Spontaneous cholecystocutaneous fistula is defined as a gallbladder communication with the external environment through the abdominal wall rupture. The first reports were written in the seventeenth century by Thilesus. During the past 50 years, 25 cases have been reported.
Clinical caseThe case is presented of a 30-year-old woman, who had a five-year history of biliary colic. Six months prior to her medical assessment there was a leak of biliary material and gallstones spontaneously in the right upper quadrant. Fistulogram was performed with no evidence of obstruction. A cholecystectomy and resection of the fistula was subsequently performed.
DiscussionThe biliary fistulas are an abnormal communication from the gallbladder into another surface. It is a rare condition nowadays, as it only occurs in 10% of patients with gallbladder lithiasis. Although the clinical signs of spontaneous cholecystocutaneous fistula clinic are more than evident, it is imperative to perform studies like ultrasound, tomography, and a fistulogram. The mainstay of treatment is cholecystectomy, resection of the fistula, and repair of abdominal wall defect.
ConclusionThe incidence of cholecystocutaneous fistula today is minimal and it seems that the current trend is to become an entity anecdotal. The subcostal abdominal examination approach remains as the first choice. The laparoscopic approach is an option reserved for the experienced surgeon.
Se define la fístula colecistocutánea espontánea como la comunicación de la vesícula biliar con el medio externo a través de la rotura de la pared abdominal; los primeros reportes escritos datan del siglo XVII por Thilesus. Durante los últimos 50 años, se han reportado 25 casos.
Caso clínicoSe trata de un paciente femenino, de 30 años, con cólico biliar de 5 años de evolución; 6 meses previos a su valoración, presenta salida de material biliar, así como litos, de manera espontánea en el hipocondrio derecho. Se realiza un fistulograma sin evidencia de obstrucción; posteriormente, se realiza colecistectomía, así como resección del trayecto fistuloso.
DiscusiónLas fístulas biliares son una comunicación anómala de la vesícula hacia otra superficie; es una patología rara en nuestros días, ya que solo se presenta en un 10% de los pacientes con colecistopatía litiásica, si bien la clínica de la fístula colecistocutánea espontánea es más que evidente, es indispensable realizar estudios complementarios, como ultrasonido, tomografía y fistulograma. La base del tratamiento consiste en la colecistectomía, así como en la resección del trayecto fistuloso y la reparación del defecto en la pared abdominal.
ConclusiónLa incidencia de fístulas colecistocutáneas en la actualidad es mínima y parece que la tendencia actual es a convertirse en una entidad anecdótica; la vía de abordaje para la exploración abdominal es la vía subcostal como primera opción. El acceso laparoscópico es una opción reservada para el cirujano experimentado.
Spontaneous cholecysto-cutaneous fistula is defined as the link between the gallbladder with the exterior by means of a rupture in the abdominal wall layers, all of which strengthens the fistulous tract. Even though there is evidence of the appearance of cholecysto-cutaneous fistulas, by putting the patient in ventral decubitus position in order to treat gallbladder disease, more than 2,000 years ago, the first written reports were found in the seventeenth century by Thilesus, who described this condition for the first time. Towards the nineteenth century, Courvoisier presented his series of 499 patients. During the past century, 70 cases have been reported and 25 of them in the last 50 years. Such tendency of reduction in the appearance of this nosologic condition is due to prompt diagnosis, as well as the development in the therapy used for treatment in the last two centuries. We submit the clinical case of a patient starting her fourth decade, with no prior medical history of the condition, who developed a long-term evolution cholecysto-cutaneous fistula.1–4
Clinical caseThe patient was a 30-year-old woman, with no chronic-degenerative or surgical history, with multiple pregnancies, who suffered from pain in the right hypochondrium of 5 years of evolution, treated as acid peptic disease. 6 months before the assessment, she presented a lesion of 2 cm in the right hypochondrium, characterised by increased volume and effusion of purulent material. She was treated in an ambulatory manner at the general medicine service as a probable cutaneous abscess with local dermatological management; however, after 3 months, the patient presented a spontaneous effusion of biliary material, as well as calculus, which suddenly connects the bile duct to the outside (Fig. 1).
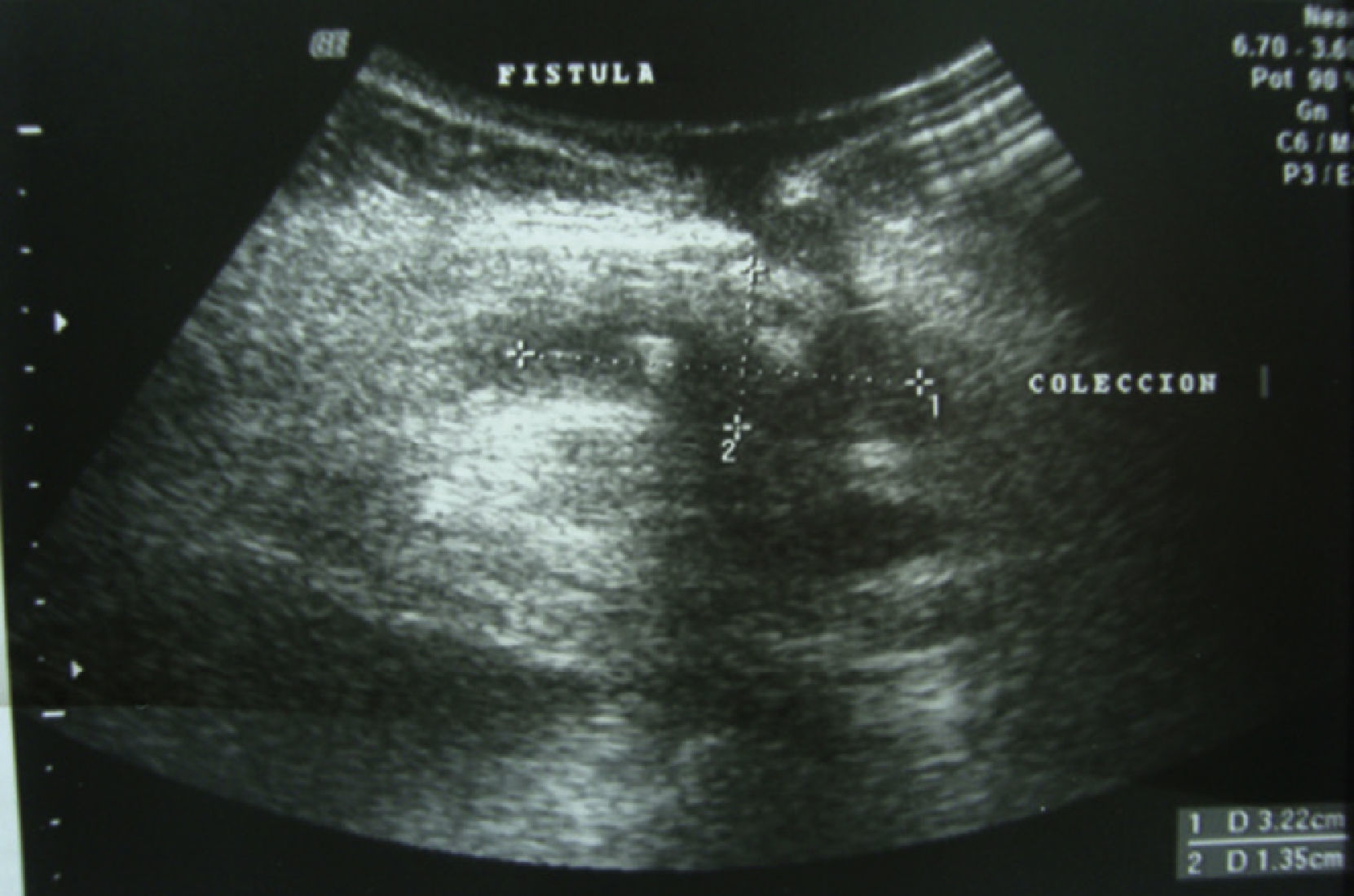
Subsequently, she returned for assessment at the general surgery service, where study protocol was initiated. She underwent an ultrasonography, with evidence of fistulous tract through abdominal wall thickness, and with collection at the subcutaneous cellular level (Fig. 2).
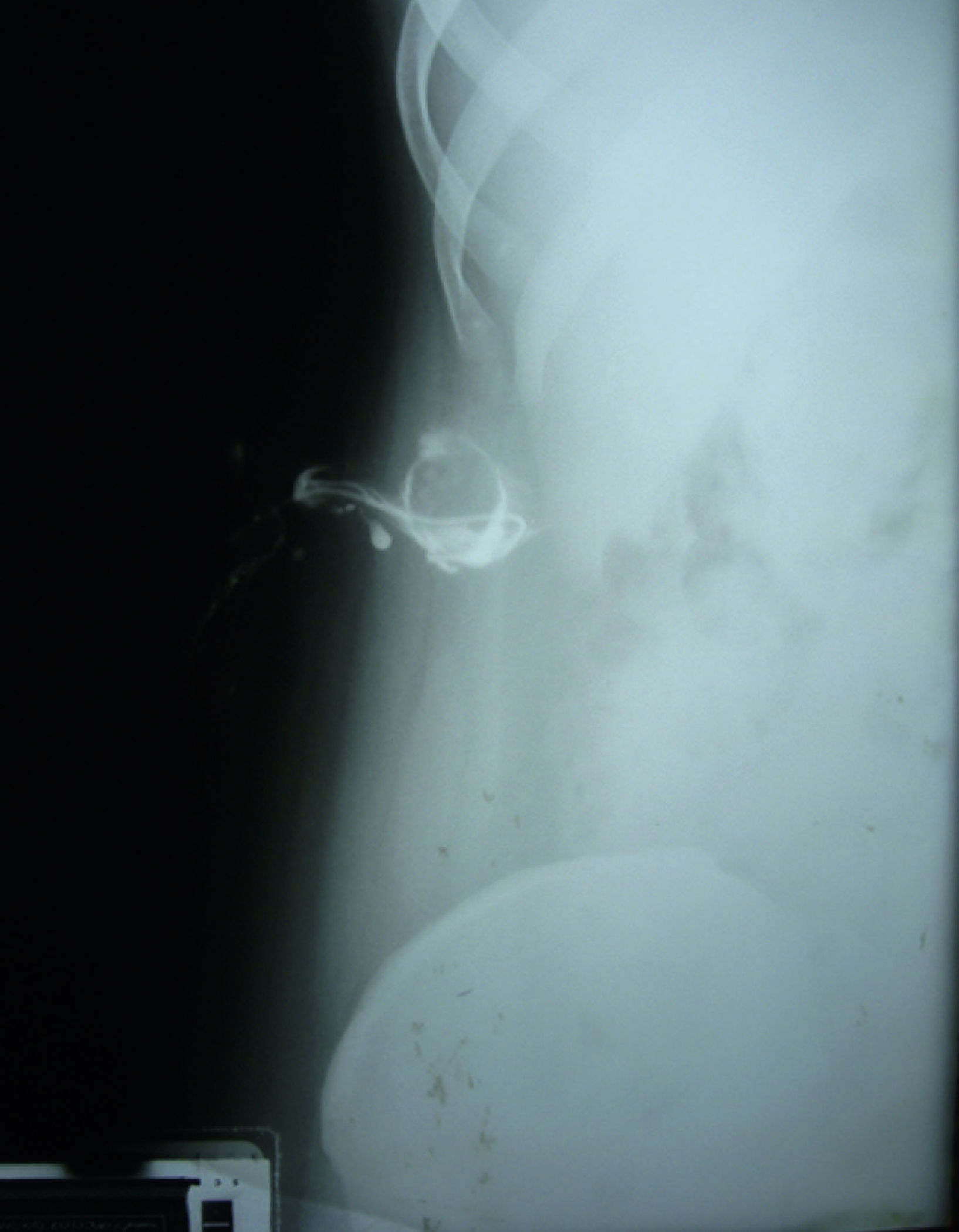
The tract was cannulated and a fistulography was performed, with presence of communication to the gallbladder, without obstruction of the bile duct (Fig. 3).
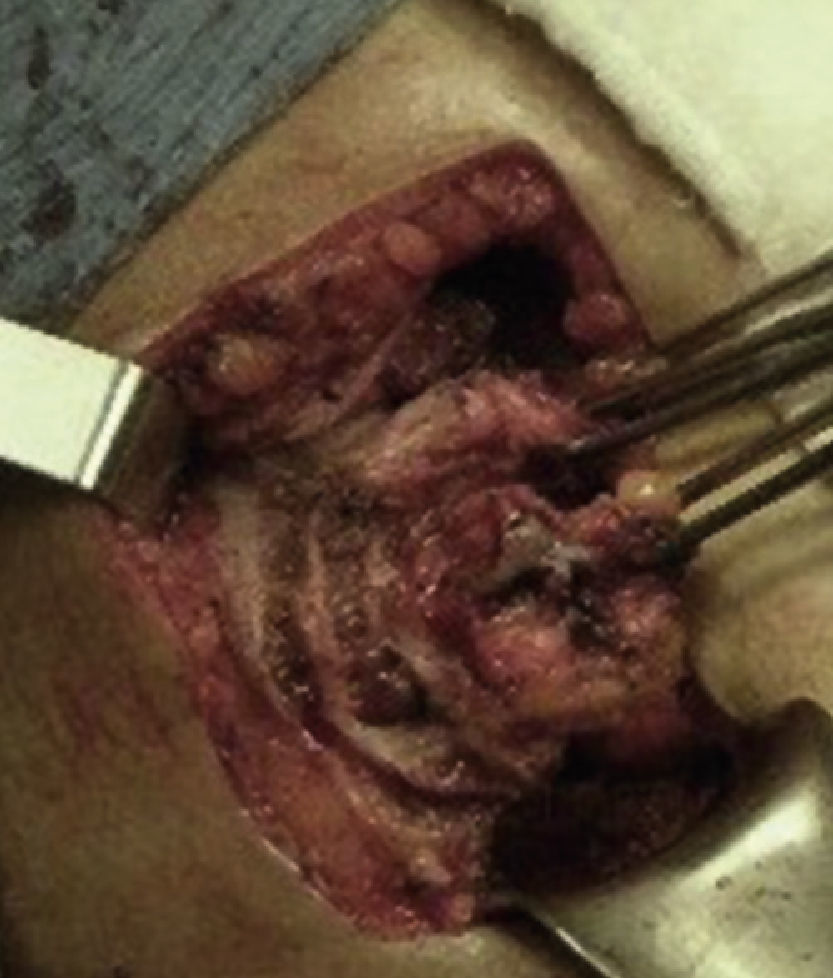
A surgical exploration was programmed electively using a Kosher approach. At subhepatic level, it was possible to observe gallbladder adherences to the colon wall, liver and greater omentum. A retrograde dissection of the gallbladder was conducted, drying the corresponding spindle of fistulous tract (Figs. 4 and 5). An exploration of the bile duct was carried out in a transcystic manner, without evidence of dilation or obstructions; the wound healed and the event concluded.
The patient presented satisfactory evolution, without postoperative complications and was discharged after 48hours. During medium and late postoperative, there was proper healing, with no information regarding complications to the procedure, and assistance finalised.
DiscussionSpontaneous biliary fistulas are anomalous connections of the gallbladder to another surface. It is a rare pathology nowadays, as it is only present in 10% of patients with gallbladder lithiasis. Despite the fact that such cases are few, they are predominant in female patients under 60 years.1,3
Biliary fistulas are classified into two groups: internal and external; the latter present communication to any part of the anterior surface of the trunk; however, they are extremely rare because, in recent decades, less than 100 cases have been reported in medical literature. In the case of internal fistulas, 75% are connected to the duodenum, 15% to colon and 10% to jejunum, stomach or bronchi.1,2
The appearance of cholecysto-cutaneous fistula has a diverse etiopathogenesis. Among the causes there are gallbladder neoplasia, anatomic anomalies and, of course, post-surgery causes. Nevertheless, most cases are associated to vesicular lithiasis, where the increase of intraluminal pressure compromises wall circulation, leading to ischemia, necrosis, bacterial translocation and, eventually, abscesses, which communicate to the abdominal wall. There is a greater association between the cholecysto-cutaneous fistula and the obstruction of the bile duct by calculus. However, our patient did not have that feature.1,3–6
Clinical presentation of spontaneous cholecysto-cutaneous fistula is an insidious condition, with long-term evolution, and biliary colic as a main feature that lasts years. Subsequently, there is also a cutaneous lesion that develops into an abscess in the right hypochondrium, right flank or even the umbilical scar, which, if there is no careful exploration and effective examination, can be treated as a dermatological pathology without success. Finally, once the tract is consolidated, the effusion of biliar material and calculus is added by means of the fistula.5,7–9
Even though the fistula clinic is more evident, it is very important to conduct extension studies, such as: ultrasound to establish bile duct characteristics, tomography to search for abscesses and, of course, a fistulogram in order to establish the lesion aetiology and the presence of bile duct obstructions.8,10–13
Cholecysto-cutaneous fistula management must be comprehensive; even though surgical management is the basis for treatment, conservative management must be considered, based on fluidtherapy and antimicrobials in those patients in which the overall condition is compromised during anaesthetic or surgical procedures. Likewise, if there is evidence of obstruction in the bile duct during the fistulogram, one of the options with less comorbility rate is the retrograde endoscopic choliopancreatography. That withstanding, we cannot set aside the fact that the patient should undergo surgical intervention as final therapy. The use of endoscopic retrograde cholangiopancreatography drains the bile duct, contributing to intraluminal pressure reduction in the gallbladder and reducing fistula wear.9,12,14–18
The surgical procedure consists of the cholecystectomy, as well as fistulous tract resection and repair of the abdominal wall defect. The fistulography establishes bile duct permeability, which should be verified during surgery according to the surgeon's criteria. The preferable approach is usually the conventional; that is to say, by means of a right subcostal incision, with spindle resection of the tract in the wall. Laparoscopy access is currently described. However, the process unleashed by the pathology is related to chronic and severe gallbladder inflammation. It also jeopardizes bile duct structures with minimal invasion.12,14,16,19,20
ConclusionsThere is currently a low incidence of cholecysto-cutaneous fistula and it seems that the current trend is for it to become an anecdotal condition. However, surgeons should keep it in mind by as one of the complications of biliary-related pathologies. Even though the efforts of health systems in establishing a prompt diagnosis and treatment for gallbladder diseases has accomplished the reduction of severe complications such as fistulation, in the lowest social strata of the population there is still a small percentage that does not have access to such benefits and that is referred to a surgical service with pathologies as described in this text.
There must be a preoperative comprehensive assessment that informs the fistula anatomy as a bile duct in order to stablish an optimal surgical plan. As regards the approach, abdominal exploration by subcostal means remains as the first option due to the ethiological features of the condition, and since laparoscopic access is an alternative reserved for expert surgeons, as well as the patience needed to treat the pathology comprehensively via this access.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Guardado-Bermúdez et al. Fístula colecistocutánea espontánea. Cirugía y Cirujanos. 2015; 83: 61-64.