Percutaneous nephrolithotomy remains the standard of care for kidney stones larger than 2cm. Therefore, setting a prognosis for complete stone resolution through this method is essential. The prognostic tools available have limited prediction.
ObjectivesTo evaluate the stone-free rate in patients undergoing percutaneous nephrolithotomy with the Clinical Research Office of the Endourological Society nomogram and suggest modifications to improve the classification.
Material and methodsWe analyzed a retrospective cohort of patients undergoing percutaneous nephrolithotomy applying the nephrolithometric nomogram specified. We modified the scale dividing the patients into 3groups: I from 80 to 110 points, II from 111 to 170 points, and III more than 170 points, respectively assessing the stone-free rate (Kruskal–Wallis test was performed, p<0.05).
ResultsA total of 126 patients were included. According to the nehrolithometric nomogram the stone-free rate was 12.5% for patients with fewer than 111 points and 70.9% for those with 111 points or more. In the modification proposed for groups I, II and III the stone-free rate was 12.5%, 50% and 80% respectively (p=0.000).
ConclusionsEvaluation using the nephrolithometric nomogram demonstrated accurate stone-free rate prediction for complex and simple stones, with a lack of discrimination for patients with intermediate scores. Our modification enabled better differentiation of the intermediate groups from the high and low stone-free rate groups.
La nefrolitotomía percutánea es la cirugía de elección para litos mayores de 2cm. El establecer un pronóstico para la resolución de la litiasis por este método es crucial. Las herramientas pronósticas propuestas hasta el momento presentan limitaciones predictivas.
ObjetivoEvaluar la tasa libre de litos por nomograma nefrolitométrico de la Clinical Research Office de la Endourological Society en pacientes tratados con nefrolitotomía percutánea y proponer modificaciones para mejorar la clasificación.
Material y métodosEvaluamos una cohorte retrospectiva de pacientes intervenidos mediante cirugía percutánea aplicando el nomograma nefrolitométrico especificado. Realizamos una modificación para mejorar su predicción dividiendo a los pacientes en 3grupos: I de 80 a 110 puntos, II de 111 a 170 puntos y III de más de 170 puntos, con el cálculo respectivo de tasa libre de litos (se realizó la prueba de Kruskall-Wallis p<0.05).
ResultadosSe incluyeron 126 pacientes. Por nomograma nefrolitométrico, la tasa libre de litos fue de 12.5% para pacientes con menos de 111 puntos y de 70.9% con 111 puntos o más. En la modificación propuesta para los grupos I, II y III la tasa libre de litos fue 12.5, 50 y 80%, respectivamente (p = 0.000).
ConclusionesLa evaluación con nomograma nefrolitométrico demostró predicción de la tasa libre de litos para litos complejos y simples, sin poder discriminar los pacientes con puntuaciones intermedias. Nuestra propuesta permite diferenciar mejor al grupo intermedio de los grupos de alta y baja tasa libre de litos.
Percutaneous nephrolithotomy (PNL) is the standard of care for stones larger than 2cm, for patients for whom extracorporeal lithotripsy has failed, and for those with specific anatomical conditions (horseshoe kidney, ectopic, calyceal diverticulum, etc.).1–3 A prognosis for resolution of the disease needs to be established; to that end, 3 tools to determine the stone-free rate (SFR) have recently been published.4–7 The last of these was developed by the Clinical Research Office of the Endourological Society, and proposes the analysis of 4 variables for the characteristics of the stone (size, location, number and presence of staghorn calculus), the clinical picture (previous treatment) and of another variable that evaluates the experience (number of cases attended in the centre where the procedure was undertaken). These variables are a summation and the final score crosses a line graphically that gives the SFR as a percentage. A 76% diagnostic accuracy is reported for this nomogram. However, predictions based on this nomogram are clinically useful if a 60% SFR threshold is applied to determine treatments auxiliary to PNL. At present, there are few series that have evaluated the application of this nomogram.8 The objective of this paper was to evaluate the capacity of the CROES nomogram to stratify patients treated with PNL according to SFR in our centre and to propose modifications to better differentiate the treatment response groups.
Material and methodsWith the approval of the local research committee, we assessed a cohort of 126 clinical records of patients diagnosed with kidney stones, who underwent NLP in our institution from December 2010 to January 2015, and who had a full medical history and sufficient radiographic tests to enable appropriate categorization according to the CROES nomogram.
An experienced urologist was asked to calculate the CROES nomogram score taking into account the 6 variables it uses to calculate SFR. The population was divided into 2 groups (SFR ≥60% and <60%) according to the original proposal of the CROES nomogram. In order to better distinguish the intermediate response group, we divided the population according to their CROES nomogram score and their corresponding SFR (score/SFR) into 3 groups: group I from 80 to 110/0% to 59%, group II 111 to 170/60% to 79% and group III more than 170/≥80%, in order to establish 3 prediction levels with at least 20% difference between them.
A SFR was considered when the radiographic studies (computed axial tomography or plain abdominal X-ray) revealed either no stones or stones smaller than 4mm (clinically insignificant). All patients who required treatment for kidney stones 90 days after the previous treatment were considered new kidney stone cases. Secondly, the operating time, blood loss, days of hospital stay and complications were assessed according to the modified Clavien scale.9 A comparative analysis was made between the groups using the Kruskal–Wallis test with the SPSS programme, the confidence interval was 95% (p<0.05).
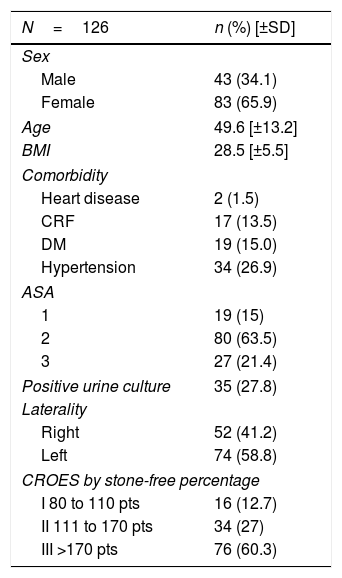
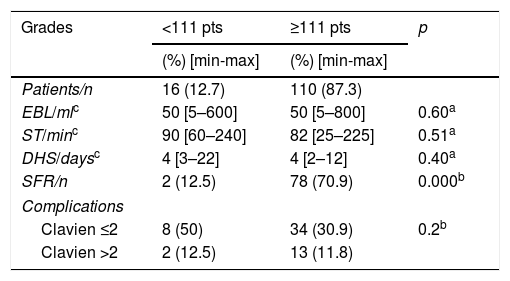
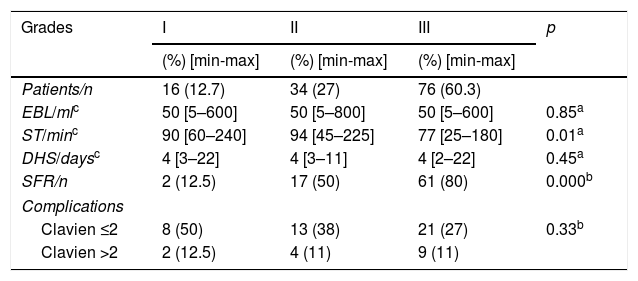
ResultsThe mean age was 49.6 years (±13.2), 65.9% were female and the overall SFR was 63.5% (Table 1). Using the CROES nomogram, 2 of the 16 patients of the <111 point group (SFR 12.5%), and 78 out of 110 patients from the ≥111 point group (SFR 70.9%) were stone-free (Table 2). According to our proposal: group I 2/16, group II 17/34 and group III 21/76 had an SFR of 12.5%, 50% and 80%, respectively (p=0.000). A difference in the surgery time between group III and group I was found (of 77 vs 90min, p=0.01). There was no difference between the groups in terms of complications (p=0.33), blood loss (p=0.85), days of hospital stay (p=0.45). The overall complications rate was 45%, and classified as follows: Clavien ≤2 (33%) and >2 (12%), the complications were stratified in the 3 groups, with no difference between them (p=0.33) (Table 3).
The patients’ clinical and demographic characteristics.
| N=126 | n (%) [±SD] |
|---|---|
| Sex | |
| Male | 43 (34.1) |
| Female | 83 (65.9) |
| Age | 49.6 [±13.2] |
| BMI | 28.5 [±5.5] |
| Comorbidity | |
| Heart disease | 2 (1.5) |
| CRF | 17 (13.5) |
| DM | 19 (15.0) |
| Hypertension | 34 (26.9) |
| ASA | |
| 1 | 19 (15) |
| 2 | 80 (63.5) |
| 3 | 27 (21.4) |
| Positive urine culture | 35 (27.8) |
| Laterality | |
| Right | 52 (41.2) |
| Left | 74 (58.8) |
| CROES by stone-free percentage | |
| I 80 to 110 pts | 16 (12.7) |
| II 111 to 170 pts | 34 (27) |
| III >170 pts | 76 (60.3) |
ASA: American Society of Anesthesiologists; SD: standard deviation; DM: diabetes mellitus; CRF: chronic renal failure; BMI: body mass index; pts: points.
Results based on groups proposed by CROES.
| Grades | <111 pts | ≥111 pts | p |
|---|---|---|---|
| (%) [min-max] | (%) [min-max] | ||
| Patients/n | 16 (12.7) | 110 (87.3) | |
| EBL/mlc | 50 [5–600] | 50 [5–800] | 0.60a |
| ST/minc | 90 [60–240] | 82 [25–225] | 0.51a |
| DHS/daysc | 4 [3–22] | 4 [2–12] | 0.40a |
| SFR/n | 2 (12.5) | 78 (70.9) | 0.000b |
| Complications | |||
| Clavien ≤2 | 8 (50) | 34 (30.9) | 0.2b |
| Clavien >2 | 2 (12.5) | 13 (11.8) | |
DHS: days of hospital stay; EBL: estimated blood loss; SFR: stone-free rate; ST: surgery time.
Results based on our proposed groups.
| Grades | I | II | III | p |
|---|---|---|---|---|
| (%) [min-max] | (%) [min-max] | (%) [min-max] | ||
| Patients/n | 16 (12.7) | 34 (27) | 76 (60.3) | |
| EBL/mlc | 50 [5–600] | 50 [5–800] | 50 [5–600] | 0.85a |
| ST/minc | 90 [60–240] | 94 [45–225] | 77 [25–180] | 0.01a |
| DHS/daysc | 4 [3–22] | 4 [3–11] | 4 [2–22] | 0.45a |
| SFR/n | 2 (12.5) | 17 (50) | 61 (80) | 0.000b |
| Complications | ||||
| Clavien ≤2 | 8 (50) | 13 (38) | 21 (27) | 0.33b |
| Clavien >2 | 2 (12.5) | 4 (11) | 9 (11) | |
DHS: days of hospital stay; EBL: estimated blood loss; SFR: stone-free rate; ST: surgery time.
PNL is currently the standard of care for stones larger than 2cm. It is very important to have tools that enable us to predict response to treatment to inform our patients more objectively and to plan secondary treatment more appropriately. Thus, we can avoid overreaching ourselves by trying to extract every stone from a patient with complex stones and exposing them to more complications, without necessarily improving the SFR.
For this reason several scales have been developed to predict response to treatment. The first was the Guy's stone score, proposed by Thomas et al., in 2011,4 who developed a 4 grade score according to the anatomical characteristics of the kidney stones and calices. This is a graphic scale where the operator assigns grades according to images. These report an overall SFR of 62%, and according to grades: I (81%), II (72.4%), III (35%) and IV (29%). It is accepted as a reproducible and standardized method that enables rapid and easy assessment to predict the complexity of the PNL.4,5
Subsequently Okhunov et al. proposed a scale called S.T.O.N.E., which gave a more objective evaluation based on computed tomography of the characteristics of the renal cavities and the stones. It takes 5 variables into account, abbreviated with the acronym S.T.O.N.E, Stone size, Tract length, meaning the distance between the skin and the stone, degree of Obstruction, Number of involved calices, and stone Essence, the density of the stones. Assessed in Hounsfield units, a score from 3 to 12 is given according to the characteristics, and divided into 3 groups of complexity, with an SFR as follows: low complexity (4–6) from 94% to 100%, moderate complexity (6–8) from 83% to 92% and high complexity (9–12) from 27% to 64%. The results of this study show an 83.1% precision rate to predict SFR with this scale.6
The CROES, in 2013, proposed the nephrolithometric nomogram, which is different from the previous scales since it includes 2 variables that the others do not consider: the experience of the centre and previous surgery.7 Although this scale has high diagnostic accuracy, the authors suggest dividing the population into 2 groups alone, with a cut-off point of a 60% SFR. This cut-off point does not seem very efficient, since it is very close to the 50% random, and it has been observed that stratification into 3 risk groups is more helpful when applied clinically. Another reason is that other SFR prediction scales also have a tripartite stratification, which in the future might help to make comparisons between them. When we divided the CROES nomogram scale in to 3 groups, we observed that it has high prediction for simple, intermediate and complex cases and that it improves discrimination. In line with this, the recommendation to use only one cut-off point to establish 2 groups is insufficient for clinicians. It is important to mention that, both in the CROES and in this study, a plain abdominal x-ray was used rather than a more sensitive and specific study such as computed axial tomography, which might reduce the SFR, and therefore, modify the predictive level.
Tulga et al., using the CROES nomogram, found results in their series similar to ours for the group with the best prognosis, with a cut-off threshold of 80.5% of SFR, 71% sensitivity and 74% specificity.10
Labadie et al., in a retrospective study, reviewed the clinical records of patients who underwent PNL between 2009 and 2012 in a total of 3 academic institutions. The scores were calculated with the Guy's, S.T.O.N.E. and CROES scales and they evaluated the SFR on computed tomography images. They concluded that the 3 scales had similar sensitivity.8
Bozkurt et al. performed a retrospective study that included 437 patients, from 2012 to 2015, in which they compared the Guy's and CROES scales in predicting SFR, and found similar results with both systems, in addition to similar results in predicting blood loss and surgery time.11
Our study has the limitation of being a historical cohort and using plain abdominal x-ray as a method to establish SFR in the majority of cases. Subsequent external validation is required to establish whether the proposed modification is reproducible in other centres.
ConclusionsThe original assessment with the CROES nomogram demonstrated SFR prediction for complex and simple stones. However, it could not differentiate patients with intermediate scores. Our proposal to stratify into 3 groups within the CROES nomogram enables better differentiation of the intermediate group from the high and low SFR group; however, more studies are required to corroborate the data obtained to date.
Evaluation using the nephrolithometric nomogram demonstrated accurate stone-free rate prediction for complex and simple stones, with a lack of discrimination for patients with intermediate scores. Our modification enabled better differentiation of the intermediate groups from the high and low stone-free rate groups.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Landa-Salas JD, Torres-Anguiano JR, Maldonado-Alcaraz E, Lopez-Samano VA, Serrano-Brambila EA, Moreno-Palacios J. Evaluación de la tasa libre de litos posterior a la nefrolitotomía percutánea mediante el nomograma nefrolitométrico. Cir Cir. 2017;85:510–514.