Acute gastric volvulus is a rare, but potentially life-threatening, cause of upper gastrointestinal obstruction.
Clinical caseMale of 60 years old with severe epigastric pain and abdominal distension with haematemesis on two occasions. The patient was haemodynamically stable, with abdominal distension and palpable epigastric fullness. Hematic cytology showed: haemoglobin 8.2g/dl and haematocrit 27%. Abdominal X-ray showed an elevation of left diaphragm with a hugely dilated stomach. A nasogastric tube was inserted. Endoscopy was performed. There was no active bleeding, but it was impossible to reach the duodenum due to the stomach distortion. The upper gastrointestinal X-ray study showed the appearance of an inverted stomach in the chest and an organoaxial gastric torsion. The CT scans of thorax and abdomen showed a gastric ascent into the thoracic cavity. Laparoscopic surgery was performed, finding the left hemi-diaphragm elevated, and the stomach, splenic angle of the colon, the spleen and tail of the pancreas were also raised. A linear gastrectomy (gastric sleeve) was performed. The postoperative progress was satisfactory. Oral feeding was started 72h after surgery, and the patient was discharged, and has remained asymptomatic during the following by 8 years.
ConclusionsEmergency physicians must maintain a high level of suspicion in patients that present with signs and symptoms suggesting upper digestive tract occlusion. The gastric sleeve is an excellent alternative to avoid recurrence of gastric volvulus.
El vólvulo gástrico agudo es un problema infrecuente como causa de obstrucción gastrointestinal.
Caso clínicoPaciente varón de 60 años que acude a urgencias por dolor epigástrico severo acompañado de distensión abdominal, con hematemesis en 2 ocasiones. A la exploración física: hemodinámicamente estable, con distensión abdominal en epigastrio, ruidos abdominales disminuidos; la citometría hemática mostró: hemoglobina 8.2g/dl y hematocrito de 27%. La radiografía de abdomen mostró: elevación del hemidiafragma izquierdo y gran dilatación de estómago; por lo que se le colocó sonda nasogástrica. Por endoscopia no se observó sangrado activo, siendo imposible alcanzar el duodeno por torsión gástrica. El estudio con medio de contraste mostró: estómago invertido dentro del tórax y con torsión gástrica axial. La tomografía de tórax y abdomen confirmó los hallazgos, con diagnóstico de vólvulo gástrico por eventración. Se procedió a efectuar laparoscopia, encontrando: hemidiafragma izquierdo elevado, así como estómago, ángulo esplénico del colon, bazo y cola del páncreas. Se realizó gastrectomía lineal (manga gástrica). La evolución fue satisfactoria; se inició alimentación por vía oral 72h después de la cirugía, y el paciente fue dado de alta, con seguimiento de 8años, en los que permanece asintomático.
ConclusionesEl médico de Urgencias debe mantener un alto índice de sospecha en pacientes que presentan signos y síntomas sugestivos de oclusión intestinal alta. El manejo con gastrectomía lineal (manga gástrica) es una excelente alternativa para evitar la recidiva.
Gastric volvulus is a rare clinical disorder, defined as abnormal rotation of the stomach of more than 180°, which creates a closed-loop obstruction which can result in incarceration and strangulation of the stomach. Gastric volvulus was described by Berti in 1866, 10 years later Berg1 performed the first successful operation for this problem, and in 1904 Borchardt2 described the classic triad associated with gastric volvulus: severe epigastric pain, retching without vomiting and inability to pass a nasogastric tube. The incidence and prevalence is unknown; both genders are equally affected, approximately 1–20% of the cases present in infancy, usually before the age of one, however cases have been reported in 15-year old children. Gastric volvulus in children is generally secondary to congenital defects of the diaphragm,3,4 and is rare in adults under the age of 50.
The case is presented of a male patient with a diagnosis of acute gastric volvulus, secondary to diaphragmatic eventration, on whom a subtotal linear gastrectomy was performed (gastric sleeve) achieving an excellent outcome, with follow-up of more than 8 years.
Clinical caseA 60-year old male patient who attended the emergency department with severe epigastric pain, accompanied by abdominal distension; he had presented haematemesis on 2 occasions. On physical examination the patient was found to be in a condition appropriate to his age, haemodynamically stable, with predominantly epigastric abdominal distension confirmed by tympanic on percussion, diminished abdominal sounds, haematic cytometry showed haemoglobin 8.2g/dl and haemocrit of 27%. Simple abdominal radiography showed elevation of the left hemidiaphragm, with a hugely dilated stomach (Fig. 1). A nasogastric tube was placed for the drainage of haematic material, and the pain was reduced. Two ulcers of the gastric fundus were found on endoscopy, active bleeding was not observed, it was impossible to find the duodenum due to the gastric torsion.
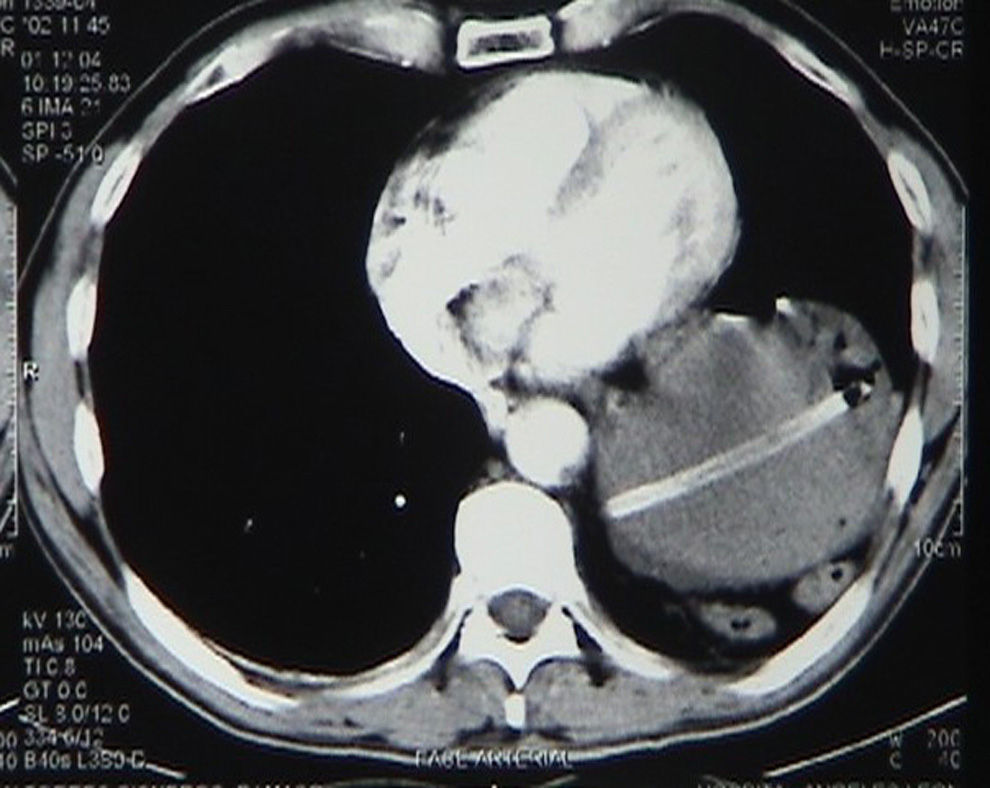
Gastrointestinal radiological contrast study showed the appearance of an inverted stomach inside the chest with axial gastric torsion (Fig. 2). CT scans of the chest and abdomen confirmed the position of the stomach inside the thoracic cavity, it was not possible to identify the diaphragm (Fig. 3). Preoperative tests of respiratory function did not show restrictive syndrome, vital capacity, and expiratory volume/1s were normal; a blood transfusion with packed blood cells was given prior to surgery. A laparoscopy was performed, finding: elevated left hemi-diaphragm, and the stomach, splenic angle of the colon, the spleen and tail of the pancreas. A hyperaemic area in the stomach was observed corresponding to the ulcers seen on endoscopy; the oesophageal hiatus was dissected, the diaphragmatic pillars were normal. A linear gastrectomy (gastric sleeve) was performed starting with section of the short vessels, the gastric band was calibrated with a 34Fr tube, a linear cutter stapler was used (Endo GIA 45-3.5), the first firing at 7cm from the pylorus, the entire line of staples was reinforced by Biosyn 2/0 continuous suture, and a drain was placed. The patient made satisfactory progress; then radiographic control was undertaken 48h later, no dehiscence was observed. The patient started an oral diet 72h after surgery and the patient was discharged; he was followed up for 8 years and remained asymptomatic.
Borchardt's triad (pain, nausea and impossibility of passing a nasogastric tube) is diagnostic of acute gastric volvulus, which occurs in 70% of cases. Carter et al.5 described 3 additional findings, which are suggestive of this diagnosis, which include: stomach located in the chest, gas occupying the lower part of the chest and the upper part of the abdomen on chest X-ray and obstruction in the site of the volvulus in the gastrointestinal series.6 Hiccups have been reported as an added symptom.7 Intra-abdominal gastric volvulus8 frequently manifests as severe pain, of sudden onset, located in the upper left quadrant of the abdomen; intrathoracic gastric volvulus9 manifests as gnawing pain in the chest radiating to the neck, shoulder, arm and back. It is almost always associated with cardiopulmonary compromise, caused by gastric distension, and can mimic a myocardial infarction, with minimal abdominal manifestations. In addition to the pain there is progressive abdominal distension and retching; some patients present haematemesis (this case) secondary to ischaemia of the gastric mucosa, and this can cause rapid progression to hypovolaemic shock due to blood and fluid loss. The classification of gastric volvulus proposed by Singleton10 relates to the axis around which the stomach turns and includes: organoaxial rotation, mesentericoaxial rotation, and a combination of both. In the former the stomach turns on an axis which connects the gastro-oesophageal union and the pylorus, the antrum rotates in the opposite direction to the gastric fundus, this type being the most common, as in our case. It manifests in 59% of cases and is usually associated with defects of the diaphragm; strangulation and gastric tissue necrosis has been reported in 5–28% of patients. In relation to aetiology, gastric volvulus can be classified as type I (idiopathic) or type II (congenital or acquired): 2/3 cases are the idiopathic form and it is thought that this is due to abnormal laxity of the gastrosplenic, gastroduodenal, gastrophrenic and gastrohepatic ligaments, allowing the approximation of cardiac and pyloric ends when the stomach is full. This is more common in adults, but has been reported in children. Type II gastric volvulus is caused by diaphragmatic defects,11 and is the most common cause of gastric volvulus in adults. The laboratory is generally not necessary for diagnostic support, however hyperamylasaemia12 has been reported and raised alkaline phosphatise and the diagnosis can be confused with that of pancreatitis. Radiographic studies (simple abdominal plate with barium contrast) and computed axial tomography confirm the diagnosis. Endoscopy13 can be useful in the diagnosis, as it reveals distortion of the gastric anatomy with difficulty or impossibility of visualising the pylorus, which is suggestive of gastric volvulus. In late stages of gastric volvulus, strangulation of the blood vessels causes ischaemic ulceration and fissures in the gastric mucosa. A diagnosis of gastric volvulus is usually based on barium studies and some authors recommend computed axial tomography as the study of choice; studies of the upper digestive tract with contrast medium using barium or gastrografin with high sensitivity and specificity, as they show gastric torsion and confirm diagnosis in 81–84% of cases; computed axial tomography offers immediate diagnosis, as it shows the presence of 2 bubbles with a transition line at gastric level, and also has the advantages of making coronal reconstructions, and also enables visualisation of the presence of gastric pneumatosis and free air, and evaluation of the diaphragm.
Mortality due to gastric volvulus reaches 80% when not surgically corrected; historically, mortality rates of 30–50% have been reported with acute gastric volvulus, strangulation being the principal cause of death, due to necrosis and perforation.14 With advances in the diagnosis and surgical management, mortality has dropped to 15–20% of acute gastric volvulus cases, and it varies from 0% to 13% for chronic gastric volvulus; emergency surgical intervention is indicated for acute gastric volvulus,15 and is still considered an emergency by many surgeons. There are increased reports of laparoscopic16 repair of gastric volvulus, which reduces the morbidity associated with open surgery procedures; if there is no peritonitis and the patient is not unstable laparoscopy seems to be an appropriate technique. The principles of treatment of gastric volvulus are based on: decompression, reduction and prevention of recurrence, which is achieved by surgical intervention. Options for repair include: repair of diaphragmatic hernia, simple gastropexy, gastropexy with division of the gastrocolic omentum, fundo-antral gastrectomy and repair of diaphragmatic eventration. A subtotal linear gastrectomy (gastric sleeve) was performed on our patient, placing trocars high in the abdominal wall to enable the instruments to reach the chest. In general the strategy is similar to that used for other gastrointestinal surgery, such as laparoscopic antireflux surgery, with a less than usual pneumoperitoneum (10–12mm Hg) to enable reduction of the hernia content. Complications are similar to those seen in other conditions which require major abdominal surgery.
ConclusionsGastric volvulus is a rare and little recognised surgical emergency which should be considered a differential diagnosis in patients presenting sever epigastric pain, retching and evidence of gastric obstruction, especially if it is difficult or impossible to pass a nasogastric tube. Patients who are critically ill or who have a diagnosis of peritonitis should be taken to the operating theatre immediately. If time allows and there is diagnostic doubt, the gastroduodenal series should be implemented, surgical repair being the treatment of choice. The gastric sleeve is a surgical alternative, which in the case that we present enabled the patient to remain asymptomatic over 8 years of follow-up.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Gálvez-Valdovinos R, Marín-Santillán E, Funes-Rodríguez JF, López-Ambriz G. Manga gástrica laparoscópica en vólvulo gástrico secundario a eventración diafragmática en paciente adulto. Cirugía y Cirujanos. 2016;84:138–141.