Among the rarest types of cancer found are the small intestine malignancies, representing only 2% of all gastrointestinal cancer and 0.1–0.3% of all malignancies. The most common subtype of this tumour is the adenocarcinoma, which is located mainly in the duodenum, jejunum and, rarely, in ileum.
Clinical caseA 75-year-old male, with no surgical history, who in the previous three months, referred to two clinical episodes of partial bowel obstruction and unquantified weight loss. When admitted into the surgical service, the patient referred to a partial bowel obstruction of more than one-week onset. A laparotomy was performed, finding three stenosis rings at the ileum end portion, carrying out an intestinal resection and enteral-enteral anastomosis. On the seventh day there was dehiscence of the anastomosis and abdominal sepsis. New surgery was performed with the resection of the intestinal anastomosis and an ileostomy. The pathologist report indicated a small bowel adenocarcinoma moderately differentiated, ulcerated, and multifocal. It was classified as stage III or T3N1M0. The patient progress was satisfactorily managed as outpatient with postoperative chemotherapy with five fluorouracil and cisplatin. The patient died a year later due to liver metastases.
ConclusionsDue to the extreme rarity of the case, it is very likely that general surgeons may find one or two cases of adenocarcinoma of the ileum in their professional career. Thus, they must suspect this pathology when faced with an episode of intestinal obstruction in the adult.
Entre los tipos de cáncer poco frecuentes encontramos las neoplasias malignas de intestino delgado, que representan el 2% de todas las neoplasias del sistema gastrointestinal y el 0.1–0.3% de todas las neoplasias malignas. De estas, el subtipo más frecuente es el adenocarcinoma, con su principal localización en duodeno, yeyuno y, con menor frecuencia, en íleon.
Caso clínicoVarón de 75 años de edad sin antecedentes quirúrgicos, quien refiere en los 3 meses previos haber presentado 2 cuadros de suboclusión intestinal y pérdida ponderal no cuantificada. A su ingreso al servicio de Cirugía muestra suboclusión intestinal de una semana de evolución. Se realizó laparotomía exploradora, mediante la cual se localizaron 3 estenosis anulares en íleon terminal; se realizó resección intestinal con entero-entero anastomosis. Al séptimo día se presentó dehiscencia de la anastomosis con sepsis abdominal, por lo que se efectuó una nueva cirugía con resección de la anastomosis intestinal e ileostomía. El estudio de anatomía patología reportó adenocarcinoma de intestino delgado moderadamente diferenciado, ulcerado y multicéntrico. Clasificación: estadio III o T3N1M0. El paciente presentó una evolución satisfactoria y se decidió su manejo ambulatorio con quimioterapia postoperatoria con 5-fluorouracilo y cisplatino. Fallece al año de postoperado por metástasis hepáticas.
ConclusionesPor la rareza del caso, es probable que los cirujanos generales atiendan en su vida quirúrgica uno o 2 casos de adenocarcinoma de íleon, por lo tanto, siempre que se enfrenten a un cuadro de suboclusión intestinal en el adulto deben sospechar esta dolencia.
Among the rare types of cancers are malignant neoplasms of the small intestine. Although these account for 75% of all the digestive tract and 90% of the mucous surface, these neoplasms only occur in 2% of all carcinomas of the gastrointestinal system, thus accounting for 0.1–0.3% of all malignant neoplasms.1–4 In the United States, these account for 0.46% of all malignancies of the small intestine, while in South Korea they account for 0.35%.5 These tumours more commonly occur during the sixties and more frequently in male patients, without any marked differences regarding gender.6–9
Of these neoplasms, the most frequent subtype is the adenocarcinoma, which accounts for 40–50% of the cases. It is mainly located in the duodenum and jejuno, and it is rarely located in the ileum.4,10 It appears as an annular, nodular or ulcerated strenuous lesion, irregular and eccentric, with prominent borders that are abruptly continued in the mucosa, which may cause partial intestinal obstruction. It is frequently located near Vater's ampulla, so it may begin with obstructive jaundice.9
The presence of multiple primary tumours in a patient is currently a very commonly diagnosed clinical condition. Therefore, multiple primary tumours refer to neoplasms present in a subject in a simultaneous or consecutive manner, provided they meet the following criteria: (1) each tumour must have a defined malignancy pattern; (2) rule out the possibility of it metastasising from another tumour; (3) each tumour should have a different histology; if both are similar within the same organ, it must be demonstrated that there is no connection between them; (4) each tumour must follow its natural course; (5) they may have independent progressions; and (6) if their diagnosis is simultaneous or if it is made within the first 6 months, they are considered synchronous; if their diagnosis is consecutive, they are considered metachronous. A little more than 37% are multicentric tumours occurring in the same organ. Multifocality is defined as the presence of two or more tumour foci in the same area, located less than 5cm from the primary focus, while multicentricity is the presence of two or more tumour foci in different sites, located more than 5cm from the primary focus.10,11 However, synchronous primary tumours are not very frequent.11
The primary adenocarcinoma of the small intestine located in the terminal ileum represents a challenge, given its rare nature. It is associated with a non-specific symptomatology and with its location, which hinders its visualisation by conventional endoscopy. This delays its timely diagnosis and treatment, which leads to a poor prognosis.1–3,5,10–14 Frequently, these tumours are detected in emergency surgeries conducted due to complications of the tumour itself, such as intestinal obstruction, perforation and haemorrhaging.14
The symptomatology is scarce and non-specific in the initial stages of the disease and mainly involves gastrointestinal symptoms (nausea, vomiting and postprandial fullness). This is due to its anatomy, given that the small intestine is difficult to examine. The most important symptoms in these cases involve weight loss, abdominal pain (52% of patients) and intestinal occlusion or subocclusion (36% of patients).13
Nevertheless, there are now more specific studies to obtain a diagnosis in earlier stages.14 A clear relation between the increase in tumour markers and the adenocarcinoma of the small intestine has not yet been established.2 Cases of an increase in the CA19-9 marker and carcinoembrionary antigen have been reported, although this increase has not yet been associated with the prognosis. However, an association between the increase in the CA19-9 marker and the tumour invasion of the peritoneum does exist.2 The intestinal disease analysis is still based on radiology, and intestinal transit method is one of the most commonly used methods. Other promising studies include the Doppler ultrasound with intravenous contrast material, which reveals the lesion blood supply, distribution and structure.15 The computed tomographic enteroclysis is a helical procedure with multiple detectors that allows for an adequate distension and visibility of the small intestine.15 The endoscopic capsule overrides the disadvantages of the conventional endoscopy and explores almost the entire small intestine without insufflation. This considerably improves the diagnosis and visibility of lesions and also confirms the diagnosis in patients who have previously undergone conventional radiological studies which revealed apparently normal results. The double-balloon enteroscopy allows for the assessment of the small intestine through an antegrade and retrograde exam, which results in visibility of the entire intestine.16–18
For its treatment, an open examination and a laparoscopy are ideal options for the surgical management when surgery is mandatory, such as in patients with full intestinal occlusion, with signs or symptoms that indicate strangulation or perforation, or in patients with unresolved subocclusion 24 or 48h following non-surgical medical treatment.4 On diagnosis, almost 40% of tumours are irresectable due to their metastases, thus reducing the surgical curative percentage to 67% of the total cases, and surgery is simply palliative in the remaining cases.2 Occlusion in the cases of primary or secondary carcinomas is not resolved by implementing a conservative treatment, and surgical intervention is always indicated.4 The objective of the surgical treatment of small intestine cancer is its broad resection, including regional lymph nodes, with potentially curative intention. In stage III cancers, if the lesion is located near the ileocecal valve, a laparoscopically assisted right hemicolectomy is recommended, with full resection of the tumour through a lymphadenectomy, so as to avoid recurrence or metastases. This objective has an impact on the prognosis, but not all patients will have a considerable life expectancy.19
The effectiveness of chemotherapy and radiotherapy has not yet been demonstrated. Nevertheless, in advanced-stage patients, with inoperable metastases or adenocarcinoma, these techniques improve life expectancy. There is not much experience with adenocarcinomas. Chemotherapy treatments are used with other tumours, such as colon cancers, such as 5-fluorouracil combined with leucovorin, irinotecan and oxaliplatin, as well as organoplatin agents, tyrosine kinase inhibitors (imatinib mesylate) or multikinase inhibitors (sunitinib).1–3,5–17,20–24 Recent studies show a capecitabine-based regime combined with oxaliplatin to improve treatment response and obtain a longer life expectancy in advanced-stage patients.25 Several retrospective studies have assessed adjuvant chemoradiation therapy followed by adenocarcinoma resection, but it has not yet been demonstrated that adjuvant treatment provides a benefit. However, it may be used as a palliative treatment for pain or obstructive symptoms. It has also been observed that it offers benefits for the control of chronic blood loss related to the tumour.
Clinical caseA 75-year-old male patient with two symptoms of intestinal subocclusion and non-quantified weight loss 3 months before his admission. When admitted to the Surgery Department, he presented one-week progression abdominal pain in the form of intense colics, and vomiting with food content, who denied having obstipation but did confirm the presence of constipation. After conducting a physical examination, the following findings were obtained: thin, non-icteric, regularly hydrated patient. Vital signs: blood pressure: 110/80mmHg; pulse: 86bpm, respiration: 20rpm; temperature: 36.5°C; weight: 64kg; stature: 1.64m. Neck with positive jugular ingurgitation. Distended abdomen, with generalised tympanism, pain on superficial and deep palpation, without decompression pain, hydro-aerial noises, without megalia. Lab results upon admission were as follows: glucose 122mg/dl; urea 57mg/dl; creatinine 1.1mg/dl; blood urea nitrogen (BUN) 26.6mg/dl; total cholesterol 153mg/dl; triglycerides 237mg/dl; haemoglobin 9.2g/dl; haematocrit 27%; leukocytes 10,500; neutrophils 88%; lymphocytes 9%; segmented neutrophils 78%; platelets 716,000; total bilirubin 0.93mg/dl; indirect bilirubin 0.70mg/dl; direct bilirubin 0.23mg/dl; oxaloacetic glutamic transaminase 50U/l; pyruvic glutamic transaminase 56U/l; alkaline phosphatase 147U/l; total proteins 7g/dl; serum albumin 4.6g/dl; albumin-globulin ratio 1.9g/dl; the general urine test was normal. Carcinoembrionary antigen 4.81ng/dl; prostatic antigen 1.9ng/dl; alpha fetoprotein 2.8ng/ml. The simple abdominal X-ray showed an image of intestinal occlusion with distended small intestinal loops and hydro-aerial levels, with air in the rectum ampulla (Fig. 1).
The patient was diagnosed with paraneoplastic syndrome with symptoms of intestinal occlusion.
The colon X-ray through an enema was reported as normal. The abdominal ultrasound showed a normal liver, without presence of metastasis, with considerable intestinal distension and no indication of the cause of the intestinal obstruction.
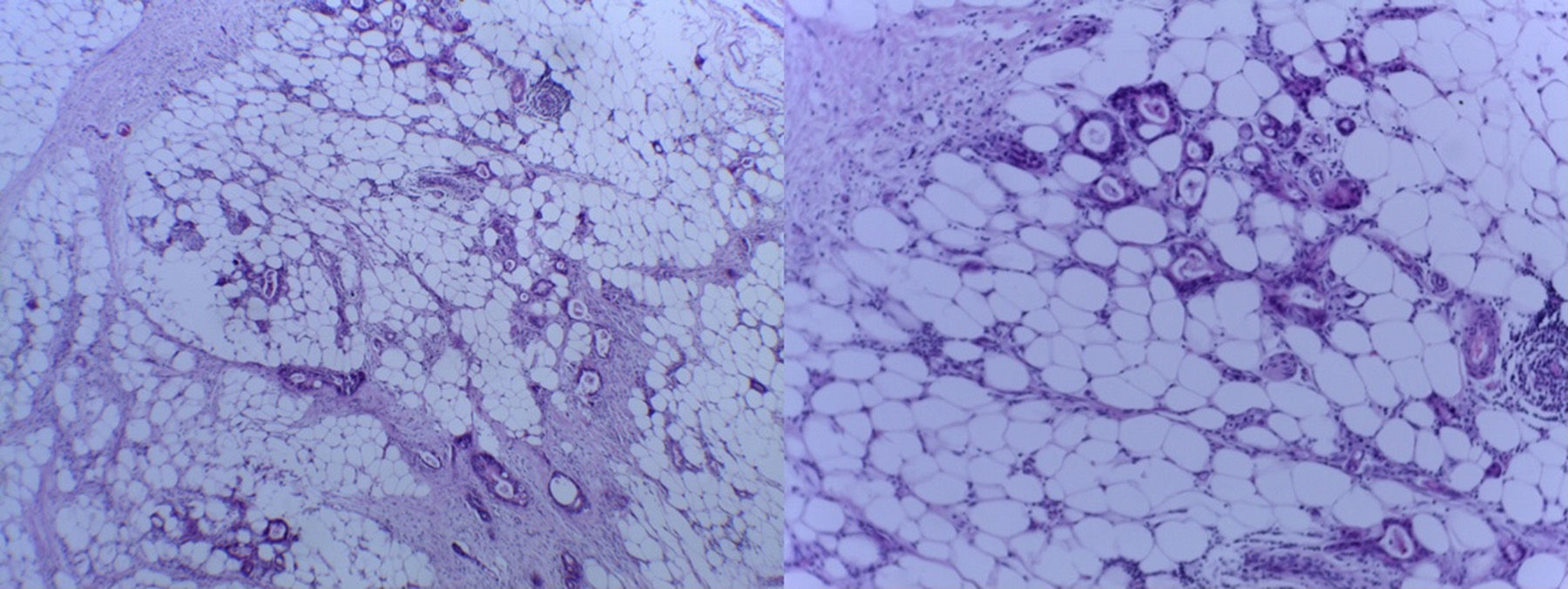
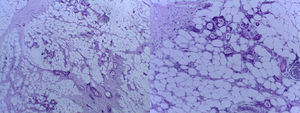
Medical care was provided during 48 hours, without any improvement in the intestinal subocclusion syndromes. Therefore, the first surgical team decided to perform an exploratory laparotomy. Upon examining the small intestine, three annular stenoses were found in the terminal ileum (Fig. 2), at 40, 70 and 100cm from the ileocecal valve, respectively, with findings of unclear and non-foetid serohaematic free fluid, without palpable lymph nodes and liver without metastasis. After the collection of these findings, the following procedures were performed: an en-block intestinal resection of the three stenoses, termino-terminal anastomosis of the intestine at 20cm from the ileocecal valve, and placement of two Penrose-type drains. In the macroscopic cut of one of the stenoses, tissue with fish-meat characteristics was observed in the mesenteric border (Fig. 3). One week after the surgical intervention, there was biliary output due to the Penrose drain, so a new exploratory laparotomy was performed by our surgical team. In this case, the anastomosis microscopic dehiscence was located, with presence of localised peritonitis. Thus, the anastomosis was resected, the terminal ileum was closed with Hartmann's pouch, and an ileostomy was performed.
The histopathological study revealed the following: moderately differentiated adenocarcinoma of the small intestine, ulcerated, multifocal, peritumoural adipose tissue infiltration, with tumour-free surgical limits, 22 peritumoural lymph nodes with sinusoidal hyperplasia and two with tumoural activity. Thus, the patient was diagnosed with adenocarcinoma of the small intestine, with presence of omental metastasis (Fig. 4). The cancer staging was stage III or T3N1M0. During the following 10 days, the patient was treated with oxygen therapy, antibiotics therapy, parenteral fluids and parenteral nutrition. He was discharged 17 days after his admission and continued with ambulatory treatment in the Medical Oncology Department using 5-fluorouracil and cisplatin. The patient died one year later due to hepatic metastases.
DiscussionIt is very common for general surgeons to provide treatment by primary intention to patients with symptoms of intestinal subocclusion or occlusion, and, although these are rare, gastrointestinal carcinomas are generally detected in very advanced stages, as shown in this case.4 The following oncological principles must always be taken into account to provide a better life expectancy to patients: (1) order a transoperative histopathological study; (2) request support from an oncological surgeon if the presence of a neoplasm is confirmed; and (3) request an examination of tumour markers, which are necessary for patients’ follow-up.
In the case of terminal ileum adenocarcinoma neoplasms, the age and gender of patients must be taken into account, given that there is a higher distribution in male patients older than sixty years old.6–9 The ileum is a very rare location, and the symptomatology is non-specific, but weight loss is a pathognomonic sign of tumour disease. In this case, the surgical management was performed without oncological criteria, given its non-specific initial symptoms, which included the following: three symptoms of intestinal subocclusion and weight loss (which was not quantified for this case). The manifestation of the lesion for this case coincides with that described in the medical literature, as it appears as an annular, ulcerated and irregular strenuous lesion, continued in the mucosa, which caused partial intestinal obstruction symptoms. The exceptional presentation of the case is the primary and synchronous existence of three tumours at 30, 70 and 100cm from the ileocecal valve. The above-mentioned risk factors for the development of intestinal neoplasms include: Crohn's disease, familial adenomatous polyposis, coeliac disease, type II Lynch syndrome, Peutz-Jeghers syndrome, peptic ulcer, cystic fibrosis and Schistosomiasis japonicum.4,20,21 In some patients, there was an increase in the CA19-9 antigen or carcinoembrionary antigen; in our patient, we ordered a test for the carcinoembrionary antigen, which showed a normal result, while a CA19-9 antigen test to supplement the diagnosis and follow-up is yet to be ordered. To analyse the small intestine disease using radiology, simple abdominal X-ray tests were performed in this case, which provided intestinal occlusive data with no other relevant sign. The contrast study and ultrasound reported no apparent or metastatic changes. On suspicion of paraneoplastic symptoms, the surgical management was chosen, since it is the recommended approach when there is no improvement using medical management.4 Based on the findings, the transurgical objective was broad resection, including regional lymph nodes, with potentially tumour curative intention. In stage III, as shown in this case, and given that the tumour was close to the ileocecal valve, a laparoscopically assisted right hemicolectomy was recommended, with full resection of the tumour through a lymphadenectomy, so as to avoid recurrence or metastatses.19 The complication arising from intra-abdominal sepsis due to dehiscence in the entero anastomosis was resolved with an ileostomy (This is an expected complication due to malnutrition in this type of patient). Due to its presentation, the chances of hepatic metastases were higher. Thus, the surgery performed had to be more radical. Our Medical Oncology Department used a 5-fluorouracil and cisplatin scheme, thus achieving a one-year life expectancy, and the cause of death was hepatic metastases. Other retrospective studies have assessed the adjuvant chemoradiation with resection of the duodenum adenocarcinoma without yet showing any benefits, except for the palliative treatment of pain and obstructive symptoms.
The prognosis for these patients is correlated with age, tumour site, clinical stage, lymph node metastases, performance of surgical resection and positive surgical margins. Negative surgical margins after surgery improve the prognosis.
It was decided to publish this case due to the low frequency with which this disease occurs and the lack of references in the national bibliography.
ConclusionThe adenocarcinoma of the small intestine is a rarely occurring malignant neoplasm. It is mainly located in the duodenum and jejuno, and less frequently located in the ileum, and multiple synchronous or metachronous tumours can be found. Because of the low frequency of the case, it is very likely that active general surgeons may treat only one or two cases of ileum adenocarcinoma in their surgical life. Therefore, on symptoms of partial intestinal obstruction in an adult, this condition must be suspected. Likewise, it is important to refer these patients to a surgical oncologist with more experience in such a condition to avoid incomplete surgeries and achieve a better life expectancy.
An examination of the entire small intestine should also be performed during surgery in case there is more than one tumour.
Conflict of interestThe authors declare that there are no conflicts of interest.
To Dr. Raúl Candia García, radiologist, teacher, good man and an excellent father, committed to teaching, may your wise advice be reflected in this article, your last one.
Please cite this article as: Candia-de la Rosa RF, Sampayo-Candia R, Bretón-Toral JC, Candia-Archundia F, Candia-García R. Adenocarcinoma primario y sincrónico de íleon terminal. Cir Cir. 2015;83:232–7.