There are barriers and enablers for the implementation of rapid response teams in obstetric hospitals. The enabling factors were determined at Instituto Mexicano del Seguro Social (IMSS).
Materials and methodsAn observational, retrospective study was conducted by analysing the emergency obstetric reports sent by mobile technology and e-mail to the Medical Care Unit of the IMSS in 2013. Frequency and mean was obtained using the Excel 2010 program for descriptive statistics.
ResultsA total of 164,250 emergency obstetric cases were reported, and there was a mean of 425 messages per day, of which 32.2% were true obstetric emergencies and required the rapid response team. By e-mail, there were 73,452 life threatening cases (a mean of 6 cases per day). A monthly simulation was performed in hospitals (480 in total).
Enabling factors were message's synchronisation among the participating personnel, the accurate record of the obstetrics, as well as the simulations performed by the operational staff.
The most common emergency was preeclampsia–eclampsia with 3351 reports, followed by obstetric haemorrhage with 2982 cases.
DiscussionThe enabling factors for the implementation of a rapid response team at IMSS were properly timed communication between the central delegation teams, as they allowed faster medical and administrative management and participation of hospital medical teams in the process.
ConclusionMobile technology has increased the speed of medical and administrative management in emergency obstetric care. However, comparative studies are needed to determine the statistical significance.
Los Equipos de Respuesta Inmediata hospitalarios tienen factores obstaculizadores y facilitadores. Se determinó la participación de estos últimos en el Instituto Mexicano del Seguro Social (IMSS).
Material y métodosEstudio observacional, retrospectivo de reportes de urgencia obstétrica enviados por tecnología móvil y correo electrónico a la Unidad de Atención Médica del IMSS durante 2013. Se utilizó el programa Excel 2010 para estadística descriptiva.
ResultadosUn total de 164,250 mensajes se recibieron (promedio 425 mensajes/día); el 32.2% correspondió a urgencia obstétrica que requirió apoyo de los Equipos de Respuesta Inmediata Directivo-Delegacional-Central. Por correo electrónico, hubo 73,452 casos de morbilidad obstétrica extrema (promedio de 6 casos/día). Se realizaron en total 480 simulacros (uno/mes) en los hospitales.
Los factores facilitadores fueron la oportuna sincronización de los mensajes entre los directivos de los diferentes niveles de mando, el registro preciso de la urgencia obstétrica y los simulacros realizados por el personal operativo.
La urgencia obstétrica más común fue preeclampsia-eclampsia con 3,351 reportes, y hemorragia obstétrica con 2,982 casos.
DiscusiónLa sincronización adecuada de comunicación por mensajes entre el equipo de respuesta inmediata de los diferentes niveles de mando permitió mayor rapidez en la gestión médica-administrativa así como la participación del equipo médico hospitalario en el proceso de la atención de la urgencia obstétrica.
ConclusiónEl uso de la tecnología móvil en el funcionamiento del equipo de respuesta inmediata en el IMSS, ha permitido mayor rapidez en la gestión médico-administrativa en la atención de la urgencia obstétrica; sin embargo, es necesario realizar estudios comparativos para determinar la significación estadística.
Ensuring the women safety in pregnancy is a fundamental principal in all healthcare systems, and safety programmes are continuously being developed to that end.1 Doctors can be faced with emergency situations even if a pregnancy has progressed well, and therefore several strategies have been designed, such as hospital rapid response teams. The rapid response system has three components: (1) specific criteria for notifying and activating the response team; (2) the rapid response team; (3) the administrative and quality component.2
A metaanalysis in 2010 reported that there were some barriers to the implementation of rapid response teams, such as: a lack of activation criteria training on the part of the healthcare team, few simulations, a lack of interest on the part of staff to activate the team despite the existence of well-established criteria, changes in culture (asking for help without fear of criticism or rebuke on activating the team), and perceptions with regard to the usefulness of a hospital rapid response team.3
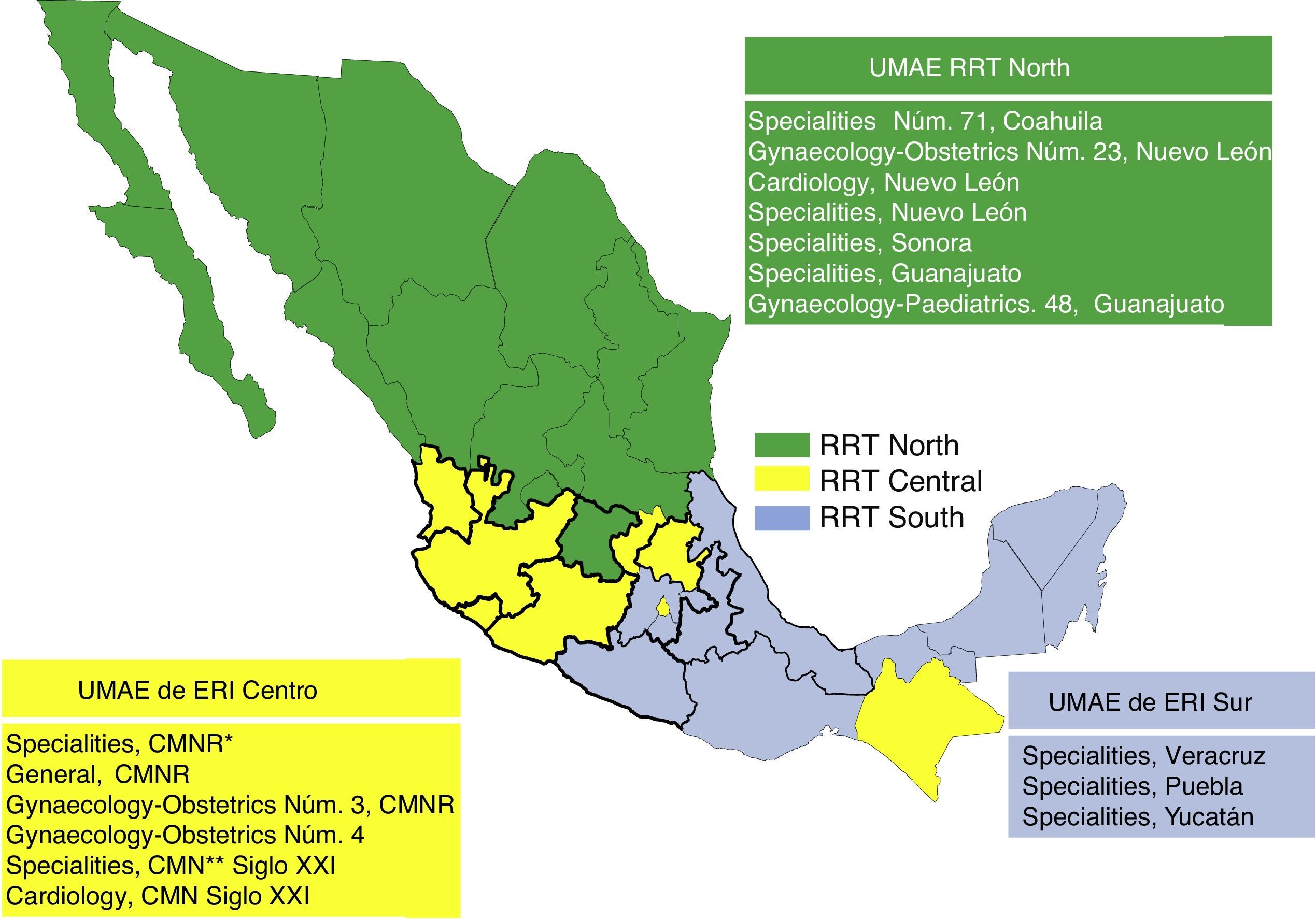
The Instituto Mexicano del Seguro Social (IMSS) (the Mexican Social Security Institute) implemented the hospital rapid response team in 2010; the mapping is shown in Fig. 1 (rapid response team, north, centre and south), however the enabling factors for it to function efficiently have not been established.
Mapping of the rapid response teams (RRT) at Instituto Mexicano del Seguro Social (IMSS). The High Speciality Medical Units (UMAE) which support obstetric care are shown in the respective boxes for each rapid response team. CMNR: “La Raza” National Medical Centre, CMN: National Medical Centre.
Therefore, our objective was to identify the factors which enable rapid response teams at IMSS obstetric hospitals to function correctly in 2013.
Materials and methodsA retrospective, observational, descriptive study was undertaken of the obstetric emergency reports from the period between 1 January and 31 December 2013. The variables studied were the obstetric emergency reports, and the number of simulations performed by rapid response teams in hospitals. The obstetric emergency reports came from the 35 delegations of the IMSS and the Unidades Médicas de Alta Especialidad (UMAE) (High Speciality Medical Units), 24h a day, all year, by means of mobile technology and e-mail, and were gathered in the Coordinación de Atención Integral en Segundo Nivel (Comprehensive Care Coordination at Second Level) of the Unidad de Atención Médica (Medical Care Unit). The number of rapid response team simulations performed in the hospitals during the same period was also recorded. The inclusion criteria were all the reports received from the different IMSS hospitals over the entire country. No exclusion criteria were considered, since all the reports were obstetric emergencies.
The information was entered on an Excel 2010 datasheet; descriptive statistics were made on the database through determining simple frequencies with central tendency and dispersion measures, and using simple frequencies, percentages and means.
Results- 1.
The number of mobile phone messages received was 164,250, with a mean of 425 messages per day; all of them were obstetric emergency cases which were resolved or awaiting resolution. Of that total, 32.2% were obstetric emergencies, which required the support of joint medical and administrative opinion from the central delegation rapid response teams.
The enabling factor found was the 100% medical-administrative synchronisation of the rapid response team of the central delegation managers.
- 2.
The number of medical cases recorded on the electronic report was 73,452 cases (new and follow-up) of women in the gravido-puerperal period whose lives were at risk (40 e-mails per day); the mean of serious cases sent by e-mail was 6 per day (Table 1).
Table 1.Obstetric emergency cases received in 2013.
Type Number Day Mobile technology (SMS messages)a 164,250 425 E-mail 73,452 6 Source: Registry of Obstetric Emergencies, Coordinación de Atención Integral en el Segundo Nivel. (Comprehensive Care Coordination at Second Level) IMSS.The enabling factor found was the 100% participation of operative and managerial hospital staff in sending the form.
- 3.
Four hundred and eighty rapid response team simulations were performed; the enabling factor was the 100% participation of medical and paramedical staff in meeting the goal of one simulation per month in each delegation and UMAE (High Speciality Medical Unit) (Fig. 1).
Of the obstetric pathologies reported, the most common was preeclampsia–eclampsia with 3351 reports, followed by obstetric haemorrhage with 2982 cases.
In 2013, 592,915 pregnant women had at least one medical consultation in the IMSS. Given this amount, a high comorbidity is to be expected (in the same year 15,439 cases of hypertensive disorders in pregnancy were recorded, and 2681 cases of placenta previa with obstetric haemorrhage, amongst other complications). The survival of these patients was determined by the severity of their acute condition on admission, the quality of care given, and the time interval between their admission and receiving care.4,5
Gosman et al.6 included various types of obstetric emergencies in their design (cord prolapse, foetal distress, and obstetric haemorrhage), and they identified the needs for implementing the team, the difficulties in application and the obstacles, but they did not compare the reduction in morbimortality before, and after the teams were formed. Whereas Skupski et al.7 focussed on the care of obstetric haemorrhage only. In their review, Barbetti and Lee8 found that education, resources, and communication are vital to the successful implementation of rapid response. In the IMSS, the use of mobile technology in its simplest form (message system) by the central delegation (UMAE) rapid response team has enabled swift management of resources, expert support, and more, in emergency obstetric care.
The enabling factors in this study coincide with those reported by other authors; principally the “paradigm shift” made by doctors, reflected by the 100% reporting of serious clinical obstetric cases and requesting, in some cases, support for transfer to more specialised hospitals, and the 100% establishment of the medical-administrative network between IMSS managers. There is greater participation on the part of hospital operational staff when they receive the support of the rapid response team management (for example, a daily report on the obstetric patients whose lives are at risk, and running simulations in their medical units).
Two factors which hinder the appropriate functioning of the rapid response team have been reported in medical literature: delayed decision-making on the part of the medical team in treating the obstetric emergency, and inadequate team formation, due to various factors; principally, the scarcity of human resources in the hospitals. The first factor can be improved by training the medical team on the diagnosis and treatment of the most common obstetric emergency in each setting: in our case, the correct diagnosis and treatment of preeclampsia–eclampsia and obstetric haemorrhage. The second factor requires an efficient and effective administrative process. The rapid medical-administrative support provided by the rapid response teams of the UMAEs, in obstetric emergency cases is essential to resolve said emergencies, therefore the use of mobile technology (text messages or SMS, termed “Chat ERI”) has greatly enhanced quality of care, particularly in critical situations (night shifts, weekends or medical units which are at a great distance from the large hospitals). As in worldwide medical literature, another enabling factor is running rapid response team simulations in the hospital units; this strengthens the standardisation of the teams, which should be permanent, in line with the features of each hospital.9
ConclusionTraining medical staff for the rapid response team should use the assessment of results as a platform to diagnose problems and create specific solutions. In order for a rapid response team to function well, good standardised criteria for implementation and auditing are required.
The use of mobile technology by rapid response teams senior management is essential for the appropriate management of resources for obstetric emergency care. A large network for the care of pregnant women, whose lives are threatened, has been created with this form of communication. This communication network in real time is useful, not only in the care of obstetric emergencies, but also in all other processes in the Mexican Health System.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Dávila-Torres J, de Jesús González-Izquierdo J, Ruíz-Rosas RA, Cruz-Cruz PDR, Hernández-Valencia M. Equipo de Respuesta Inmediata Obstétrico en el Instituto Mexicano del Seguro Social, factores facilitadores. Cir Cir. 2015;83:492–495.