Placenta percreta may lead to massive obstetric haemorrhage, haemodynamic decompensation, and ultimately death. Total obstetric hysterectomy is universally accepted as treatment; however, the emergence of new techniques such as the uterine artery angioembolization approach, and the use of chemotherapy agents such as methotrexate, are alternatives also described in the literature.
Clinical caseA 28 year-old patient, in her fourth gestation, with a previous history of 2 vaginal and 1 caesarean birth 4, in her 28.4 week of pregnancy, by second trimester ultrasound, was diagnosed with placenta percreta with bladder and rectal invasion using magnetic resonance imaging. Multidisciplinary and sequential treatment included: Caesarean with placenta in situ, uterine artery embolisation immediately after caesarean, chemotherapy with methotrexate weekly for 4 doses, and finally obstetric hysterectomy after bilateral hypogastric artery ligation. The outcome was favourable and the patient was discharged in good general condition.
ConclusionsThe protocoled and sequential management including selective embolisation immediately after caesarean section with placenta in situ, weekly chemotherapy with methotrexate and obstetric hysterectomy, preceded by bilateral ligation of the hypogastric arteries, is a therapeutic alternative to be considered in cases of placenta percreta.
El percretismo placentario puede llevar a hemorragia obstétrica masiva, descompensación del estado hemodinámico y finalmente a la muerte. Con relación al tratamiento, la histerectomía obstétrica total de inicio se encuentra universalmente aceptada; sin embargo, el surgimiento de nuevas técnicas de abordaje, como la angioembolización de arterias uterinas y el uso de agentes quimioterapéuticos como el metotrexato, con el objetivo de disminuir las complicaciones asociadas, son alternativas también descritas en la literatura.
Caso clínicoPaciente femenina de 28 años de edad, multigesta, gesta 4, partos 2, cesárea una, que cursó con embarazo de 28.4 semanas por ultrasonografía del segundo trimestre, es diagnosticada de percretismo placentario con invasión vesical y rectal, mediante resonancia magnética. Ingresa bajo protocolo de manejo multidisciplinario y secuencial, cuyos componentes fueron cesárea con placenta in situ, embolización selectiva de arterias uterinas inmediatamente posterior a cesárea, quimioterapia semanal con metotrexato por 4 dosis y, finalmente, histerectomía obstétrica, previa ligadura bilateral de arterias hipogástricas. El resultado fue favourable, ya que la paciente egresó en buenas condiciones generales, sin presentar hemorragia ni otras complicaciones durante el tratamiento.
ConclusionesEl manejo protocolizado y secuencial, que incluye embolización selectiva de las arterias uterinas inmediatamente posterior a la cesárea con placenta in situ, quimioterapia con metotrexato de forma semanal y, finalmente, histerectomía obstétrica precedida de ligadura bilateral de las arterias hipogástricas es una alternativa terapéutica a considerar en casos de percretismo placentario.
Placenta percreta is defined as the abnormal insertion of chorionic villi in the myometrium, in the absence of decidua basalis and Nitabuch's1 fibrinoid layer that, depending on the degree of penetration, is classified as placenta acreta (78% of cases), which reaches the myometrium but does not invade it; placenta increta (17% of cases), which invades the myometrium, and finally placenta percreta (5% of cases), in which the chorionic elements penetrate and pass through the serous layer of the uterus and may reach neighbouring organs.2
Placenta acreta may lead to massive obstetric haemorrhage, with haemodynamic decompensation and eventually death, making it a public health problem. The World Health Organisation recently described placenta acreta as a new pandemic that is directly associated with patients with a history of 2 or more previous cesarian sections. In Mexico the rate of cesarian sections has gradually increased to levels above 36% in 2012, as a result of which the number of cases of placenta acreta has also increased.3
The American College of Obstetricians and Gynaecologists indicates that, if data exist that lead to a suspicion of placenta acreta certain measures should be taken to optimise birth and treatment, to reduce the risk of maternal morbimortality. These measures include:
- 1.
Warning the patient of the risks of hysterectomy and blood transfusion.
- 2.
A reserve of hemoconcentrates must be available.
- 3.
A suitable place for the resolution of the pregnancy must be available, in terms of its staff as well as its facilities.
- 4.
Previous evaluation by anaesthesiology.
- 5.
If necessary, the pelvic arteries can be embolised as an alternative to hysterectomy or to reduce blood loss in the latter.4
This clinical case aims to present the clinical and surgical evolution of a patient diagnosed placenta percreta, with invasion of the bladder and rectosigmoid, treated in the Gynaecology and Obstetric Intensive Care Unit of the Hospital General in México.
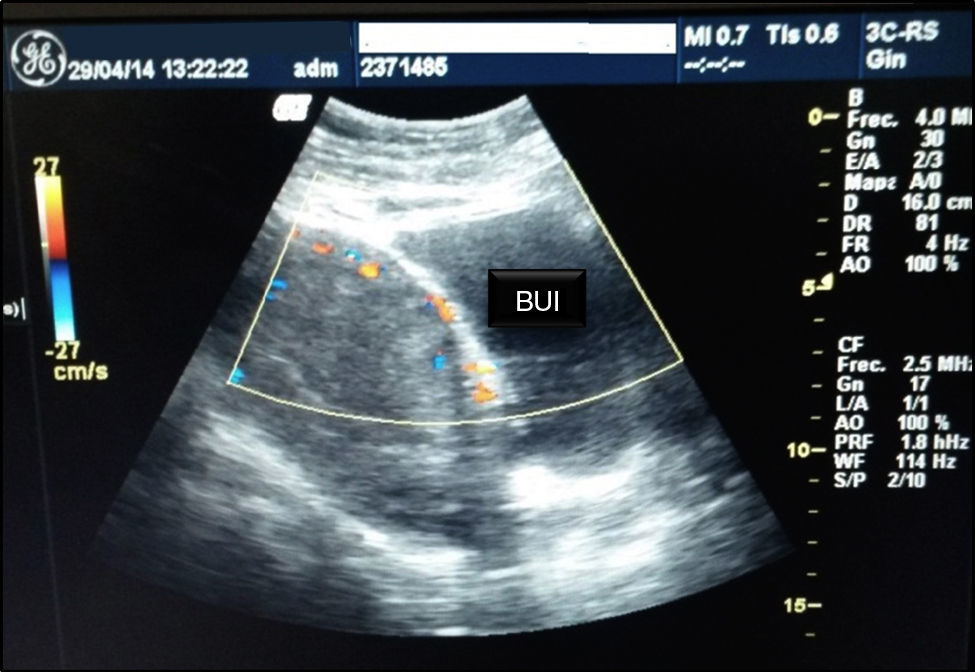
Clinical caseA 28-year-old female patient who had previously undergone several pregnancies and who was admitted to the Gynaecology and Obstetric Intensive Care Unit of the Hospital General in México, after referral by the Hospital Materno Infantil of the State of México (Toluca). She had a history of: 4 pregnancies, with 2 normal births (7 and 5 years previously) and one caesarean section (9 years previously, due to the umbilical cord wrapping round the foetus) and the diagnosis of pregnancy at 28.4 weeks by ultrasound scan in the second three-month period, haemorrhage in the second half of the pregnancy, anaemic syndrome under treatment, a previous totally occlusive placenta, placenta percreta up to the bladder and sigmoid rectum. The previous placenta study was included, with: Doppler ultrasound cystoscopy and nuclear magnetic resonance, showing involvement of the bladder and rectosigmoid (Fig. 1); at the same time treatment with foetal pulmonary maturity inductors commenced. Doppler ultrasound scan also showed previous placenta body and previous total placenta, with pelvic presentation, placenta acreta and percreta to the bladder and sigmoid rectum. Cystourethroscopy reported premeatal sentinel vessel, right lateral with serous membrane involvement, 2–3cm and pulsatile; left posterolateral wall with large calibre sentinel vessel in the left lateral wall without involvement of the bladder dome, with placenta percreta to the bladder.
Interruption of the pregnancy by cesarian section was planned, under peridural conduction anaesthesia. During the surgical procedure medusa head infiltration of the placenta that compromised the bladder dome, the broad ligament in its right thickness and the posterior fundus of the sac was found. Classical hysterotomy was performed in the fundic region resulting in a single male foetus weighing 1kg and 34cm in size, Apgar 5/6, Capurro 31.5 weeks. The umbilical cord was sutured with 1/0 silk and re-inserted in the uterine cavity. Single plane hysterorrhaphy was carried out using 1/0 chromed catgut. The patient was immediately taken to the Interventional Radiology department for the selective embolisation of the uterine arteries with gelfoam, and 100% of them were embolised (Figs. 2 and 3).
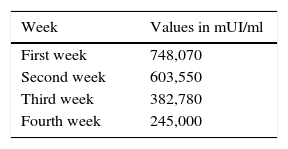
Following the third day after the cesarian section 80mg IV of methotrexate was administered weekly in 4 consecutive doses. Levels of human chorionic beta subunit gonadotropin were also monitored, with an initial figure of 598.960mUI/ml (Table 1).
A slight increase was detected in bilirubin levels after the final dose of methotrexate had been administered, when total bilirubin levels were found to be 1.32mg/dl, indirect bilirubin was 0.92mg/dl and direct bilirubin was 0.40mg/dl.
After 32 days of hospitalisation the patient was hemodynamically stable and quantitative levels of human chorionic beta subunit gonadotropin were below 250mUI/ml and Doppler ultrasound scan showed a significant reduction in bladder and uterine circulation (Fig. 4), so that it was decided to perform a second surgical operation to carry out a total obstetric hysterectomy.
To reduce the risk of bleeding during surgery a ligature was first applied to the hypogastric arteries using the GALA technique, after which the classical surgical technique was performed, corresponding to obstetric hysterectomy. Surgical findings showed a 90% reduction in infiltration by medusa head placenta towards the dome of the bladder, the broad ligament and posterior sac fundus. Total estimated bleeding amounted to 1800ml, so that two globular concentrates were transfused.
The patient was monitored for a further 24h for multiple parameters in the Obstetric Intensive Care Unit before being moved to the Perinatology Department, from where she was discharged without complications.
DiscussionThe phenomenon of invasion of the bladder and adjacent structures almost always occurs in patients with totally occlusive placenta previa and a history of one or more previous cesarian sections.5 Thanks to the introduction of new diagnostic methods such as Doppler ultrasound scan, magnetic resonance imaging and cystoscopy, the diagnosis of placenta acreta, increta or percreta may be carried out in an opportune manner before the end of gestation.6 Although total obstetric hysterectomy is universally accepted,7 the emergence of new techniques to treat symptoms such as the angioembolization of the uterine arteries and the use of chemotherapeutic agents such as methotrexate are alternatives for the safer management of placenta acreta.
Angioembolization of the uterine arteries is performed with the aim of reducing the risk of surgical bleeding,8 which is often associated with the ligation of the hypogastric arteries.
Methotrexate is a chemotherapeutic medication which is classified as a folate antagonist. It is used in placenta acreta due to its action against proliferative trophoblasts, although it is said that, following birth, it loses its usefulness given that the placenta ceases to be biologically active. Nevertheless, research works published by authors such as Arulkumaran et al. in 1986,9 followed by Mussalli et al. in 200010 raise doubts about these hypotheses.
ConclusionProtocol-governed and sequential management including the selective embolisation of the uterine arteries immediately following cesarian section with the placenta in situ, chemotherapy with methotrexate and, finally, obstetric hysterectomy after bilateral ligation of the hypogastric arteries is a therapeutic alternative to be considered in cases of placenta percreta.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Tórrez-Morales F, Briones-Garduño JC. Percretismo placentario con invasión de vejiga y recto. Cir Cir. 2017;85:66–69.