Choledochal cysts are rare. They usually present during childhood in women, but it can also be seen during pregnancy. Clinical signs and symptoms are obscured during this time, thus it can complicate the diagnosis and represent a life threatening complication for both the mother and the child.
ObjectiveTo communicate the case of 3 pregnant patients with choledochal cyst.
Clinical casesThree pregnant women in which choledochal cyst were diagnosed. Two developed signs of cholangitis. The first one underwent a hepatic-jejunostomy, but had an abortion and died on postoperative day 10. The second one had a preterm caesarean operation due to foetal distress and underwent a hepatic-jejunostomy 4 weeks later; during her recovery she had a gastric perforation and died of septic complications. The third one did not develop cholangitis or jaundice. She had an uneventful pregnancy and had a hepatic-jejunostomy 4 weeks later with good results.
ConclusionsManagement of choledochal cysts during pregnancy is related to the presence of cholangitis. When they do not respond to medical treatment, decompression of the biliary tree is indicated. Definitive treatment should be performed after resolution of the pregnancy.
Los quistes de colédoco son una enfermedad rara que afecta principalmente a mujeres en la infancia, pero que pueden presentarse durante el embarazo. Sus síntomas y signos están opacados por los cambios en esta fase, por lo que el diagnóstico puede ser tardío y sus complicaciones poner en peligro tanto a la madre como al producto.
ObjetivoPresentar 3 casos de quiste de colédoco en embarazadas, tratadas en un hospital de tercer nivel.
Casos clínicosPresentamos 3 pacientes con diagnóstico de quiste de colédoco durante el embarazo. Dos desarrollaron datos de colangitis; la primera fue intervenida quirúrgicamente con anastomosis hepaticoyeyunal, pero abortó y falleció al décimo día del postoperatorio. La segunda tuvo una cesárea pretérmino por sufrimiento fetal; 4 semanas después fue intervenida con anastomosis hepaticoyeyunal, pero tuvo una perforación gástrica y falleció por complicaciones sépticas. La tercera no desarrolló colangitis, tuvo un embarazo sin complicaciones, se le realizó anastomosis hepaticoyeyunal 4 semanas después, con buenos resultados.
ConclusionesEl tratamiento de los quistes de colédoco durante el embarazo está relacionado con la presencia de colangitis. Cuando no responden al tratamiento médico, la descompresión de la vía biliar está indicada. El tratamiento definitivo debe realizarse una vez resuelto el embarazo.
According to Angel and Nassar, et al. choledochal cysts were described by Vater in 1723.1,2 Their aetiology is unknown, based on that published by Wu3 and Gmijović et al.4 in 1936 Yotsuyanagi posed the theory that they arise from inequality in the vacuolisation of the biliary tract in early embryonic life. Currently there are 2 theories; the first postulates that the distension or cyst forms secondary to congenital stenosis of the biliary tract; the second, proposed by Babbitt,3,5 in 1969, is that they are the result of abnormal union between the bile duct and the pancreatic duct (greater than 15mm), with pancreatic reflux, increasing the intraluminal pressure of the bile duct and its distension. The latter theory is the most widely accepted.
Martínez-Ordaz and Niño-Solís6 contend that in 1959, Alonso-Lej proposed a classification that was modified by Todani in 1977. The symptoms are non-specific, principally jaundice without apparent cause during infancy and vague abdominal pain, and are even more evident in pregnant women. Pregnancy significantly alters the gallbladder, due to hormonal changes of oestrogen and progesterone levels. Oestrogens have been demonstrated to inhibit the motility of Oddi's sphincter. The gravid uterus can also accentuate or aggravate symptoms due to distal obstruction of the bile duct by compression.2
ObjectiveTo present 3 cases of choledochal cysts in pregnant women, treated in a third level hospital and to compare them with cases reported in medical literature.
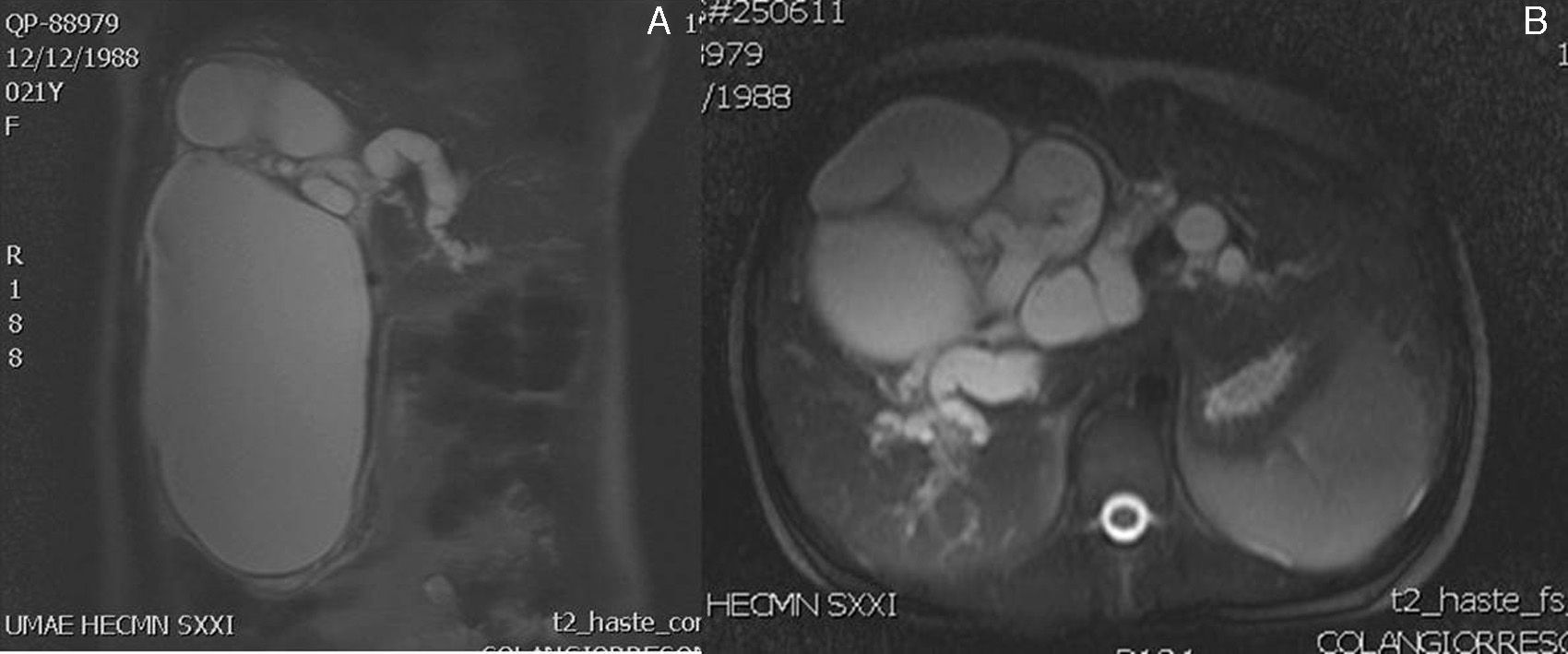
Clinical casesCase 1A 22 year-old primiparous woman, with an interuterine pregnancy of 9 weeks’ gestation. She started to suffer abdominal pain that was treated with analgesics and antispasmodics. Then she experienced nausea and later vomiting, jaundice and choluria. On physical examination she was found to be conscious, cooperative and calm, adequately hydrated, with jaundiced skin and mucosa+cardiopulmonary examination showed no compromise; there was a palpable tumour in the hypochondrium and right flank of her abdomen, which was firm, mobile, painful, with no signs of peritoneal irritation. The laboratory results showed: direct bilirubin 3.54mg/dl, indirect 0.22mg/dl, total 3.76mg/dl; with raised transaminases (alanine aminotransferase172U/l, aspartate aminotransferase 89U/l). An ultrasound was performed which reported an abdominal tumour dependent on the liver. There were no alterations obstetrically. Magnetic cholangioresonance reported a cystic lesion of 20cm in cephalocaudal and 11cm anteroposterior diameter, homogeneous, dependent on the extrahepatic bile duct (Fig. 1). The patient started with signs of cholangitis, which did not improve with medical treatment, and therefore underwent giant choledochal cyst resection, cholecystectomy and hepaticojejunal anastomosis. She was reoperated twice for a haemoperitoneum due to haemorrhage from the surgical site. As this developed absence of foetal heart rate presented, and therefore uterine curettage was performed. The outcome was poor, and the patient died due to multiple organ failure on the tenth day of the post-operative period.
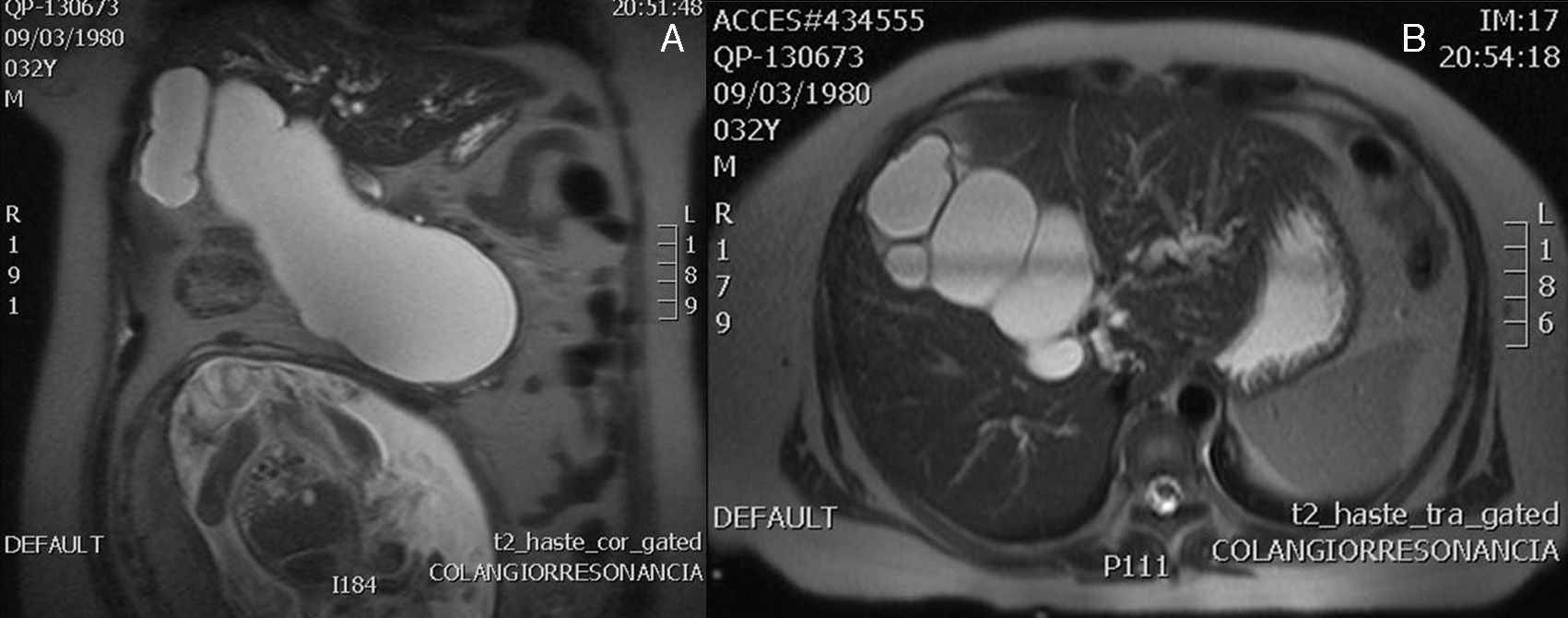
Case 2A 31 year-old woman, with an interuterine pregnancy of 22 weeks’ gestation. She had a history of one normally progressing pregnancy, with an uncomplicated labour 8 years before her current condition. A 3 week history of jaundice, choluria, acholia, colicky transflictive abdominal pain located in the epigastrium, increasing in intensity to 10/10, diaphoresis and nausea. On physical examination the patient was found to be conscious, cooperative and calm, jaundice +++, soft abdomen, rounded due to adipose panniculus and gravid uterus, with mild pain on deep palpation, with no signs of peritoneal irritation. Laboratory tests showed: albumin 2.5g/dl, total bilirubin 4mg/dl (indirect bilirubin 0.54mg/dl, direct bilirubin 3.46mg/dl) and haemoglobin 10.7g/dl. The ultrasound reported a live singleton of 22.5 weeks’ gestation from the femoral length, hydrocephaly, intrabdominal calcification indicative of foetus-in-fetu, amniotic fluid echoes, which is evidence of bleeding, placenta maturity grade II, cephalic presentation. Magnetic cholangioresonance reported dilatation of the intrahepatic biliary duct and the presence of a voluminous Todani I choledochal cyst compressing the adjacent structures (Fig. 2). An elective caesarean section was performed due to chronic foetal distress, and a live girl was delivered at 26 weeks by Capurro. Because the patient's hyperbilirubinaemia (direct bilirubin 25mg/dl) and signs of cholagitis, 4 weeks after the caesarean, an elective hepaticojejunal Roux en Y anastomosis was formed finding a findings of choledochal cyst 25cm×12cm, with firm adherences to the portal vein. The patient progressed satisfactorily over the 8 weeks post surgery. However, she presented haemorrhage of the upper digestive tract with a drop in haemoglobin and haemodynamic deterioration, and therefore an exploratory laparotomy was performed and a haemoperitoneum of 1300cc was found with the presence of ischaemic perforation in the gastric fundus. The outcome was poor; the patient presented abdominal sepsis, septic shock and disseminated intravascular coagulation, and died on the 21st postoperative day.
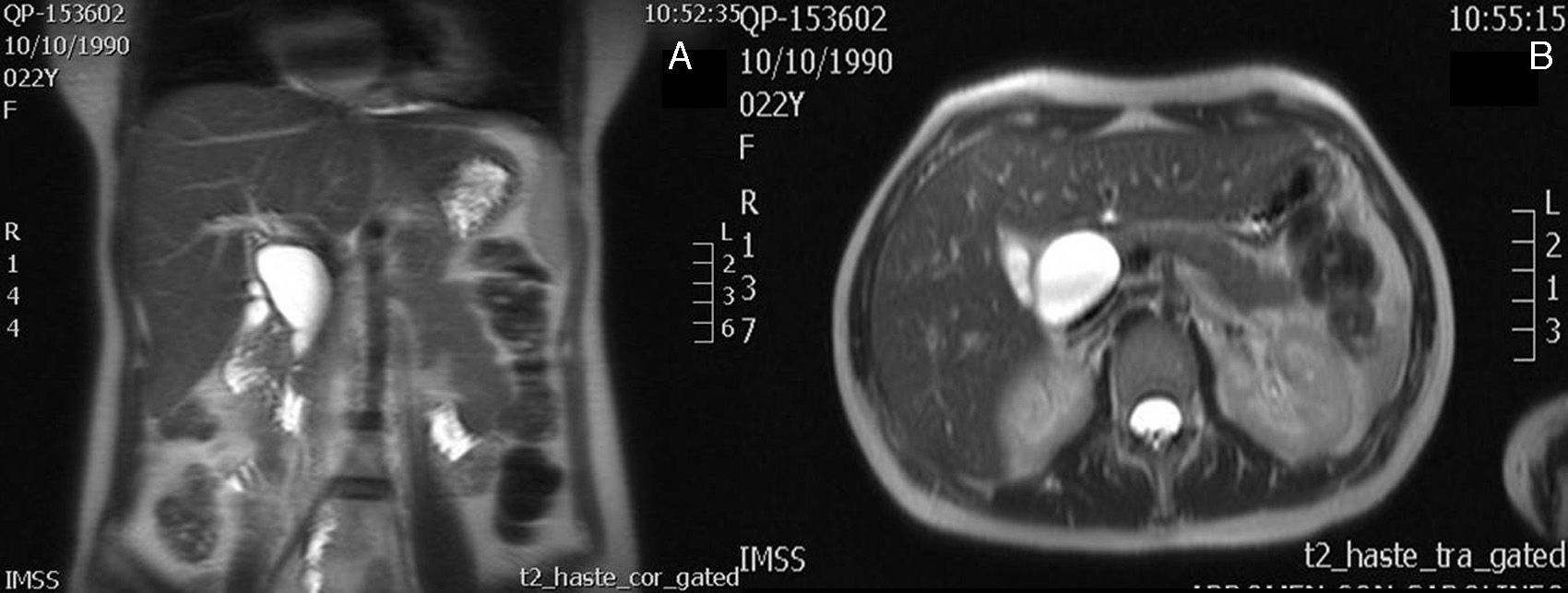
Case 3A 22 year-old primiparous patient, with no relevant history. At 20 weeks’ gestation she started with signs of mild abdominal pain in the right hypochondrium in relation to cholecystokinetics. Laboratory tests were performed which reported aspartate aminotransferase 201U/l and alanine aminotransferase 343U/l. An ultrasound was performed, reporting chronic lithiasic cholecystitis and probable choledochal cyst. Magnetic cholangioresonance was performed, which reported dilatation of the common bile duct of 5cm×6cm compatible with a choledochal cyst (Fig. 3). The patient was managed solely symptomatically for the remainder of her pregnancy. The pregnancy proceeded normally with an uncomplicated labour. One month after the patient was operated, a cholecystectomy was performed and resection of the choledochal cyst with hepaticojejunal anastomosis. Postoperative recovery was satisfactory and the patient was discharged with no complications.
DiscussionBabbit's theory postulates that abnormality in the biliopancreatic union with the formation of a long and abnormal common channel out of the control of the Boyden sphincters, allows reflux of pancreatic enzymes into the common bile duct and these cause inflammation, de-epithelialisation and thinning, with distal obstructions, which eventually causes the formation of the cyst. Incidence varies, but one case in 13,000 to 2 million live births, and is more common in women (4:1) and Asians. They are principally diagnosed during infancy (60%).3–5,7,8 Type I cysts (50–85%) and type IV (30–40%) are the most common.3,5,9
In general, the symptoms are vague; patients present jaundice and imprecise abdominal pain. The classic presentation triad is: abdominal pain (87%), jaundice (57%) and palpable abdominal tumour in the right hypochondrium (17%); it presents only in 20% of cases.6 Alterations are expected in liver function tests.
The most frequent complications are cholangitis and pancreatitis.8,10,11 Other complications include biliary cirrhosis, portal hypertension, rupture, peritonitis, vesicular or choledochal lithiasis, and the major complication is the risk of malignancy with increases with age (0.7% in minors under 10, 7% between 10 and 20, 14% in people over 20 and 50% in people over 50).2,5,12,13
Choledochal cysts in pregnant women are rare, but they represent a threat to the mother and the foetus. The main expected complications are loss of the foetus or preterm labour.12,13 Diagnosis during pregnancy is difficult, as it requires its suspected diagnosis and diagnostic aids. The most common is ultrasound, however, it is difficult during pregnancy due to the distortion of the normal anatomy of the abdomen and due to the gravid uterus.12,14 Ionising radiation or contrast studies can be performed, such as computed tomography or retrograde endoscopic cholangiopancreatography, but with extreme precaution. Cholangiography (percutaneous, endoscopic or nuclear) demonstrates the type of cyst, intra- or extra-hepatic compromise and abnormality of the biliopancreatic union. Magnetic resonance imaging can provide adequate visualisation and relationships between the choledochal cyst (size and extension) and the biliary tree; however, it has limitations for diagnosing small cysts or duct abnormalities.4,7,15,16
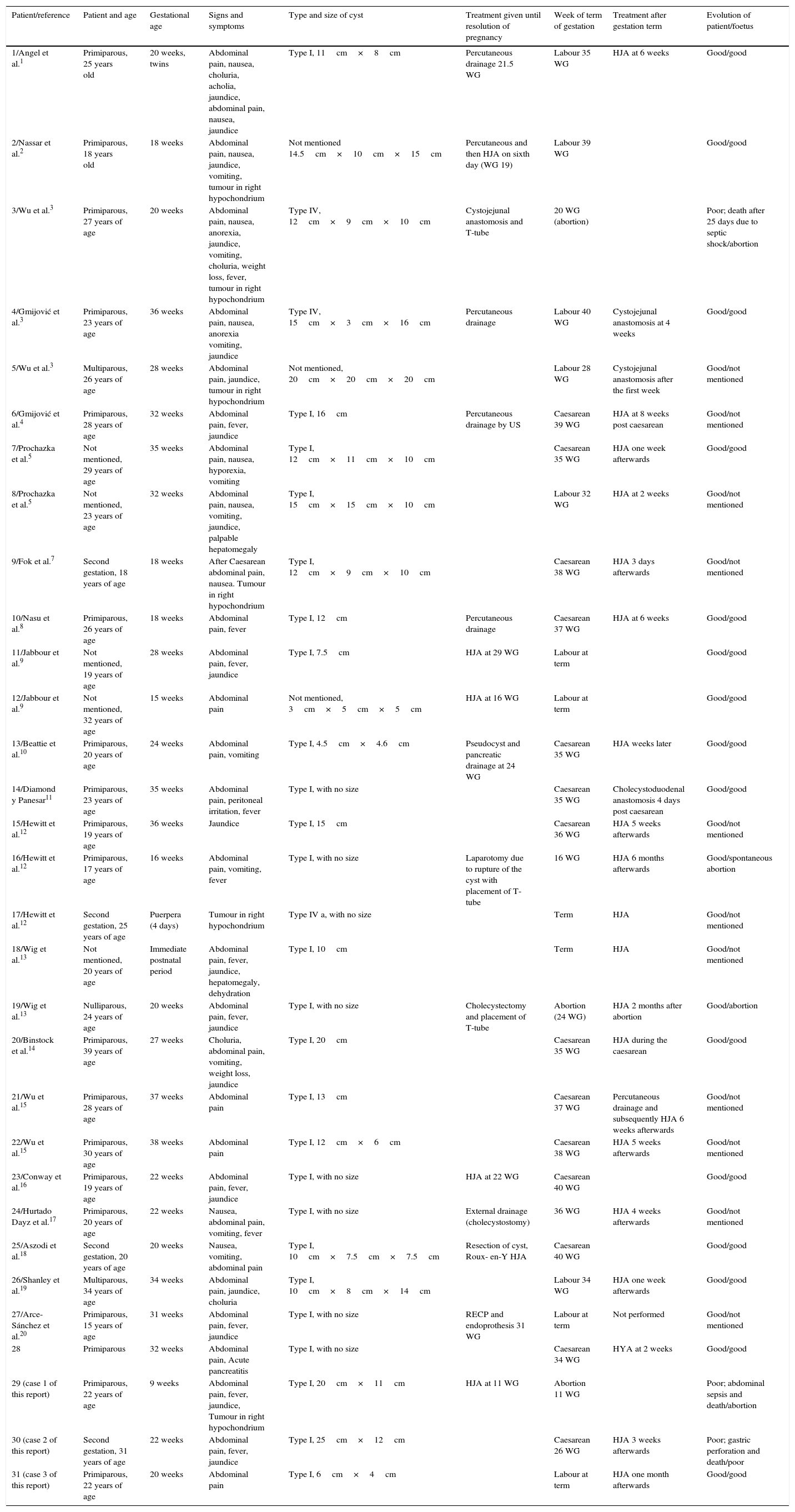
Once the diagnosis has been made, the patients should be referred to a specialist unit, as inappropriate treatment might be catastrophic to mother and foetus. Pregnant patients constitute a special situation. The presence of the cyst in the case of very large lesions, or complications developing from these lesions is associated with a rise in maternal and foetal morbimortality. Experience in the management of this disease in pregnant women was reviewed and a summary is presented in Table 11,7–21; it also includes (at the end) the 3 patients from our study; of these, in 29 diagnosis was made during pregnancy and in 2 cases in the immediate postnatal period. Eighteen patients (69%) out of the 26 where the number of pregnancies was mentioned were primiparous. The most frequent symptoms were associated with cholangitis, with abdominal pain in 28 patients (90%), jaundice in 17 (57%) and fever in 12 (40%). A palpable tumour was only mentioned in the right hypochondrium in 6 patients (19%), although the presence of a gravid uterus should be taken into consideration, which probably affected the assessment during the physical examination. In 12 patients the pregnancy was resolved through labour (39%), in 13 through caesarean section (42%) and 4 abortions (13%). It was not mentioned in 2 cases. In 15 patients (48%) pregnancy reached 36 weeks or more, in 10 it reached 35 weeks or less and 4 (13%) cases ended in abortion. In 2 cases the weeks of pregnancy were not mentioned.
Characteristics, presentation, evolution and treatment of 30 patients with a choledochal cyst diagnosed during pregnancy or the immediate post natal period.
| Patient/reference | Patient and age | Gestational age | Signs and symptoms | Type and size of cyst | Treatment given until resolution of pregnancy | Week of term of gestation | Treatment after gestation term | Evolution of patient/foetus |
|---|---|---|---|---|---|---|---|---|
| 1/Angel et al.1 | Primiparous, 25 years old | 20 weeks, twins | Abdominal pain, nausea, choluria, acholia, jaundice, abdominal pain, nausea, jaundice | Type I, 11cm×8cm | Percutaneous drainage 21.5 WG | Labour 35 WG | HJA at 6 weeks | Good/good |
| 2/Nassar et al.2 | Primiparous, 18 years old | 18 weeks | Abdominal pain, nausea, jaundice, vomiting, tumour in right hypochondrium | Not mentioned 14.5cm×10cm×15cm | Percutaneous and then HJA on sixth day (WG 19) | Labour 39 WG | Good/good | |
| 3/Wu et al.3 | Primiparous, 27 years of age | 20 weeks | Abdominal pain, nausea, anorexia, jaundice, vomiting, choluria, weight loss, fever, tumour in right hypochondrium | Type IV, 12cm×9cm×10cm | Cystojejunal anastomosis and T-tube | 20 WG (abortion) | Poor; death after 25 days due to septic shock/abortion | |
| 4/Gmijović et al.3 | Primiparous, 23 years of age | 36 weeks | Abdominal pain, nausea, anorexia vomiting, jaundice | Type IV, 15cm×3cm×16cm | Percutaneous drainage | Labour 40 WG | Cystojejunal anastomosis at 4 weeks | Good/good |
| 5/Wu et al.3 | Multiparous, 26 years of age | 28 weeks | Abdominal pain, jaundice, tumour in right hypochondrium | Not mentioned, 20cm×20cm×20cm | Labour 28 WG | Cystojejunal anastomosis after the first week | Good/not mentioned | |
| 6/Gmijović et al.4 | Primiparous, 28 years of age | 32 weeks | Abdominal pain, fever, jaundice | Type I, 16cm | Percutaneous drainage by US | Caesarean 39 WG | HJA at 8 weeks post caesarean | Good/not mentioned |
| 7/Prochazka et al.5 | Not mentioned, 29 years of age | 35 weeks | Abdominal pain, nausea, hyporexia, vomiting | Type I, 12cm×11cm×10cm | Caesarean 35 WG | HJA one week afterwards | Good/good | |
| 8/Prochazka et al.5 | Not mentioned, 23 years of age | 32 weeks | Abdominal pain, nausea, vomiting, jaundice, palpable hepatomegaly | Type I, 15cm×15cm×10cm | Labour 32 WG | HJA at 2 weeks | Good/not mentioned | |
| 9/Fok et al.7 | Second gestation, 18 years of age | 18 weeks | After Caesarean abdominal pain, nausea. Tumour in right hypochondrium | Type I, 12cm×9cm×10cm | Caesarean 38 WG | HJA 3 days afterwards | Good/not mentioned | |
| 10/Nasu et al.8 | Primiparous, 26 years of age | 18 weeks | Abdominal pain, fever | Type I, 12cm | Percutaneous drainage | Caesarean 37 WG | HJA at 6 weeks | Good/good |
| 11/Jabbour et al.9 | Not mentioned, 19 years of age | 28 weeks | Abdominal pain, fever, jaundice | Type I, 7.5cm | HJA at 29 WG | Labour at term | Good/good | |
| 12/Jabbour et al.9 | Not mentioned, 32 years of age | 15 weeks | Abdominal pain | Not mentioned, 3cm×5cm×5cm | HJA at 16 WG | Labour at term | Good/good | |
| 13/Beattie et al.10 | Primiparous, 20 years of age | 24 weeks | Abdominal pain, vomiting | Type I, 4.5cm×4.6cm | Pseudocyst and pancreatic drainage at 24 WG | Caesarean 35 WG | HJA weeks later | Good/good |
| 14/Diamond y Panesar11 | Primiparous, 23 years of age | 35 weeks | Abdominal pain, peritoneal irritation, fever | Type I, with no size | Caesarean 35 WG | Cholecystoduodenal anastomosis 4 days post caesarean | Good/good | |
| 15/Hewitt et al.12 | Primiparous, 19 years of age | 36 weeks | Jaundice | Type I, 15cm | Caesarean 36 WG | HJA 5 weeks afterwards | Good/not mentioned | |
| 16/Hewitt et al.12 | Primiparous, 17 years of age | 16 weeks | Abdominal pain, vomiting, fever | Type I, with no size | Laparotomy due to rupture of the cyst with placement of T-tube | 16 WG | HJA 6 months afterwards | Good/spontaneous abortion |
| 17/Hewitt et al.12 | Second gestation, 25 years of age | Puerpera (4 days) | Tumour in right hypochondrium | Type IV a, with no size | Term | HJA | Good/not mentioned | |
| 18/Wig et al.13 | Not mentioned, 20 years of age | Immediate postnatal period | Abdominal pain, fever, jaundice, hepatomegaly, dehydration | Type I, 10cm | Term | HJA | Good/not mentioned | |
| 19/Wig et al.13 | Nulliparous, 24 years of age | 20 weeks | Abdominal pain, fever, jaundice | Type I, with no size | Cholecystectomy and placement of T-tube | Abortion (24 WG) | HJA 2 months after abortion | Good/abortion |
| 20/Binstock et al.14 | Primiparous, 39 years of age | 27 weeks | Choluria, abdominal pain, vomiting, weight loss, jaundice | Type I, 20cm | Caesarean 35 WG | HJA during the caesarean | Good/good | |
| 21/Wu et al.15 | Primiparous, 28 years of age | 37 weeks | Abdominal pain | Type I, 13cm | Caesarean 37 WG | Percutaneous drainage and subsequently HJA 6 weeks afterwards | Good/not mentioned | |
| 22/Wu et al.15 | Primiparous, 30 years of age | 38 weeks | Abdominal pain | Type I, 12cm×6cm | Caesarean 38 WG | HJA 5 weeks afterwards | Good/not mentioned | |
| 23/Conway et al.16 | Primiparous, 19 years of age | 22 weeks | Abdominal pain, fever, jaundice | Type I, with no size | HJA at 22 WG | Caesarean 40 WG | Good/good | |
| 24/Hurtado Dayz et al.17 | Primiparous, 20 years of age | 22 weeks | Nausea, abdominal pain, vomiting, fever | Type I, with no size | External drainage (cholecystostomy) | 36 WG | HJA 4 weeks afterwards | Good/not mentioned |
| 25/Aszodi et al.18 | Second gestation, 20 years of age | 20 weeks | Nausea, vomiting, abdominal pain | Type I, 10cm×7.5cm×7.5cm | Resection of cyst, Roux- en-Y HJA | Caesarean 40 WG | Good/good | |
| 26/Shanley et al.19 | Multiparous, 34 years of age | 34 weeks | Abdominal pain, jaundice, choluria | Type I, 10cm×8cm×14cm | Labour 34 WG | HJA one week afterwards | Good/good | |
| 27/Arce-Sánchez et al.20 | Primiparous, 15 years of age | 31 weeks | Abdominal pain, fever, jaundice | Type I, with no size | RECP and endoprothesis 31 WG | Labour at term | Not performed | Good/not mentioned |
| 28 | Primiparous | 32 weeks | Abdominal pain, Acute pancreatitis | Type I, with no size | Caesarean 34 WG | HYA at 2 weeks | Good/good | |
| 29 (case 1 of this report) | Primiparous, 22 years of age | 9 weeks | Abdominal pain, fever, jaundice, Tumour in right hypochondrium | Type I, 20cm×11cm | HJA at 11 WG | Abortion 11 WG | Poor; abdominal sepsis and death/abortion | |
| 30 (case 2 of this report) | Second gestation, 31 years of age | 22 weeks | Abdominal pain, fever, jaundice | Type I, 25cm×12cm | Caesarean 26 WG | HJA 3 weeks afterwards | Poor; gastric perforation and death/poor | |
| 31 (case 3 of this report) | Primiparous, 22 years of age | 20 weeks | Abdominal pain | Type I, 6cm×4cm | Labour at term | HJA one month afterwards | Good/good |
HJA, hepaticojejunal anastomosis; RECP, retrograde endoscopic cholangiopancreatography; WG, weeks of gestation; US, ultrasound.
Treatment of pregnant women should be conservative when the cysts are asymptomatic.1,3,14,19 Fifteen patients were treated conservatively. The pregnancy of nine of these patients (60%) resolved before week 36; subsequently, 13 were reoperated for resection of the cyst with hepaticojejunal anastomosis, and 2 patients underwent cystoduodenal and cystojejunal anastomosis, respectively. One of the patients (case 2 of this report) died during the late postoperative period. Seven percent mortality is reported with this treatment.
In symptomatic cases which do not respond to treatment with antibiotics the cyst should be decompressed via the percutaneous transhepatic, endoscopic or surgical route.3,5,8,14 In these patients 9 drainages were performed, 5 percutaneous, 3 surgical with placement of a tube (T tube in 2 cases and another with cholecystostomy) and one endoscopic retrograde cholangiopancreatography. Progress after drainage was good in 7 patients (in 5 cases the pregnancy was resolved in week 36 or later), and in 2 cases the mother progressed well but lost the foetus (both were patients operated with placement of a T-tube due to rupture of the cyst and grave cholangitis, respectively); none of the patients in this group died. After resolution of the pregnancy, 7 patients underwent resection of the cyst with hepaticojejunal anastomosis, another patient underwent cystojejunal anastomosis, and in one patient no other subsequent surgical treatment was reported.
The definitive treatment is surgical, and therefore the decision to operate should take into account the risk to the mother–child binomial, and the complications of the disease itself. If possible, surgical treatment should be performed up until the second trimester, as surgery carries a high risk of morbimortality in pregnant women.2,12,18 Surgery is justified in the first trimester when the life of the mother is at risk, and induction of labour or caesarean section during the third trimester if the foetus is sufficiently mature.3,9 Definitive surgical treatment was performed on 7 patients during pregnancy. In 5 cases (71%) both the mother and foetus made good progress, and in all cases the pregnancy went to term. Two cases (28%) made poor progress, with maternal death secondary to the complications of surgery.
Definitive surgery should be based on the classification of the cyst and the general condition of the patient. The surgery of choice is hepaticojejunal Roux-en-Y anastomosis owing to its low incidence of cholangitis and surgical reintervention. Resection of the cyst is widely accepted for types I, II and IV. Type III cysts require surgical drainage generally by the endoscopic route with sphincterotomy. There is controversy for type IV, the options being resection of the extrahepatic cyst alone or total resection of the cyst with hepatectomy. In type V cysts some authors recommend hepatic resection. It is recommended that resection is performed over the derivation of the cyst due to the greater incidence of carcinoma of the common bile duct in the cyst remnant.2,3,18 At 10 years’ follow-up one of the cases on whom this procedure was performed had developed a carcinoma.
ConclusionsCholedochal cyst is a rare disorder which can be found in patients during pregnancy. A successful prognosis in pregnant patients is based on the time that the disease is diagnosed, the patient's general condition, her clinical progress during monitoring and when the final treatment is given. Patients should be referred to specialist units for integral management. Conservative treatment is indicated for asymptomatic patients. Those with cholangitis should be treated with antibiotics and if necessary decompression of the bile duct through the percutaneous transhepatic route or retrograde endoscopic cholangiopancreatography, which is a temporary form of treatment. The definitive procedure (resection with hepaticojejunal anastomosis) should be based on the patient's general condition, the support of diagnostic aids and surgical experience as these are patients with a high risk of morbimortality.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Martínez-Ordaz JL, Morales-Camacho MY, Centellas-Hinojosa S, Román-Ramírez E, Romero-Hernández T, de la Fuente-Lira M. Quiste de colédoco y embarazo. Reporte de 3 casos y revisión de la bibliografía. Cirugía y Cirujanos. 2016;84:142–151.