The introduction of laparoscopic surgery (LS) can be considered the most important advancement in our specialty in the past 25 years. Despite its advantages, implementation and consolidation have not been homogenous, especially for advanced techniques. The aim of this study was to analyse the level of development and use of laparoscopic surgery in Spain at the present time and its evolution in recent years.
Material and methodsDuring the second half of 2012 a survey was developed to evaluate different aspects of the implementation and development of LS in our country. The survey was performed using an electronic questionnaire.
ResultsThe global response rate was 16% and 103 heads of Department answered the survey. A total of 92% worked in the public system. A total of 99% perform basic laparoscopic surgery and 85,2% advanced LS. Most of the responders (79%) consider that the instruments they have available for LS are adequate and 71% consider that LS is in the right stage of development in their environment.
ConclusionsBasic laparoscopic surgery has developed in our country and is considered to be the standard surgery performed by most surgeons, and forms part of the basic surgical training of residents. With regard to advanced LS, although it is frequently used, there are still remaining areas of deficit, and therefore, opportunities for improvement.
La introducción de la cirugía laparoscópica (CL) puede considerarse el avance más importante que ha experimentado nuestra especialidad en los últimos 25 años. A pesar de sus ventajas, la implantación y consolidación de la CL no ha sido homogénea, especialmente si tenemos en cuenta las técnicas laparoscópicas avanzadas. El objetivo de este trabajo es analizar el nivel de desarrollo e implantación de la CL en España en el momento actual y analizar su evolución en los últimos años.
Material y métodosDurante el segundo semestre de 2012 se desarrolló una encuesta que evaluaba distintos aspectos relacionados con la implantación y el desarrollo de la CL en nuestro país. La encuesta se realizó mediante un cuestionario electrónico.
ResultadosLa tasa global de respuesta a la encuesta fue del 16% y 103 jefes de Servicio contestaron el cuestionario. El 92% correspondió a cirujanos de centros sanitarios públicos. El 99% de los encuestados realizaba CL básica y el 85,2%, avanzada. La mayor parte de los encuestados (79%) considera que el instrumental y los equipos para CL de los que dispone son correctos y el 71% considera que, en su medio, la CL está en el lugar adecuado.
ConclusionesLa CL básica ha logrado desarrollarse en nuestro país hasta considerarse un estándar practicado por la mayoría de los cirujanos y ser parte de la formación básica del residente de cirugía. Con respecto a la CL avanzada, aunque los porcentajes de utilización son altos, todavía existen déficits y, en consecuencia, oportunidades de mejora.
The introduction of laparoscopic surgery (LS) can be considered as the most important advancement in our specialty in the past 25 years. During this period the results of numerous laparoscopic techniques have surpassed those of the traditional approach, demonstrating advantages that have been found to be clinically significant, improved quality of life and patient management. However, there has been no standardised introduction and consolidation of LS, particularly regarding advanced laparoscopic techniques. Procedures such as cholecystectomy,1,2 hiatus hernia and anti-reflux surgery3 and even other more complex surgical interventions such as bariatric surgery4 have obtained very high replacement rates to LS. By contrast, other procedures such as surgery of the colon have not obtained their expected LS levels given their high prevalence.5
In 2003, the Endoscopic Section of the Spanish Association of Surgeons (AEC in Spanish) conducted a survey among Spanish surgeons, the objective of which was to hear their opinion on LS and become aware of the level of implementation of these techniques in Spain.6 This survey reported that although LS was widely accepted for the treatment of cholelitiasis and gastroesophageal reflux disease (GERD), and that hospitals had the sufficient technical means to perform it, it was still rarely used. The aim of our study was therefore to analyse the evolution of LS from its introduction into Spain 25 years ago, and 10 years after the publication of the abovementioned survey.
The aim of this study was to analyse the level of development and use of laparoscopic surgery in Spain at the present time and its evolution in recent years.
Material and MethodsDuring the second half of 2012 the project for the development of a survey began to evaluate the different aspects relating to the introduction and development of LS in Spain. The survey was conducted using an electronic questionnaire (https://docs.google.com/spreadsheet/viewform?formkey=dE9ob1FmaFJTVlpPbko4OXByc04tLWc6MQ) and published through the AEC's electronic media.
The questionnaire consisted of a total of 64 questions. Of these, 56 referred to general demographic aspects, equipment availability, and the use of the laparoscopic approach in different groups of disease, training and innovations. Three of the questions were directed only at hospitals accredited to train residents and were about aspects of training. Finally, five questions were directed at department heads. With regard to techniques, only generally accepted ones were explored, with the exclusion of minimally invasive surgery of the thyroid glands and cancer of the oesophagus, liver and head of the pancreas. The Feliu et al.6 survey conducted previously was not reproduced completely since it was considered that numerous aspects contained in it lacked contemporary validity.
Completion of the questionnaire was enhanced by the response design which used percentages and descriptive terms (regularly, 50% of the time, 25% of the time, sporadically, never, over 75%, between 50%–75%, between 25% and 50%, less than 25%) rather than quantitative data. Additionally, in order to summarise several results, the non-routine use of the laparoscopic approach (50% of the time, 25% of the time, sporadically) was grouped under the term “occasional”.
Responses to the different questions were expressed as relative frequencies. Quantities variables were presented as mean± (SD). The ratios between the variables of hospital size and resident doctor training variables and the frequencies of different procedures were carried out using the chi square test. For the paired comparisons between the different procedures the McNemar test was used. The statistical significance level considered was 5% (P<.05).
For all calculations the PASW statistics programme version 18.0 (SPSS, Inc., Chicago, IL, USA) was used.
The study did not receive public or private financial support and the final decision to publish these findings was taken by the survey coordinator and the Endoscopic Surgery Section Board of the Spanish Association of Surgeons.
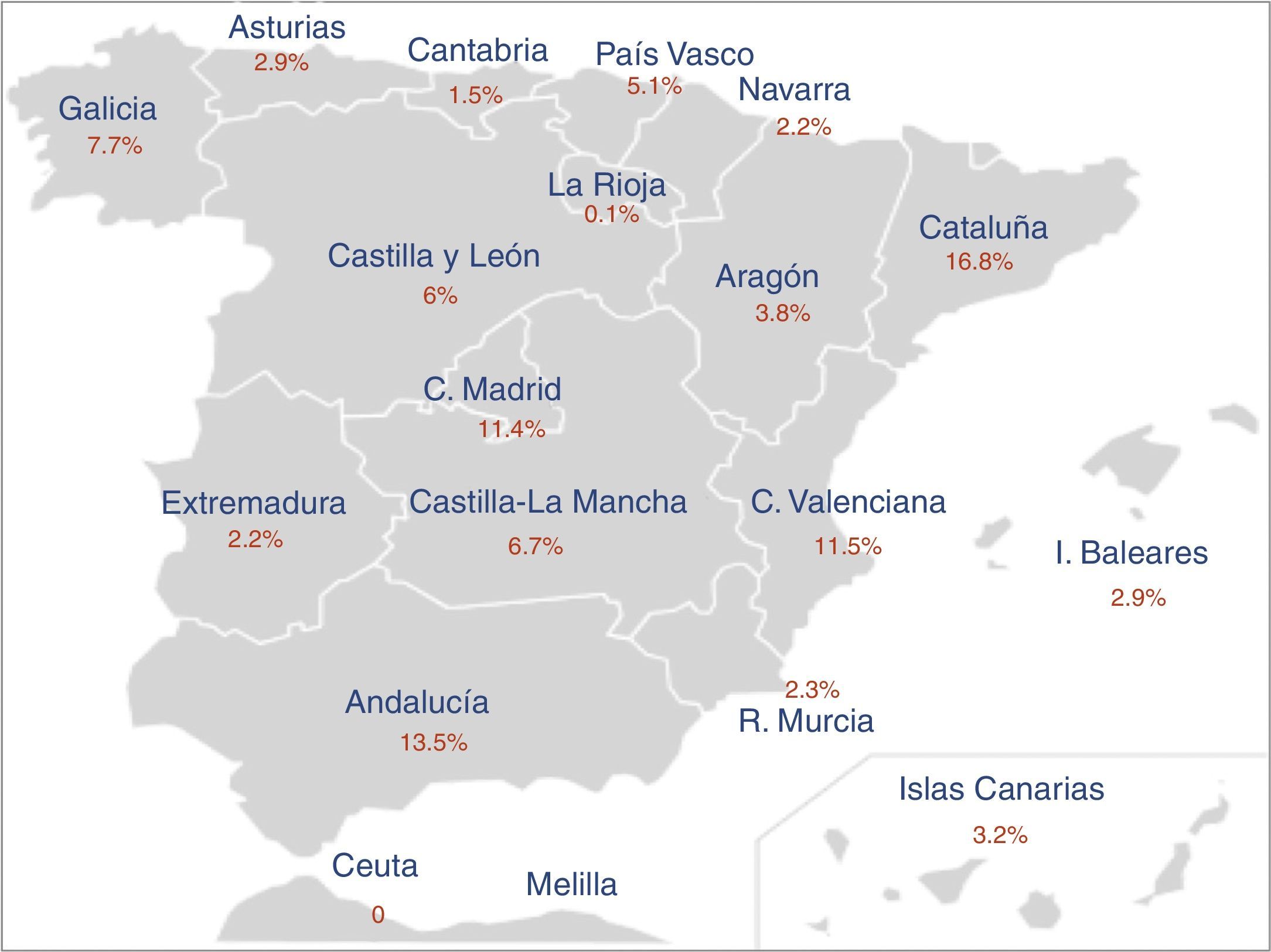
FindingsOf the 4387 active members of the Spanish Association of Surgeons, 684 (16%) responded to the survey. 25% of the members of the Endoscopic Surgery Section completed the questionnaire. The section aimed at department heads was answered by 15% of participants. 74% were received from hospitals that include resident training. Geographic distribution of respondents is shown in Fig. 1.
Regarding hospital size, 9% of the hospitals had less than 100 beds, 17% between 100 and 200, 25% between 200 and 400, 22% between 400 and 600, and 27% were hospitals with over 600 beds.
The mean age of the respondents was 46.5±9.4 (27–73). 92% were surgeons from public hospitals, 26% were unit heads (15%) or department heads (11%).
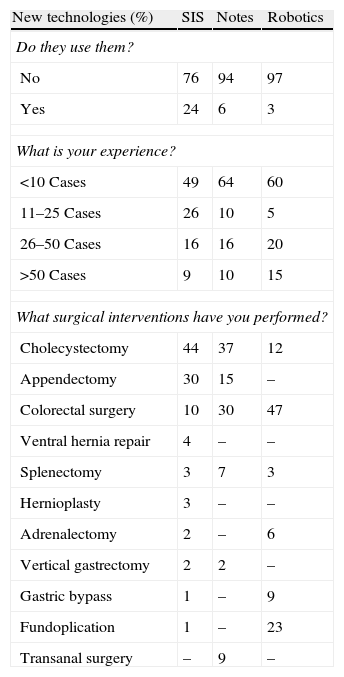
The mean experience of respondents in LS was 13.5±5.9 (1–40). Half had an experience of less than 14 years and 25%, of 19 or more years. 99% of respondents carried out basic laparoscopic surgery and 85.2%, advanced surgery (funduplication, gastrectomy, colectomy, rectal resection, solid organ surgery, bariatric surgery). Reasons for not performing advanced LS are: insufficient cases (46%), training access problems (24%), avoiding the learning curve (24%) or considering that LS offers no advantages over the traditional approach (13%). 69% performed LS in more than 50 operations per year, but only 30% performed over 50 advanced procedures (Table 1).
Most respondents (79%) consider that the instruments and equipment available to them for LS are appropriate and 71% consider that, on average LS is performed in its correct place.
The questionnaire aimed at department heads was completed in 103 cases. According to respondents the number of surgeons using basic laparoscopy exceeds 75% of the staff in the majority of departments (91%). There were no statistically significant differences between the opinion of the department heads and the other surgeons (P=.4). With regard to advanced LS, in 27% of the departments, the majority of surgeons (>75%) carried out some kind of advanced procedure, in 32% this was completed by 50% of the staff and in 41% of cases, the advanced procedures were carried out by less than half of the surgeons. In this case, the opinion of the department heads (99.7% believe that it is carried out with some frequency in their Department) is significantly different (P<.001) to the opinion of the other specialists (81%).
According to the heads of department, the most frequent reason (50%) for not carrying out advanced procedures is an insufficient number of cases from which to gain experience, although training problems impede their development in up to 20% of centres. There is an obvious correlation between the answers from heads of department and the other surgeons. However, reservations with regard to the learning curve are exclusive to staff surgeons.
The majority of department heads surveyed (86%) consider that the LS material they have is correct and that in their department, LS is in its appropriate place. This favourable opinion regarding the development of LS in their unit is significantly higher (P<.001) than the opinion of the other surgeons.
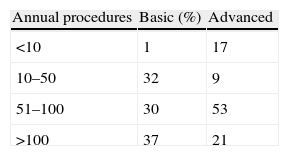
Emergency Laparoscopic SurgeryThe findings regarding the use of LS in emergency departments are summarised in Table 2. 93% of respondents have the possibility of performing emergency LS. If it cannot be carried out, in 50% of the cases the impediments found are due to external factors (anaesthesia, nursing care), in 31% of the cases it is due to lack of experience of the team, in 10% of cases to the lack of access to laparoscopic material during the duty shift and in 9% of the cases LS is not used in their emergency departments.
Emergency Laparoscopic Procedures.
| Laparoscopic procedures (%) | |
| Acute abdomen to determine in woman of reproductive age | |
| Never | 0.1 |
| Sporadically | 7 |
| 25% of cases | 11.9 |
| 50% of cases | 14 |
| Regularly | 67 |
| Acute cholecystitis | |
| Never | 2 |
| Sporadically | 4 |
| 25% of cases | 7 |
| 50% of cases | 8 |
| Regularly | 79 |
| Duodenal perforation | |
| Never | 14 |
| Sporadically | 4 |
| 25% of cases | 13 |
| 50% of cases | 19 |
| Regularly | 50 |
Hospital size was not statistically significant (P=.08), but the tendency to perform emergency LS was proportionate to the centre size. With regard to procedures, performing emergency laparoscopy for the treatment of acute abdomen in women of reproductive age or for the treatment of duodenal perforation correlated with the experience in advanced LS (P<.001), this relationship was not demonstrated in the treatment of acute cholecystitis (P=.21).
Abdominal Wall SurgeryThe most frequently performed surgery by respondents is abdominal wall surgery (96%). However, 64% never use endoscopic surgery for the repair of inguinal hernia, 30% do so occasionally and only 6% regularly use it. In the case of incisional hernia, standard use rose to 10%, whilst 49% used it selectively and 41% never considered it. This was also the trend in the case of non-frequent abdominal wall hernias. Analysis of the correlation between regular or occasional use of the laparoscopic approach in the different types of hernia revealed a statistically significant association (P<.001). This trend was maintained among the respondents who never use this method.
Benign Gastroesophageal Surgery43% of respondents regularly performed this type of surgery and 29% performed it sporadically. Of these, 85% regularly performed LS of GORD. However, in the case of major hiatal hernias and achalasia, preference for the laparoscopic approach is significantly lower (65% and 68% respectively).
GORD treatment using LS did not present any correlation with other variables. However, there was a preference for major hiatus hernias to be treated in large hospitals (P<.001) and achalasia in teaching hospitals (P<.001). A significant correlation also existed (P<.001) in the regular use of LS for the treatment of the three types of disease under consideration.
Gastric SurgeryWith regard to gastric surgery, only 27% of respondents regularly use LS for this type of disease, whilst 48% do so occasionally and 25% never do. 82% regularly (45%) or occasionally (37%) use LS in benign gastric disease, a trend mostly used for the treatment of GIST tumours. However, only 18% of respondents used a laparoscopic approach for gastric cancer as standard and 40% used it selectively. 42% of respondents, however, never use LS for the treatment of gastric cancer.
The use of LS in the treatment of gastric disease correlated with hospital size. This correlation rises with complexity (benign gastric disease P=.02, GIST and malignant disease P<.001). Finally, gastric cancer treatment with LS correlated with standard management of other gastric diseases using this method (P<.001).
Colorectal Cancer90% of the surgeons who participated in the survey regularly (59%) or sporadically (31%) performed colorectal surgery. The laparoscopic approach in benign disease of the colon was used in 89% of the cases (66% as standard and 23% occasionally). In the case of malignant disease, laparoscopy rose to 82% (57% standard and 25% occasionally). However, in the case of rectal neoplasias, only 43% of respondents regularly used LS, with 36% doing so selectively.
There was a correlation throughout the whole colorectal disease group with hospital size, detecting an increase in statistical significance as surgery complexity increased (benign disease of the colon P=.05, malignant disease of the colon P=.001, rectal disease P<.001). Finally, regular use of the laparoscopic approach for the treatment of rectal disease was correlated with the high rate of the use of this approach in the treatment of disease of the colon (P<.001).
Solid Organ SurgeryLS of the adrenal glands is standard among respondents and only 4% replied that they did not use this method. However, up to 26% responded that they did not use laparoscopy for splenic diseases.
In the case of liver surgery, endoscopy was used by 54% of respondents, although only 16% used it on a regular basis. A great majority use LS for the treatment of simple cysts (82%) whilst in benign neoplasias the usage rate drops to 60%, its use was selective in 39% of cases.
LS is frequently used in surgery of the tail of the pancreas (31% regularly and 31% occasionally) among surgeons who perform pancreatic surgery (48% of respondents).
Large hospitals are preferred for the treatment of splenic and adrenal diseases (P<.001).
Bariatric SurgeryIn treating morbid obesity 91% of surgeons regularly use bariatric laparoscopic surgery techniques, whilst 1% always use open surgery.
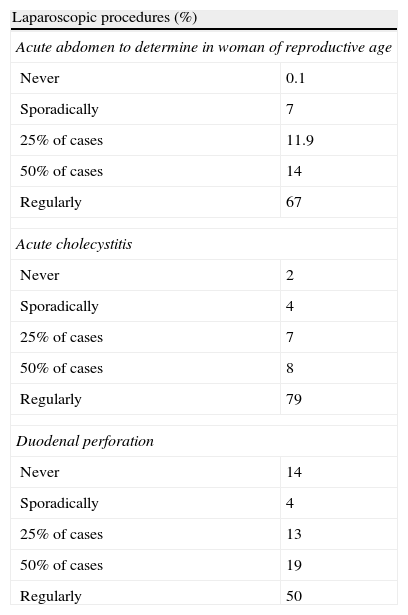
Use of New TechnologiesThe results regarding the use of new technologies are shown in Table 3; the most widely used technology is single incision surgery. In any case, the number of cases does not rise above 50 and most are for cholecystectomies, appendicectomies and resections of the colon. There is no correlation between hospital type or size, and the use of new technologies. However, there is a significant correlation between surgeons who regularly use colorectal LS and those who have some experience in the management of this disease using robots (P=.05) or surgery through natural orifices (P=.002).
Use of new technologies.
| New technologies (%) | SIS | Notes | Robotics |
| Do they use them? | |||
| No | 76 | 94 | 97 |
| Yes | 24 | 6 | 3 |
| What is your experience? | |||
| <10 Cases | 49 | 64 | 60 |
| 11–25 Cases | 26 | 10 | 5 |
| 26–50 Cases | 16 | 16 | 20 |
| >50 Cases | 9 | 10 | 15 |
| What surgical interventions have you performed? | |||
| Cholecystectomy | 44 | 37 | 12 |
| Appendectomy | 30 | 15 | – |
| Colorectal surgery | 10 | 30 | 47 |
| Ventral hernia repair | 4 | – | – |
| Splenectomy | 3 | 7 | 3 |
| Hernioplasty | 3 | – | – |
| Adrenalectomy | 2 | – | 6 |
| Vertical gastrectomy | 2 | 2 | – |
| Gastric bypass | 1 | – | 9 |
| Fundoplication | 1 | – | 23 |
| Transanal surgery | – | 9 | – |
SIS: single incision surgery; Notes: surgery through natural orifices.
Finally the majority (90%) of respondents believe that new technologies in LS are a step forward in endoscopic surgery and would offer benefits.
Training in Laparoscopic Surgery During the Residency Period62% of the units with resident training use laparoscopic training simulators. 25% of respondents believe that a resident doctor should carry out basic LS (appendicectomy and cholecystectomy). There is correlation here with what they actually do. Regarding advanced LS (ventral hernia repair, fundoplications and colectomy), up to 20% of surgeons think that the residents should perform these procedures although these expectations are not fulfilled in their Departments.
DiscussionThe expansion of minimally invasive techniques has led to a large number of surgical interventions being possible with LS. However, the levels of implementation and development are very variable due to different factors which include the type of disease, the technical difficulty of some of these techniques, the specific needs for training and the need to take on a new learning curve.
Ten years after the last survey conducted by the Spanish Association of Surgeons to discover the status of LS in Spain, it was considered that sufficient time had elapsed for its level of implementation to be reassessed and to analyse its development over this period of time.
Surveys directed at wide samples are tools which enable current and true information to be obtained in a short space of time,7,8 and have been used previously to audit the status of endoscopic surgery in different specialties in Spain.6,9,10 Moreover, periodic surveys not only provide updated information on aspects audited, they also enable comparisons to be made.6
The response rate to this survey was low despite being aimed at a well-identified target population and using electronic methods for dissemination. This may be considered a limitation of this study. Our experience has been that low participation in this type of initiative is the norm, and possible causes to justify this fact are low interest in LS and different demographic aspects in relation to AEC members.6 Another factor influencing low participation in this survey is the social, economic and employment reality in Spain, which make us increasingly vulnerable to behavioural changes leading to a lack of interest in all aspects related to the profession.11 Nevertheless, the low rate of response and surveys targeted at the medical profession is a universal and constant fact, with response rates between 11% and 50%12; financial incentives have even been put forward as a strategy to increase the number of responses.13 Finally, to support the validity of our findings, we would point out that the trends found in this type of study are considered more important than the absolute values obtained.12,13
In view of our findings, the level of implementation of basic LS in Spain may be considered universal and its use routine. Maturity gained through laparoscopic techniques, the continuous appearance of studies to support their validity in different areas and the availability of training tools have led to a major increase in the number of surgeons with advanced LS skills (85% vs 25%).6 However, there is still room for improvement. At present, the reasons argued for not carrying out advanced LS are exactly the same as those used years ago6 and are summed up in lack of training and experience. Moreover, for a high number of surgeons (20%) having to embark on a learning curve is sufficient cause for their failing to perform advanced LS, although these reserves were exclusive to the staff surgeons who participated in the survey. Finally, it is surprising that there is still a percentage of surgeons who consider that LS does not offer any advantages over the traditional approach; this percentage continues to be the same as in the survey by Feliu et al.6
With respect to hospital equipment, the majority of respondents (79%) are satisfied with the technical means available. Department heads are most optimistic (86%), and there is a significant increase (70%) compared with years ago.6
Training in LS during the residency period is one of the basic pillars for its consolidation and development. In this regard, the advancement during this decade has been very notable. Years ago, 15% of surgeons thought that advanced LS could be approached during residency but in reality a mere 1% had access to this training.6 At present, over 90% of respondents think that residents should perform basic LS and the opinion about access to advanced LS has greatly improved (72% think they should know how to perform a fundoplication). Current reality does not meet these expectations, but over 80% of resident physicians perform basic LS and between 25% and 45% perform some type of advanced LS. Undoubtedly apart from the knowledge acquired in the departments where the resident physician is trained, the inclusion in the speciality training of a practical initiation course in endoscopic surgery and advanced LS contribute and will lead to the consolidation of even higher standards.14 In this sense, it is important to note the work carried out by the Endoscopic Surgery Section of the AEC which has been coordinating an LS training course since 2010 on a national level and since 2000 has supported the advanced LS course of the General Hospital of Castellón, planting the seed for future advanced LS courses promoted by the Section. Finally, it is worth mentioning that LS simulators are available in a great many departments for the acquisition of basic skills prior to working in surgery15–17; this training should be essential for all resident surgeons.
Emergency LS has become widely performed in Spain. A great number of respondents had the opportunity to perform it and if they did not, this was mainly due to external constraints. Another obstacle was the lack of experience of the team on call and occasionally the department's policy impeded implementation. Regarding procedures, there is frequent use of LS for the management of acute abdomen in women of reproductive age or in duodenal perforation and this correlates with greater experience in advanced LS. This aspect was not confirmed in the case of acute cholecystitis, which translates as generalised use of LS for this indication. It is worthy of note that 80% of respondents regularly use the laparoscopic approach for treatment of acute cholecystitis and up to 18% are selective about it. These figures are found in the range of what was considered optimum in the survey years ago6 and very much above (50%) other studies.1
LS usage analysis by area of specific knowledge demonstrates very different tendencies. In general, performing advanced laparoscopic procedures is linked to hospital size, which is logical since the main reason for not using advanced LS is the small number of cases and this would not apply in larger sized hospitals.
LA use is low in abdominal wall surgery, which is the disease respondents most frequently treated, and there has been little development compared with previous surveys.6 Only 6% routinely used it to repair inguinal hernia and 10% regularly use it to repair ventral hernias and rare hernias. These figures are below usage rates reported in recent publications, both in the case of inguinal (6%–18%) and incisional hernia (26.6%),18,19 which may be related to doubts about the advantage of LS in these procedures, pressure on healthcare for very common diseases and cost.
Treatment of GORD with LS continues to be one of its most accepted indications, from 80% to 85% of respondents6 having increased its use; these figures are very much higher than those registered in traditional studies.3 However, open surgery is still used in numerous cases of major hiatal hernias and in the treatment of achalasia. This fact contrasts with figures published in literature.20,21 The lower prevalence of these diseases, the technical difficulty of treatment and recurrence rates found could account for this trend.
There is a clear tendency to use laparoscopic surgery in the treatment of benign gastric diseases and gastric GIST, but the use of LS in malignant gastric cancer is circumscribed by the selection of patients and up to 42% of respondents never use the laparoscopic approach, data which are found to be in line with published literature.22–24 Obviously, LS management of gastric cancer significantly correlates with the use of this approach for treatment of other gastric diseases.
The highest increase in laparoscopic use is in colorectal surgery, although its use drops as complexity rises. While ten years ago it was only used routinely by 33% of respondents,6 at present 57% use the laparoscopic approach for the treatment of benign colon disease, 51% use it for malignant disease and up to 43% for the treatment of rectal cancer. These figures exceed those recently published in literature.5,25
The use of LS for the treatment of solid organ disease is variable, as previously indicated in literature.26–28 Although this is normal in the case of adrenalectomy and simple liver cysts, its use is selected in splenic and tail of the pancreas diseases, where technical difficulty increases.
Finally, in general,4 trends in the management of morbid obesity have radically changed and are clearly laparoscopic, with just 1% of respondents routinely using open surgery. Some years ago this figure was 39%.
The opinion of Spanish surgeons on new technologies in LS is mainly positive, framed within the context of minimally invasive surgery. Furthermore, although its implementation is minimal, the survey illustrates the reality of the use of LS, which is chiefly through a single incision for the treatment of processes which are prevalent in especially dedicated groups, without it being related to type or size of hospital, or other variables. These findings are in line with those obtained from other studies.29
The respondents have assessed the overall level of development of LS their environment, and there has been a clear change in trends. Ten years ago over half of the surgeons believed that LS had not grown as expected,6 and at present 75%–86% consider that LS occupies an appropriate place in their environment.
Generally in Spain, basic LS procedures have developed to the extent that they are considered standard techniques practised by the majority of surgeons and are part of the basic training of surgical residents. Although the scenario has radically changed regarding advanced LS and usage percentages are high, deficits remain and there are consequently opportunities for improvement. A decade ago, Feliu et al.6 demonstrated that surgical training institutions were essential elements in ensuring the development of LS. Although there have clearly been advances in recent years, the findings from our survey have highlighted that difficulties in obtaining training and gaining experience are still the highest barriers for the development of advanced techniques for Spanish surgeons. The validity of the available training models is therefore questioned. As previously stated, it is difficult to identify an ideal model.30 However, once the advantages of endoscopic surgery in different areas have been demonstrated, a realistic objective for those in charge of surgical departments is to promote structured LS training from the initial stages of residence and the first years of professional practice, with a view to furthering gradual generational change and provide us with surgeons who are more highly trained in LS.
Finally, the debate as to whether LS is a specialty appears to be closed. The introduction of minimally invasive techniques in the different areas of specific knowledge of our speciality is common and it could be said that the old figure of the surgeon especially dedicated to LS has been replaced by one of an innovative surgeon, concerned about the advancement of minimally invasive therapies through emerging technologies.
Conflict of InterestThe authors declare that there is no conflict of interest.
To all AEC members who have collaborated by participating in this survey.
Please cite this article as: Moreno-Sanz C, Tenías-Burillo JM, Morales-Conde S, Balague-Ponz C, Díaz-Luis H, Enriquez-Valens P, et al. 25 años de cirugía laparoscópica en España. Cir Esp. 2014;92:232–239.