The development and application of 3D images in laparoscopic surgery has brought the benefit of in-depth perception that traditional laparoscopic surgery lacked. Previous studies in surgical populations have demonstrated the advantages of 3D technology. To limit bias of the previous experiences of participants, this study was performed in a population without any experience in this area.
Material and methodsAn experimental, open, cross-sectional, comparative study between surgical skills achievements using 2D and a 3D laparoscopy equipment, using each subject as their own control. Six skills were evaluated in 2D and 3D modalities.
ResultsOf the 40 participants included, 20 began the skills in the 2D modality and then performed them in 3D, and the other 20 began in 3D. Of the 118 skills evaluated there was a time improvement in 72% in the 3D group compared to 37% in the 2D modality. The accomplishment percentage using the 3D laparoscopy was greater for both groups. There was a statistically significant difference in the better time for the 3D performed tasks. Just over half (52.5%) of participants preferred 3D laparoscopy, 15% preferred 2D, and 32.5% had no preferences.
DiscussionAs other studies have demonstrated, there was improvement in the overall performance using the 3D laparoscope. Bias was limited by using a population without surgical experience.
Conclusions3D laparoscopic surgical skills showed superior to 2D, with higher percentages of tasks completion, less time in performing them, and a shorter learning curve.
El desarrollo y aplicación de imágenes tridimensionales en cirugía laparoscópica ha brindado los beneficios de la percepción de profundidad, de la que la laparoscopia tradicional carecía. Existen estudios al respecto en poblaciones con experiencia quirúrgica previa y para limitar este sesgo de selección realizamos este estudio en población sin experiencia previa.
Material y métodosEstudio experimental, abierto, transversal y comparativo en el que se evaluaron los logros obtenidos con un equipo 2D de cirugía laparoscópica y un equipo 3D, siendo cada sujeto su propio control. Se evaluaron 6 destrezas realizadas en 2D y 3D.
ResultadosSe incluyó a un total de 40 participantes, de los cuales 20 comenzaron los ejercicios en 2D y 20 en 3D. En el 72%, de 118 destrezas se mejoró el tiempo de realización con 3D, contra solo 37% en 2D. El porcentaje al final de los ejercicios en el grupo de 3D tanto en el primero como en el segundo ejercicio fue mayor de manera estadísticamente significativa y se observaron menores tiempos al realizar los ejercicios en 3D. Un 52.5% de los participantes prefirieron el equipo 3D, el 15% el 2D y el 32.5% no tuvieron preferencia por ninguno.
DiscusiónComo se ha encontrado en diversos estudios, existió mejoría en el desempeño en el grupo 3D. Al ser población sin experiencia quirúrgica previa, se elimina este sesgo del estudio.
ConclusionesLa realización de destrezas laparoscópicas en 3D mostró ventajas en comparación con 2D, con mayor porcentaje de finalización, menores tiempos para realizarlas y menor curva de aprendizaje.
The development of minimally-invasive surgical techniques with the known need to acquire new and different manual and psychomotor skills,1,2 has created a need for awareness of the best and most effective ways to learn these skills, in order to evaluate subsequent advances in the design of equipment, and which constitute an effective advantage in performing the techniques which facilitate procedures.3,4
The introduction of video cameras, and monitors with 3D imaging is a clear example of these advances and one which needs to be evaluated.
From an a priori perspective, a third dimension should offer advantages, in particular in the steps or stages of procedures where a view at different levels of depth is essential, in making intra-corporeal knots for example. To date, there have been few studies which assess this variant, in the different types of video cameras, and yet they have been indicated to be of some help.4,5 From our point of view, these studies present a methodological problem which lies in the heterogeneity of the populations studied, as practically all published studies have been undertaken with surgical interns5–7 or with surgeons who have already graduated.
It is known that every year new students have knowledge and skills that have already been learned by new-intake interns, and that these vary considerably according to geographic and academic background, pre-graduation rotation site and, in particular, if there is an association with a family member specialising in laparoscopic surgery. Thus, an evaluation of the basic aspects of 3D equipment on psychomotor skills can be significantly biased. However, because the fundamental principal of evaluation of the supposed advantages of 3D images was chiefly from a psychomotor perspective, and we were not at all interested in evaluating or measuring the level of theoretical medical knowledge (anatomy and aspects of surgical techniques), we preferred to carry out our first evaluation on a population assumed a priori to be more removed from any contact with this type of technique and equipment.
Material and methodsAn experimental, open, cross-sectional, comparative study which evaluated the achievements gained using 2D and 3D laparoscopy equipment. The study was completed in the Hospital General Dr. Manuel Gea González, in Mexico City from 1 February to 1 March of 2014.
The inclusion criteria were students aged over 16, currently undertaking work experience in the central hospital, and with no previous contact with laparoscopic surgery, simulators or equipment. Preparatory level students, nutrition degree students, and psychology degree students, undergraduate medical students, before starting their hospital internships, undergraduate veterinary students, and information technology intern students were included in the study.
Subjects who had had direct contact with laparoscopic surgery techniques and equipment, subjects reporting incapacitating visual impairment, subjects who had not agreed to participate in the study, and subjects who had not completed their skills were excluded from the study.
The sample size was calculated expecting a 45% difference between the percentages of improvement in the time taken to do the exercises (30 with 2D vs. 75% with 3D), with a power of 80% and an alpha level of 0.05, data from at least 38 subjects was required (19 in the 2D group and 19 in the 3D group).
All the subjects were shown a video in which an expert laparoscopic surgeon had been filmed performing each of the skills. They also filled in a questionnaire requesting information on demographic data, their use of lenses, whether they had family members in the surgical profession, whether they had seen these types of procedures before, and the amount of hours spent playing video games each week.
Immediately afterwards a random distribution was made by random computer-generated numbers (Epidat software version 4.0) in order to determine the type of equipment each subject should be started with, recording the time of each procedure.
A cross-over design was used to evaluate the equipment with 2D vision vs. equipment with 3D vision, in which the 2D group initially performed a series of exercises with 2D equipment and then a second series of exercises with 3D equipment; while the sequence was reversed in the 3D group.
In order to assess the initial learning curve, the results obtained from the first attempt at each psychomotor skill were compared with the second attempt (learning), irrespective of the type of laparoscopic surgery used, each subject being their own control. At the end they were asked to state the equipment that they felt most comfortable with.
Description of skillsThe model used was a simulator used for laparoscopic surgery training, characterised by a wooden box, length 40cm, width 30cm, and height 30cm. The upper surface could be disassembled and had 3 15mm holes, with 12cm between them, distributed in a triangle. A laparoscopic lens entered the simulator and 2 Storz® intestinal clamps, 5mm in diameter by 20cm in length, through the 3 holes. A 2D laparoscopic lens was used and a Storz® light source, and a 3D laparoscopic lens and a Viking® light source was used for the skills in 2 and 3 dimensions, respectively.
The skills evaluated were:
- 1.
Pom-poms. This consisted of placing a set of 30 felt pom-poms, 1.5cm in diameter, in 3 different colours, into their respective 3 containers, 6cm in diameter and 3cm high (Fig. 1).
- 2.
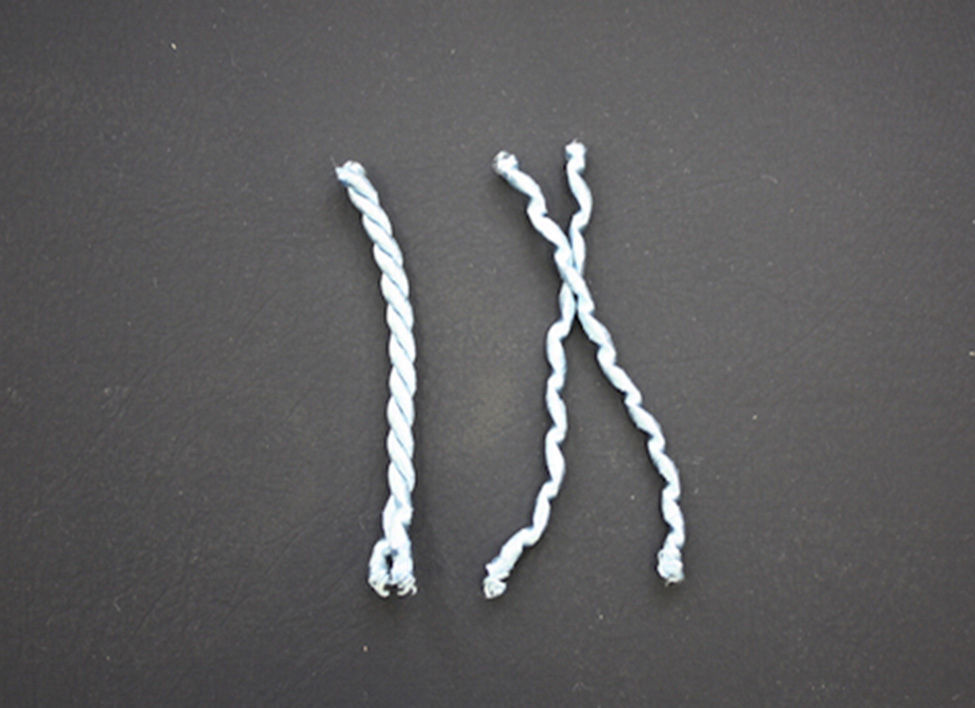
Braids. A double braided strip had to be undone, with a length of 10cm, and a thickness of 0.5cm (Fig. 2).
- 3.
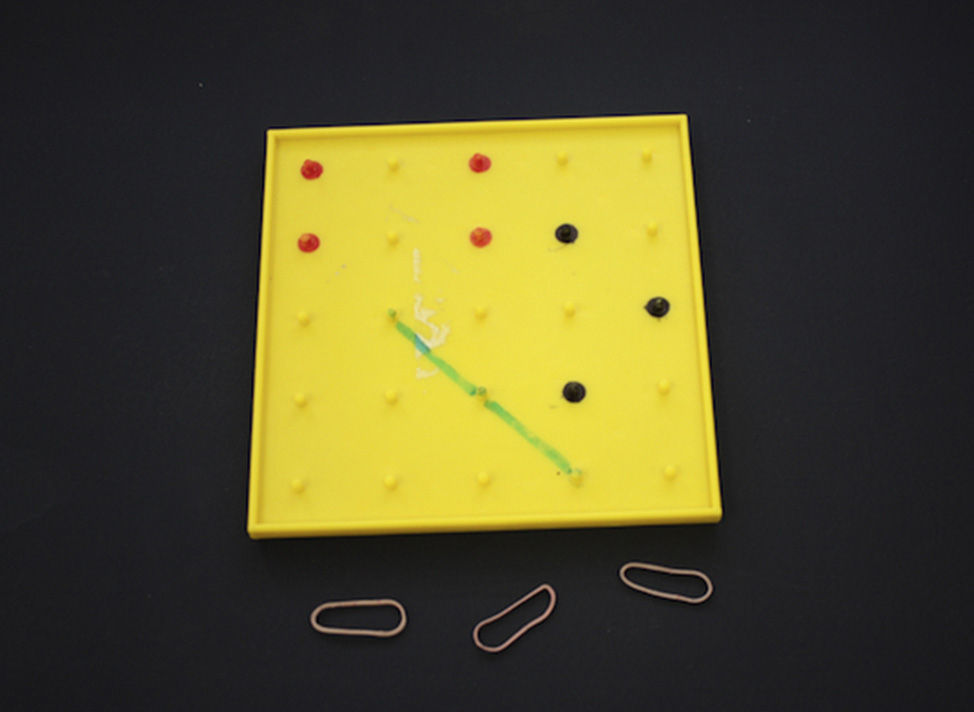
Elastic bands. A square plastic platform of 100cm2, and 25 plastic spurs, 3mm thick, 0.5cm high of the same material emerging onto its surface; the subjects were instructed to put 3 elastic with a resting length of 3cm onto said spurs, to form 3 figures of an equilateral triangle with sides of 5cm, a 3.5cm×7cm rectangle and a straight line 9.5cm long (Fig. 3).
- 4.
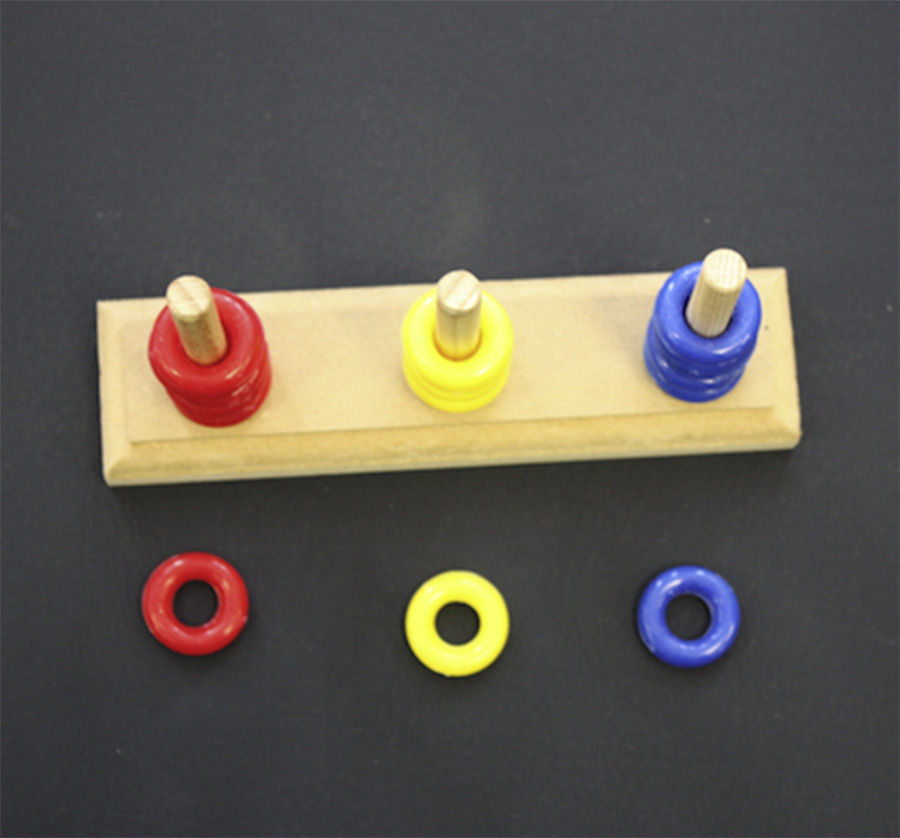
Rings. This activity requires placing 18 plastic rings in a series of 3 colours, 0.5cm thick, and 1cm in diameter, over 3 respective wooden columns (Fig. 4).
- 5.
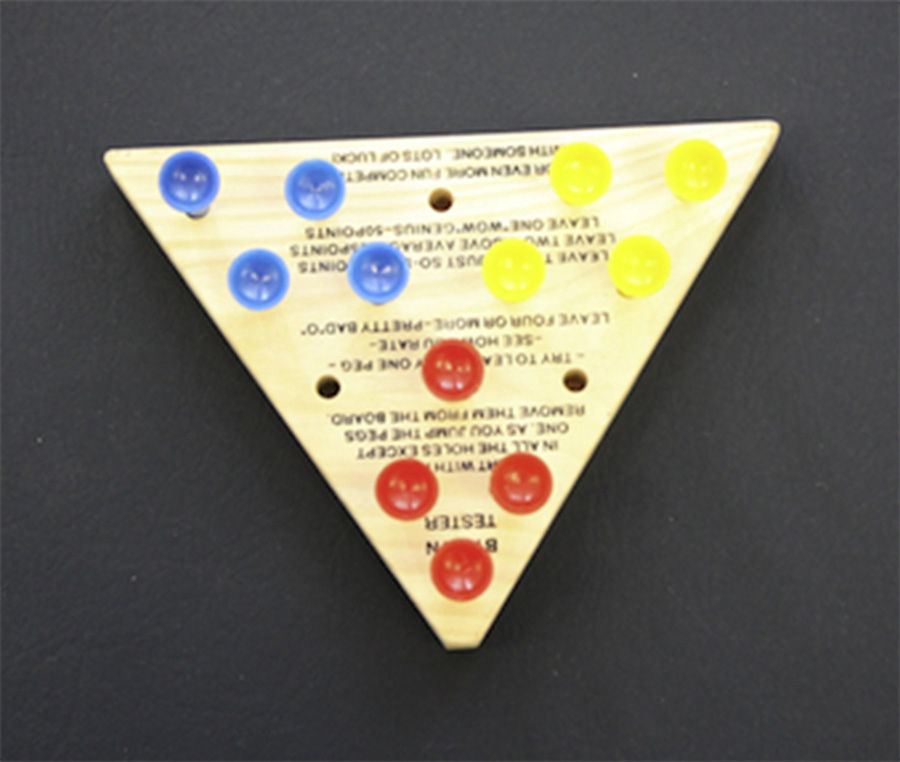
Pegs. On a wooden platform in the form of an isosceles triangle (with a 12.5cm base and sides of 11.5cm), holes of 0.4cm in diameter have been placed into which slot a set of 12 plastic pegs in 3 different colours, 1.3cm long, and crowned with a circular head 1cm in diameter. The skill consists of rotating the positions of the different coloured bars 180° clockwise; this involves picking each of the pegs up, taking them out of their original hole, and putting them into their final location in another hole (Fig. 5).
- 6.
Needle. A straight plastic needle (7.5cm in length and with an eye of 1cm×0.1cm), needs to be threaded with a 7.5cm long plastic thread and then passed with the thread through 3 round plastic buttons 3.5cm in diameter (Fig. 6).
The time taken by a recently graduated surgeon to perform these skills was used to measure the initial time, and duplicated as the maximum permitted for each skill.
Statistical analysisA chi-squared test was used for the following analyses: 1. Differences in the success rate (number of completed procedures compared to uncompleted procedures), in attempts using the 2D and the 3D equipment. 2. Differences in achievement between the first and second attempt at each skill, irrespective of the equipment used (2D vs. 3D).
A Student's t-test was used for the analysis of the quantitative time differences in attempts using the 2D and the 3D equipment, only analysing the subjects who completed them. All the statistical analyses were conducted using IBM SPPS Statistics software version 21.
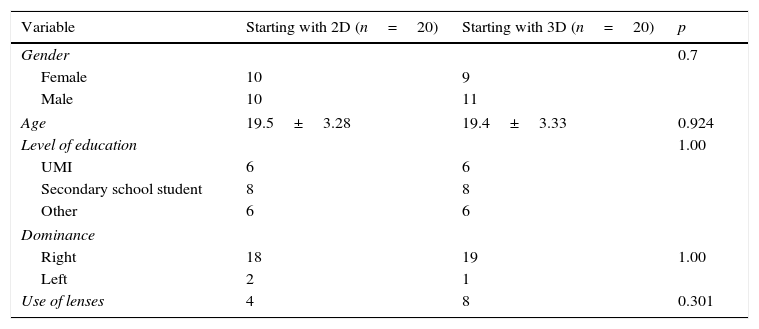
ResultsA total of 40 participants were included, of whom 20 started the first series of 6 skills in 2D and 20 in 3D, at the end of which the equipment was crossed over to perform a second series of exercises. The groups were comparable in distribution by age, gender, level of education, and dominant laterality (Table 1).
General characteristics.
| Variable | Starting with 2D (n=20) | Starting with 3D (n=20) | p |
|---|---|---|---|
| Gender | 0.7 | ||
| Female | 10 | 9 | |
| Male | 10 | 11 | |
| Age | 19.5±3.28 | 19.4±3.33 | 0.924 |
| Level of education | 1.00 | ||
| UMI | 6 | 6 | |
| Secondary school student | 8 | 8 | |
| Other | 6 | 6 | |
| Dominance | |||
| Right | 18 | 19 | 1.00 |
| Left | 2 | 1 | |
| Use of lenses | 4 | 8 | 0.301 |
UMI: undergraduate medical intern.
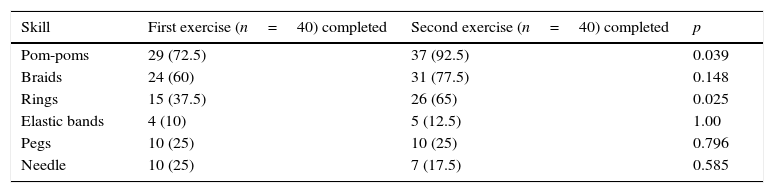
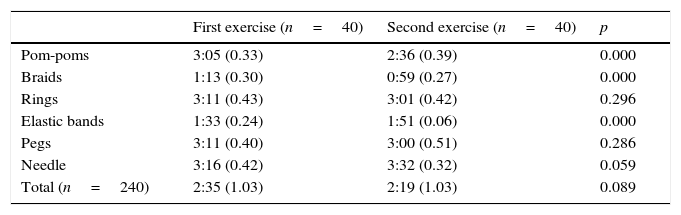
When the different skills were compared it was observed that the students had a greater success rate with the pom-poms followed by the braids, the elastic bands were the most difficult, and the rings, pegs and needles were of intermediate difficulty (Table 2). In general, there was an improvement over the success rate for the skills of the second exercise, which was only statistically significant with the pom-poms and the rings. In 2 exercises no improvement was observed in success rate; there was even a non-significant decrease in the success rate of the needle skill (Table 2). There were also improved times in the second exercise compared to the first (Table 3).
Comparison of success between skills.
| Skill | First exercise (n=40) completed | Second exercise (n=40) completed | p |
|---|---|---|---|
| Pom-poms | 29 (72.5) | 37 (92.5) | 0.039 |
| Braids | 24 (60) | 31 (77.5) | 0.148 |
| Rings | 15 (37.5) | 26 (65) | 0.025 |
| Elastic bands | 4 (10) | 5 (12.5) | 1.00 |
| Pegs | 10 (25) | 10 (25) | 0.796 |
| Needle | 10 (25) | 7 (17.5) | 0.585 |
N (%).
Comparison of times between exercises.
| First exercise (n=40) | Second exercise (n=40) | p | |
|---|---|---|---|
| Pom-poms | 3:05 (0.33) | 2:36 (0.39) | 0.000 |
| Braids | 1:13 (0.30) | 0:59 (0.27) | 0.000 |
| Rings | 3:11 (0.43) | 3:01 (0.42) | 0.296 |
| Elastic bands | 1:33 (0.24) | 1:51 (0.06) | 0.000 |
| Pegs | 3:11 (0.40) | 3:00 (0.51) | 0.286 |
| Needle | 3:16 (0.42) | 3:32 (0.32) | 0.059 |
| Total (n=240) | 2:35 (1.03) | 2:19 (1.03) | 0.089 |
Time in mins (SD).
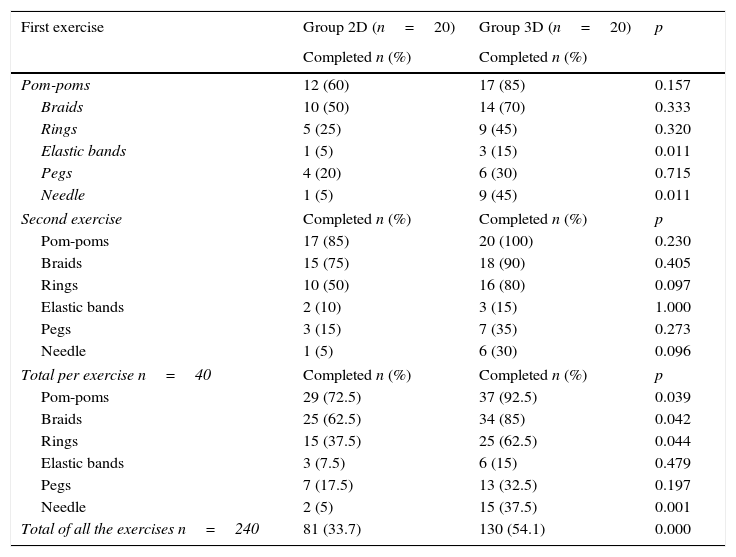
When the exercises performed in 2D were compared to those in 3D, there was a significant improvement in the completion rate of some exercises in the 3D group, in both the first and the second exercise. Furthermore, when comparing the totals, there was a greater completion rate of the 3D exercises in the pom-pom, braid, ring and needle exercises which was statistically significant (Table 4). Finally, when evaluating the total exercises, a greater completion rate was observed of the 3D exercises; this was statistically significant (Table 4).
Comparison of success between groups.
| First exercise | Group 2D (n=20) | Group 3D (n=20) | p |
|---|---|---|---|
| Completed n (%) | Completed n (%) | ||
| Pom-poms | 12 (60) | 17 (85) | 0.157 |
| Braids | 10 (50) | 14 (70) | 0.333 |
| Rings | 5 (25) | 9 (45) | 0.320 |
| Elastic bands | 1 (5) | 3 (15) | 0.011 |
| Pegs | 4 (20) | 6 (30) | 0.715 |
| Needle | 1 (5) | 9 (45) | 0.011 |
| Second exercise | Completed n (%) | Completed n (%) | p |
| Pom-poms | 17 (85) | 20 (100) | 0.230 |
| Braids | 15 (75) | 18 (90) | 0.405 |
| Rings | 10 (50) | 16 (80) | 0.097 |
| Elastic bands | 2 (10) | 3 (15) | 1.000 |
| Pegs | 3 (15) | 7 (35) | 0.273 |
| Needle | 1 (5) | 6 (30) | 0.096 |
| Total per exercise n=40 | Completed n (%) | Completed n (%) | p |
| Pom-poms | 29 (72.5) | 37 (92.5) | 0.039 |
| Braids | 25 (62.5) | 34 (85) | 0.042 |
| Rings | 15 (37.5) | 25 (62.5) | 0.044 |
| Elastic bands | 3 (7.5) | 6 (15) | 0.479 |
| Pegs | 7 (17.5) | 13 (32.5) | 0.197 |
| Needle | 2 (5) | 15 (37.5) | 0.001 |
| Total of all the exercises n=240 | 81 (33.7) | 130 (54.1) | 0.000 |
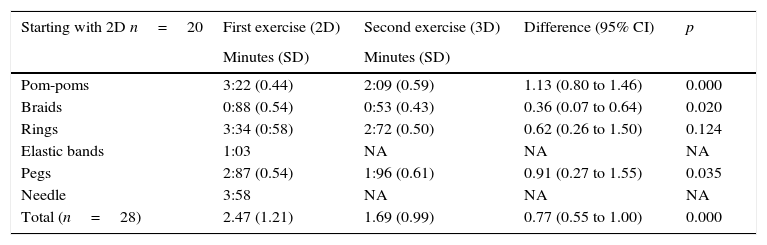
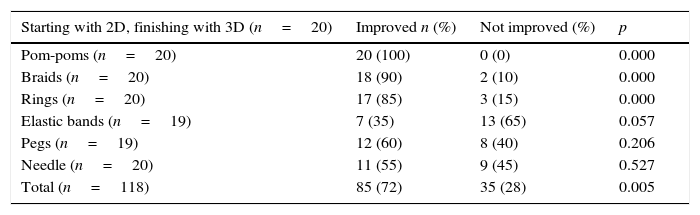
Table 5 shows the comparisons in times between the group which started in 2D and the group that started in 3D where a statistically significant difference can be observed with lower times taken to perform the 3D exercises, compared to the group which started in 2D, and this improvement was not observed in the second exercise when the first exercise had been performed in 3D; the improved performance is also illustrated in Table 6. Finally, with regard to the preferences questionnaire, 52.5% of the participants preferred the 3D equipment, 15% the 2D equipment, and 32.5% had no preference for either.
Before and after comparison of groups 2D vs. 3D.
| Starting with 2D n=20 | First exercise (2D) | Second exercise (3D) | Difference (95% CI) | p |
|---|---|---|---|---|
| Minutes (SD) | Minutes (SD) | |||
| Pom-poms | 3:22 (0.44) | 2:09 (0.59) | 1.13 (0.80 to 1.46) | 0.000 |
| Braids | 0:88 (0.54) | 0:53 (0.43) | 0.36 (0.07 to 0.64) | 0.020 |
| Rings | 3:34 (0:58) | 2:72 (0.50) | 0.62 (0.26 to 1.50) | 0.124 |
| Elastic bands | 1:03 | NA | NA | NA |
| Pegs | 2:87 (0.54) | 1:96 (0.61) | 0.91 (0.27 to 1.55) | 0.035 |
| Needle | 3:58 | NA | NA | NA |
| Total (n=28) | 2.47 (1.21) | 1.69 (0.99) | 0.77 (0.55 to 1.00) | 0.000 |
| Starting with 3D n=20 | First exercise (3D) | Second exercise (2D) | Difference (IC 95%) | p |
|---|---|---|---|---|
| Minutes (SD) | Minutes (SD) | |||
| Pom-poms | 2.79 (0.55) | 2.73 (0.60) | 0.05 (−0.34 to 0.45) | 0.775 |
| Braids | 0.96 (0.46) | 0.97 (0.43) | −0.01 (−0.45 to 0.44) | 0.979 |
| Rings | 2.77 (0.83) | 3.03 (0.64) | −0.26 (−0.84 to 0.32) | 0.326 |
| Elastic bands | 1:25 | 1:50 | NA | NA |
| Pegs | 2.80 (1.21) | 3.10 (1.01) | −0.30 (−4.54 to 3.94) | 0.790 |
| Needle | 4:00 | 3:00 | NA | NA |
| Total (n=41) | 2.29 (1.06) | 2.33 (1.04) | −0.04 (−0.29 to 0.21) | 0.738 |
Comparison of the performance of groups 2D vs. 3D.
| Starting with 2D, finishing with 3D (n=20) | Improved n (%) | Not improved (%) | p |
|---|---|---|---|
| Pom-poms (n=20) | 20 (100) | 0 (0) | 0.000 |
| Braids (n=20) | 18 (90) | 2 (10) | 0.000 |
| Rings (n=20) | 17 (85) | 3 (15) | 0.000 |
| Elastic bands (n=19) | 7 (35) | 13 (65) | 0.057 |
| Pegs (n=19) | 12 (60) | 8 (40) | 0.206 |
| Needle (n=20) | 11 (55) | 9 (45) | 0.527 |
| Total (n=118) | 85 (72) | 35 (28) | 0.005 |
| Starting with 3D, finishing with 2D (n=20) | p value | ||
|---|---|---|---|
| Pom-poms (n=20) | 9 (45) | 11 (55) | 0.527 |
| Braids (18) | 9 (45) | 11 (55) | 0.527 |
| Rings (20) | 6 (30) | 14 (70) | 0.011 |
| Elastic bands (20) | 7 (35) | 13 (65) | 0.057 |
| Pegs (20) | 3 (15) | 17 (85) | 0.000 |
| Needle (19) | 3 (15) | 17 (85) | 0.000 |
| Total (n=117) | 37 (30.9) | 83 (69.1) | 0.016 |
The main limitation of laparoscopic surgery is 2D vision, compared to the three-dimensionality of open surgery. This has resulted in the development of new imaging technologies such as 3D laparoscopy, and the daVinci robot system.8 One of the main advantages of the three-dimensional system is that it shortens the learning curve for surgeons who are not very experienced, as it enables them to become familiar with an environment very different to that of open surgery.9,10 It has also been demonstrated that this platform improves the perception of the shape of figures, and therefore it improves the anatomical appreciation of students with few visuospatial skills with advances in optical feedback.11
Comparative studies have been undertaken in which it has been shown that three-dimensional laparoscopic vision improves performance times in complex exercises, and of novice surgeons, during the acquisition of minimally-invasive surgery skills.12,13 However, although this demonstrates some advantages of this technology, the results are also determined by the level of experience of each trainee surgeon, and by any surgical skills they may have gained previously; and therefore to eliminate these factors in determining the benefits of performing 3D laparoscopic skills, the population of this study had no previous surgical experience at all. The trend in all the studies was towards an improvement after performing the procedures in 3D.
It was evident, with statistically significant differences, that the participants improved the second time they carried out the exercise, both in the completion rate of the task and in the times taken, especially if they had undertaken the task in 2D first and the second time in 3D. The improvement was more marked with the 3D equipment in the more complex tasks, compared to the simpler tasks. This coincides with Alaraimi's5 randomised study with similar results, and with more obvious improvement in complex tasks.
Some authors have published adverse effects such as eye strain and dizziness while using 3D laparoscopy.9,10 In our study's population none of the participants presented collateral effects with the use of lenses for 3D imaging; however, a small percentage (15%) preferred 2D vision to 3D vision.
Furthermore, there are authors who have evaluated the superiority of 3D laparoscopy not only in terms of performance and time, but also in the amount of errors committed, which might have an impact on patient safety.14,15 Although in this study the amount of errors made was not established, the fact that improvements were achieved with regard to the percentages completing the 3D tasks compared to the 2D tasks and the improved times reflect greater accuracy in undertaking the tasks.
In this study any of the tasks undertaken reflected the learning curve from zero, as the population had never been exposed to similar tasks. This enabled us to demonstrate that the learning curve is shorter with 3D imaging, and this is reflected in better times and completion rates in the first phase of the exercises performed by those initially allocated to 3D. In addition, those participants performed well subsequently on the 2D model. The participants starting with 2D showed significant improvement when they performed the second task in 3D. Storz et al.12 have also demonstrated an improved learning curve in medical students and expert surgeons in tasks performed in 3D. Other authors, like Cicione et al.,16 have demonstrated an improved learning curve using 3D imaging on a urology model.
ConclusionsPerforming 3D laparoscopic skills showed advantages compared to 2D with a greater completion rate, shorter completion times, and a shorter learning curve. Because the study population had had no previous contact with surgical procedures, we can conclude that 3D imaging has these benefits, irrespective of the experience and skill of the surgeon.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Romero-Loera S, Cárdenas-Lailson LE, de la Concha-Bermejillo F, Crisanto-Campos BA, Valenzuela-Salazar C, Moreno-Portillo M. Comparación de destrezas en simulador de laparoscopia: imagen en 2D vs. 3D. Cirugía y Cirujanos. 2016;84:37–44.