5.o día sin incidencias.
ConclusiónEl empleo de agentes hemostáticos como el gel de gelatina y trombina (Floseal®) y el uso de mallas envolventes de ácido poliglicólico posibilitan la cirugía de preservación esplénica tras un traumatismo abdominal, representando una alternativa segura y factible a la esplenectomía completa clásica, con el beneficio de la conservación del órgano y de sus funciones.
The spleen is one of the intra-abdominal organs most frequently damaged in blunt abdominal trauma. The severity of signs and symptoms or lack of surgical experience often lead to a total splenectomy.1 The spleen plays an important role in organ defence due to its filtrating mechanisms, phagocytosis and the synthesis of complementary and immunoglobin factors.2
The risk of severe infections following splenectomy has led to radical changes in splenic trauma management, fostering splenic preservation techniques, including the application of haemostatic agents, splenorrhaphy, partial splenic resection and the wrapping up of the organ with prosthetic mesh materials.2–6 Total splenectomy has been linked to an increase of blood loss, with the need for transfusions, the formation of postoperative abscesses of the residual splenic cavity and the increase in mortality rates from sepsis in patients who have undergone total splenectomies.7,8 Medical references state that when at least 25% of the healthy spleen parenchymal. All the immunological and haematological functions of this organ were maintained.6,7
Splenic vascularisation is segmentary and very variable. The splenic artery supplies irrigation to the spleen and to substantial parts of the stomach and the pancreas. Close to the splenic hilum the artery normally divides into superior and inferior terminal branches, and each branch divides in turn between 4 and 6 segmentary intra-splenic branches.6 The surgical anatomy of splenic vascularisation should therefore considered since it may help surgeons to perform partial resections.
At present, preservation of the spleen either using non surgical management or conservative surgery is the most accepted treatment in cases of blunt and penetrating trauma where this organ is affected.9,10
Clinical caseA 22 year old woman with no personal history of interest was taken to the emergency services after presenting with blunt thoracoabdominal trauma as a result of a car-motorbike collision accident. The patient was conscious and focused on arrival, and scored 15 on the Glasgow scale, with slight mucocutaneous paleness; blood pressure figures stayed below reference figures (99–55mmHg); she was eupneic and her heart rate was between 55–60bpm. The patient only mentioned abdominal pain down her left side and left hypochrondrium. No other injuries were identified after systematic examination.
A FAST scan was performed which showed the presence of free intra-abdominal fluid. As the patient was haemodynamically stable, we decided to perform computed tomography which showed up a splenic blowout fracture involving the lower spleen pole (grade IV of the Organ Injury Scaling [OIS] classification of the American Association for the Surgery of Trauma [AAST]) with imaging of active bleeding at several foci. We decided to perform emergency surgery as a result.
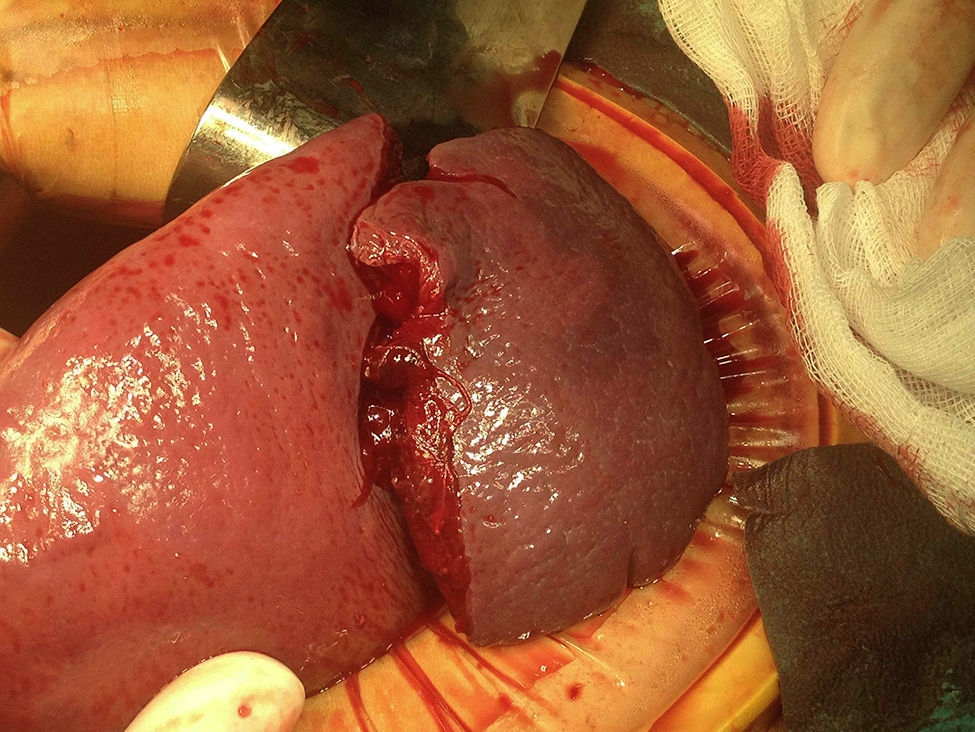
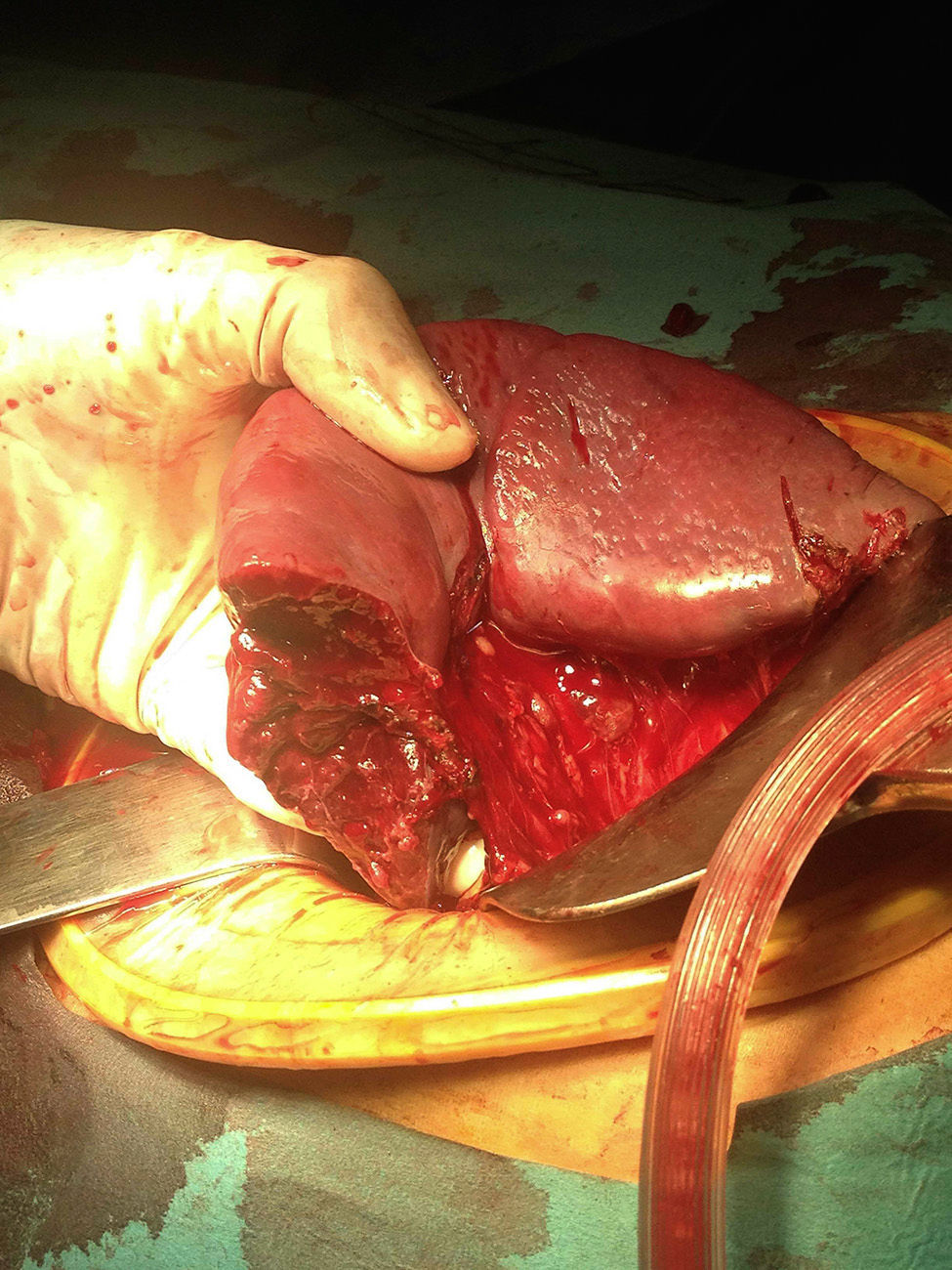
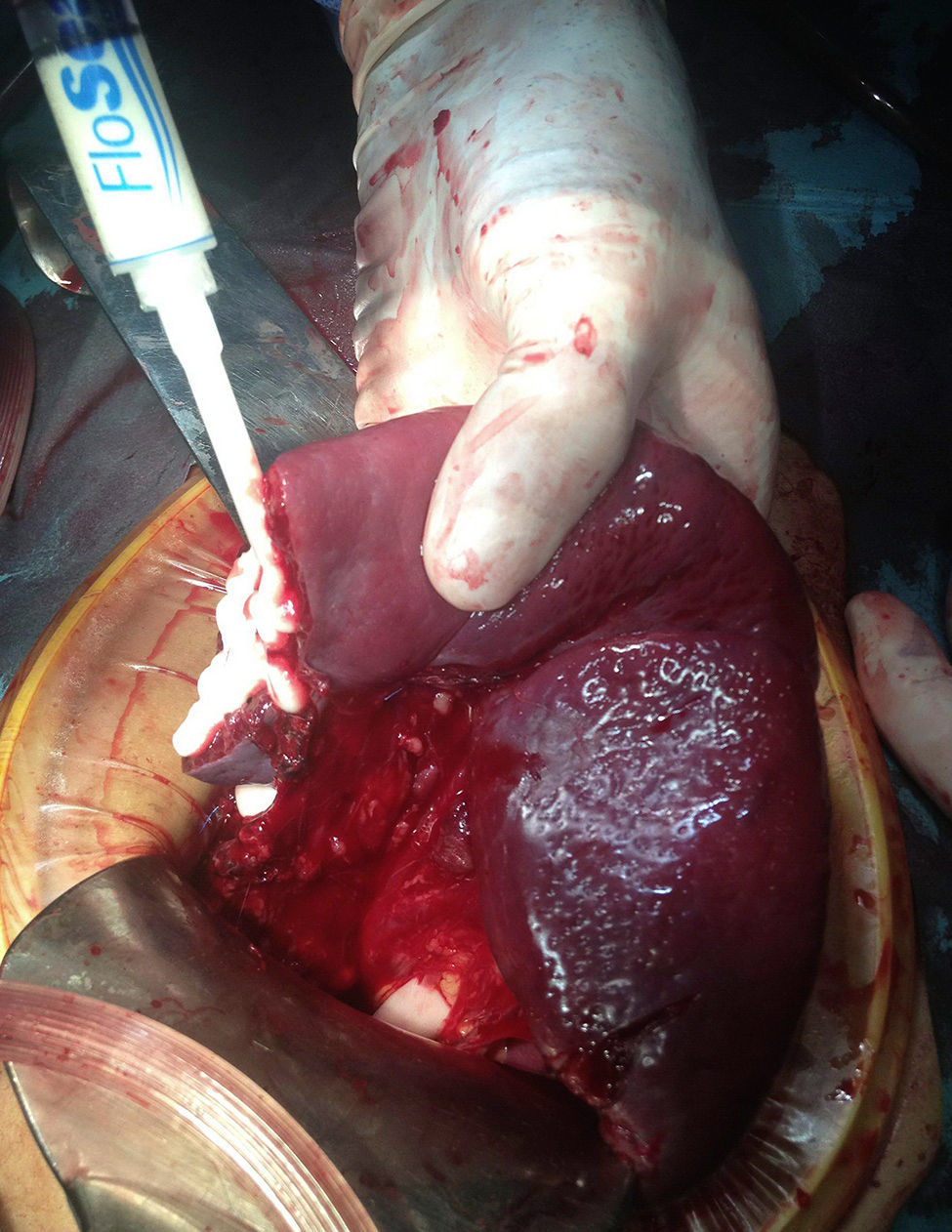
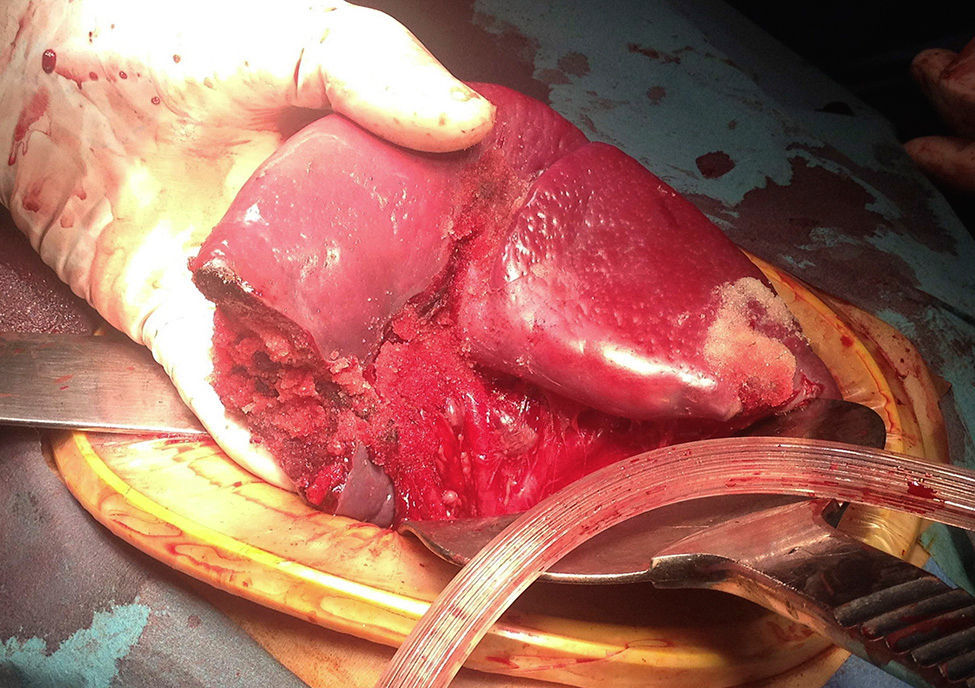
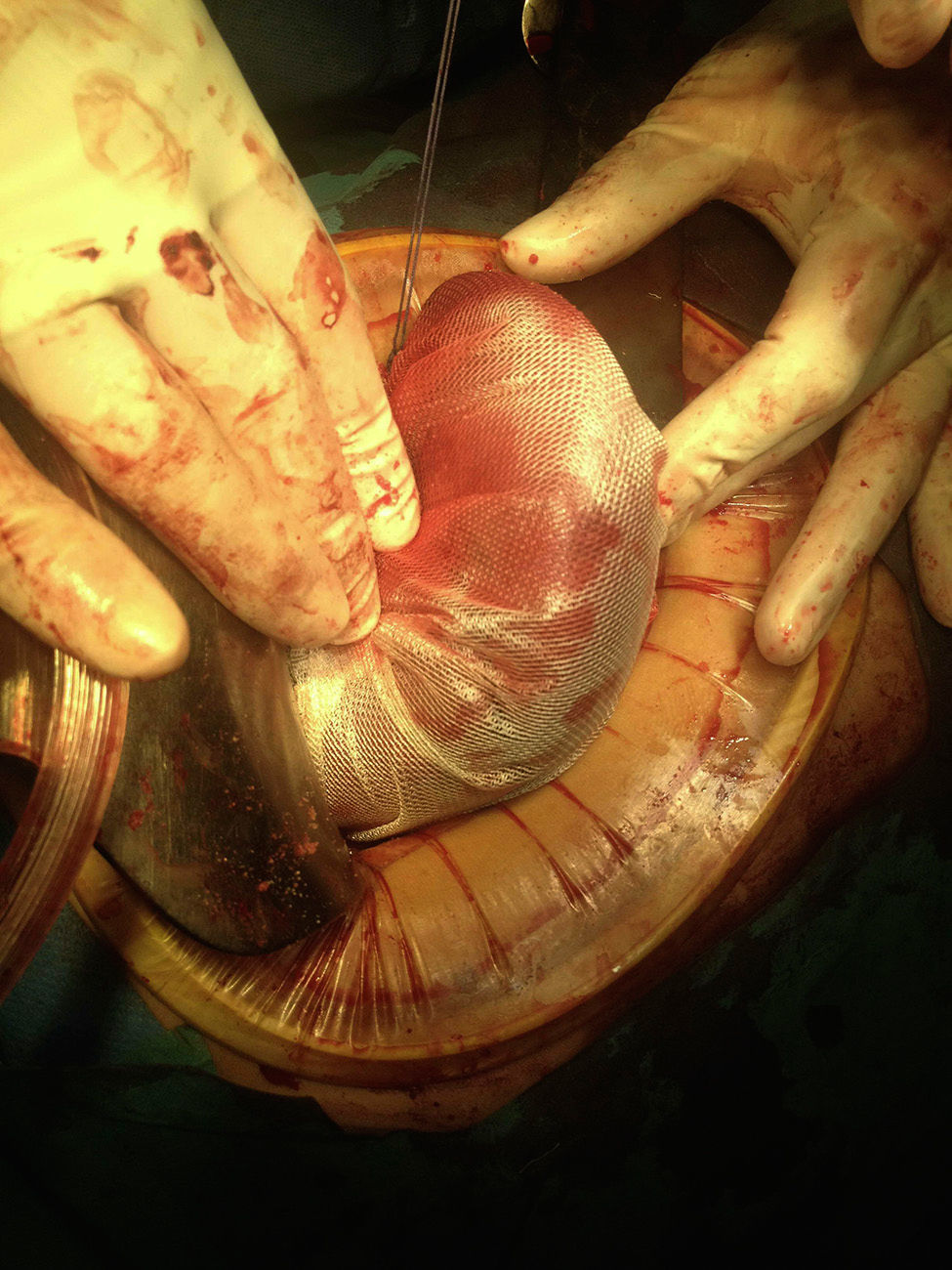
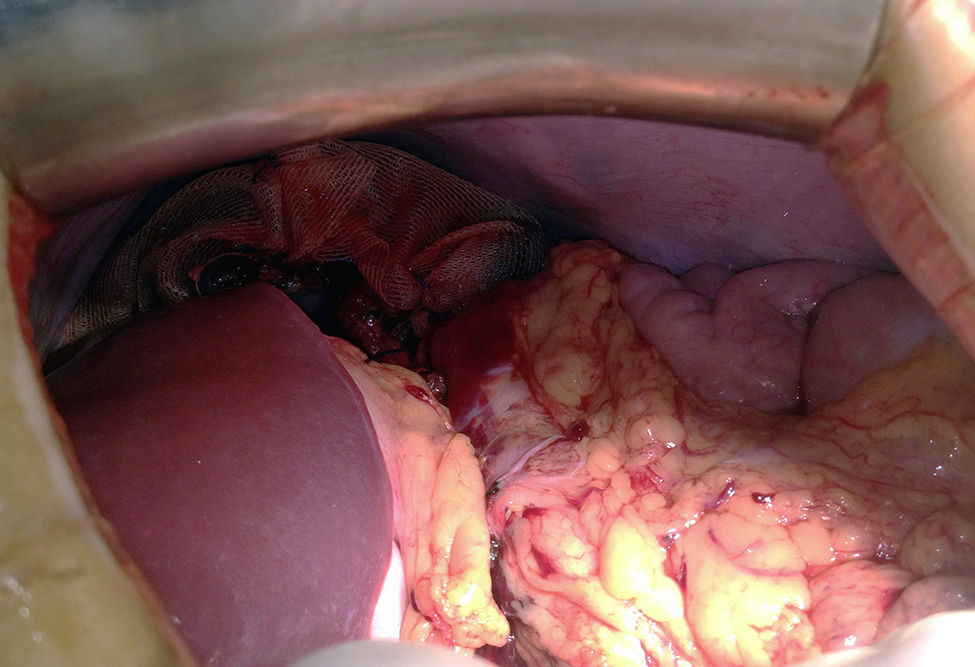
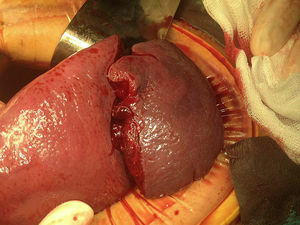
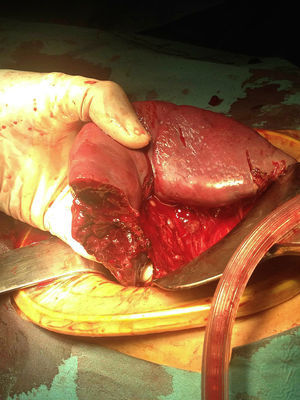
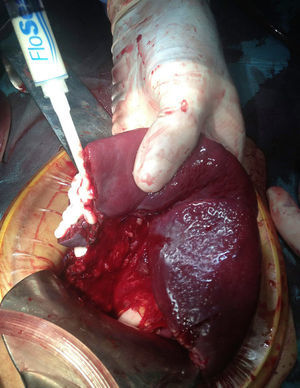
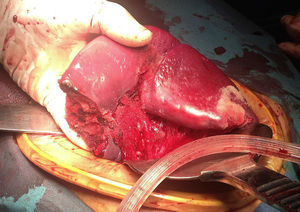
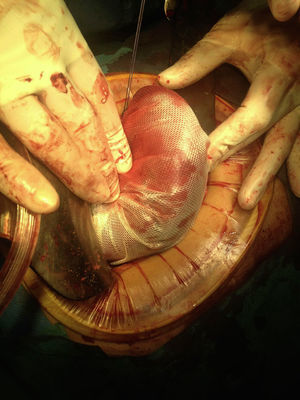
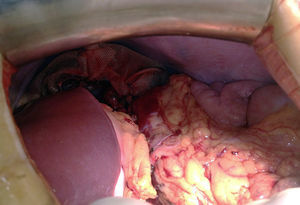
Exploratory laparotomy was performed with supra-umbilical access and moderate haemopertioneum was observed in all quadrants. Following splenic luxation and lysis of adhesions, an extensive laceration was identified in the lower pole, which involved the capsule and one intra-perisplenic haematoma with active bleeding at hilum level which devascularised said splenic region and at the same time we observed a laceration of 3cm in the upper pole (Fig. 1). As a result, and given the viability of the remainder of the spleen (which represented approximately 75% of the organ) we decided to control the bleeding at hilum level using ligation of the lower branches of the splenic veins and complete the splenic transection with electrocoagulation (Fig. 2) with posterior application of Floseal® (Baxter Healthcare, Fremont, CA, USA) in the parenchymal capillary bed and in the upper pole laceration, thus achieving total control of the bleeding (Figs. 3 and 4). The remaining spleen was then wrapped up in a bag made of reabsorbable polyglycolic acid (Safil®) aided by haemostasia in both the transection area and the area of the upper pole tear (Fig. 5); the mesh bag was then attached to the left upper quadrant, to prevent twisting of the remaining spleen which could have endangered vascularisation (Fig. 6). The whole abdominal cavity was systematically reviewed with no observation of any other injuries involved.
Postoperative evolution of the patient in the intensive care unit and on the ward was satisfactory and she was discharged from hospital 5 days after the procedure without incident.
DiscussionIn recent years, rupture of the spleen caused by blunt abdominal trauma has generally been treated by performing splenectomy. Patients who undergo splenectomy have an acquired immunodeficiency and are at greater risk of serious infection for the rest of their lives. Several authors consider that the risk of serious infections in adults who have undergone splenectomies has been overstated due to the low incidence of septic episodes in different patient series.11–13 Although the risk of sepsis in splenic patients with trauma is low, it exists, and in the references severe cases of sepsis appearing many years after splenectomy have been described. As a result, long periods of follow-up are required to evaluate the real incidence of these infectious complications in splenectomised patients.14 In contrast, low morbidity and mortality rates referred to with the use of traditional methods of splenic preservation enhance the arguments in favour of conservative procedures of spleen function.12,13 Both laboratory experience and clinical practice have demonstrated the ability for healing, regeneration, recuperation and maintenance of the immunological functions of a spleen that has undergone trauma.15
Given that these patients are usually healthy and often relatively young, conservative and organ preservation management have been used and should always be considered as an alternative to the standard total splenectomy in these patients.
In abdominal trauma where the spleen is compromised, initial treatment whether it be conservative or surgical, must be assessed for each patient individually. Therapeutic approach must mainly be substantiated by an exhaustive clinical evaluation and findings from ultrasound examinations. At present, the rate of spleen preservation using a combined non surgical and surgical treatment is approximately 40–75%.4,16–18
Percentage rates of patients who undergo splenorrhaphy ranges between 17% and 35%; however, the overall splenic preservation rate with the use of reabsorbable mesh bags is up to 67%.18
In Spain, according to the data consulted in the references, the rate of conservative splenic surgery due to trauma is from 7% to 40%.12,15
In our case and given the level of laceration of the lower pole, we decided to perform partial splenectomy with the application of a haemostatic supplement in both the area of transection and the level of laceration of the upper pole which also allowed for its preservation. This haemostatic, Floseal® (Baxter Healthcare, Fremont, CA, USA), consists of a gelatine gel and a thrombin component which is mixed prior to use. This haemostatic consisting of reticulated gelatine granules swells up approximately by 20% when it comes into contact with blood or body fluids, reducing blood flow. Coagulation is activated by a thrombin component to form a solid haemostatic thrombin; these two procedures combine to accomplish haemostasis.7
In spleen preservation surgery, haemorrhaging initially can be controlled by using organ compression, clamping of blood vessels, sutures, electro-coagulation and the implantation of haemostatic biological products.12
Placing the spleen in a tightly-fitting bag removes the need for too many sutures and for partial splenectomy, except in cases of avulsion or over-fragmentation of any of the poles. We have confirmed that the creation of a bag with a polyglycolic acid mesh and wrapping the spleen in it is a simple and straightforward procedure which has helped us with haemostasis of the splenectomy site whilst avoiding splenorrhaphy. The polyglycolic acid mesh easily fits around the shape of the spleen and its function is to contain blood, especially in cases of parenchyma fracture and/or extensive areas of decapsulation and the formation of a neo-capsule.18,19
The use of reabsorbable meshes does not appear to change the vascularisation of the organ nor its splenic function. The mesh should not be overly tight around the organ and compression of the polar arteries and splenic hilum should be avoided as much as possible.19 Omission of this may lead to ischaemia and possible intestinal infarction.
We also recommend attaching the remaining spleen to the upper left quadrant to avoid torsion.6 In our case, assisted by the reabsorbable mesh bag we were able to proceed with attachment from several anchorage points.
Open surgery continues being used in trauma, for both splenectomy and spleen preservation, particularly when the patient is haemodynamically unstable. We chose open surgery despite the fact that the laparoscopic approach in splenic pathology treatment has become easier and safer thanks to technological advances and increasing surgical experience. In the medical references this approach has been recommended even for trauma injuries in the organ, including splenic haemostasis techniques and total and partial splenectomy.20–24 Improvements in technical instrumentation in elective splenic surgery and extensive experience in elective splenic surgery will be essential factors to guarantee laparoscopy as an effective procedure in splenic surgery for trauma.
ConclusionThe decision regarding which procedure to use after splenic trauma depends on the severity of the injury and the patient's condition and must be decided on an individual basis. The use of haemostatic agents such as gelatine gel and thrombin and/or the use of polyglycolic acid mesh bags enable us to choose an alternative to the traditional splenectomy approach for spleen preservation in selected cases.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Navas-Cuéllar JA, Canete-Gómez J, López-Bernal F, García-Rivera C, Pareja-Ciuró F, Padillo-Ruiz J. Cirugía preservadora de órgano tras traumatismo esplénico cerrado con implicación hiliar. Cir Cir. 2015;83:516–521.