Body contouring surgery is in high demand following the increase in bariatric surgery. But these types of procedures are associated with high complication rates that cause long hospital stays and have a negative effect on patient satisfaction. The purpose of this study is to identify predictors of complications in order to optimize outcomes in these patients and find a relationship between complication rate and satisfaction.
Materials and methodsOut of a group of 175 post-bariatric patients, 72 patients underwent body contouring surgery following massive weight loss from 2003 to 2008. They were reviewed retrospectively for demographic data, pre- and postoperative weight status, co-morbidities and complications and reoperation rate. Patient satisfaction was evaluated.
Results(a) Complications: The overall complication rate was 45.8%. The most frequent were seromas (23.6%); infection (13.9%), bleeding (11.1%), hematoma (6.9%) (needing transfusions [6.9%]), skin necrosis (6.9%) and umbilical necrosis (4.2%). A total of 8 patients required reoperation (11.1%).
(b) Satisfaction rating: (1) very satisfied: 51.4%, (2) satisfied: 31.9%, (3) dissatisfied: 8.3%, (4) very dissatisfied: 8.3%.
(c) The presence of complications was significantly associated with patients’ satisfaction, reoperation rate and longer hospital stays (P<.001).
ConclusionsPost operative complications were frequent. No predictors could be found to prevent these complications and optimize patient selection and appropriate timing of surgery. Patients with complications had a significantly higher reoperation rate, longer hospital stay and more dissatisfaction. The patients’ satisfaction was negatively influenced by complication occurrence and not by the esthetic results.
Las abdominoplastias se han convertido en un proceso quirúrgico frecuente en pacientes con pérdida masiva de peso tras cirugía bariátrica. Este tipo de procedimientos no están exentos de complicaciones que afectan a la calidad de vida y satisfacción del paciente. El objetivo de este estudio es encontrar los factores de riesgo para desarrollar dichas complicaciones y evaluar la satisfacción de nuestros pacientes.
Material y métodosA un total de 72 pacientes, de los 175 intervenidos de cirugía bariátrica, se les realizó una abdominoplastia entre 2003 y 2008. Fueron revisados, retrospectivamente: datos demográficos, estado pre- y poscirugía, comorbilidades, tasa de complicaciones y reintervención. El nivel de satisfacción fue medido mediante una encuesta expresada en una escala tipo Likert. Se realizó un análisis comparativo de las distintas variables entre pacientes con y sin complicaciones.
Resultadosa) Complicaciones: tasa global del 45,5%. La más frecuente fue el seroma (23,6%); infección (13,9%), sangrado (11,1%), hematoma (6,9%) (requiriendo transfusión [6,9%]), necrosis de piel (6,9%) y necrosis umbilical (4,2%). Se reintervino a 8 pacientes (11,1%).
b) Satisfacción: 1) muy satisfecho: 51,4%; 2) satisfecho: 31,9%; 3) insatisfecho: 8,3%; 4) muy insatisfecho: 8,3%.
c) Se encuentra una relación estadísticamente significativa entre complicaciones, reintervención, estancia media y satisfacción (p<0,001).
ConclusiónLas complicaciones son relativamente frecuentes en este tipo de pacientes, alargando la estancia media y posteriores controles ambulatorios. No hemos identificado factores de riesgo que ayuden a prevenir este tipo de complicaciones. El grado de insatisfacción está en relación con las complicaciones postoperatorias del procedimiento quirúrgico y no con el resultado estético.
Bariatric surgery has made extraordinary advances in recent decades, especially since it has been demonstrated to be the only effective treatment for long-term weight loss in morbidly obese patients. After massive weight loss, the skin and subcutaneous abdominal tissue frequently transform into a mass of redundant, lax skin that requires surgical treatment because of the physical and psychosocial effects that this condition causes the patient. Although in the long term this operation is associated with better quality of life and patient satisfaction, the high rates of postoperative complications, such as bleeding or seroma, initially influence patient expectations.
Despite the progressive increase in the number of patients who undergo abdominoplasty, few authors publish complication rates, and there is great controversy about associated risk factors.
In this study, we analyzed: (1) the results of abdominoplasties in patients with previous bariatric surgery in order to identify the risk factors for complications, optimize patient selection and better adjust the period between bariatric surgery and later abdominal reconstructive surgery; (2) the factors that influence patient satisfaction.
Patients and MethodsPatientsThe series is made up of 175 cases that underwent bariatric surgery for morbid obesity. Afterwards, 72 patients (21 males and 51 females; mean age 43.5±10.7) had dermolipectomy and abdominoplasty at the Hospital Universitario José María Morales Meseguer. The surgery was performed by 3 general and gastrointestinal surgeons with experience in bariatric surgery. The study covers a 5-year period (January 2003 to February 2008).
Study Variables- -
Demographic data, including age and sex, type of bariatric surgery, body mass index (BMI), weight loss in both surgeries and associated comorbidities, time transpired between surgeries, mean hospital stay and rate of re-operation
- -
Albumin and hemoglobin levels
- -
Presence of incisional hernia, its diagnosis and type of repair
- -
Postoperative complications
- -
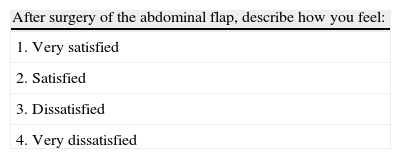
Six months after surgery, patient satisfaction was calculated in order to evaluate abdominoplasty results using a simple survey with a Likert scale from 1 (very satisfied) to 4 (very unsatisfied) (Table 1). This scale was applied by an independent observer (resident physician of the Surgery Department) in a personal interview with the patients.
The data collected included weight loss and gain, BMI and patient medical history centered on associated comorbidities.
The surgeons examined the characteristics of the skin and fat in order to determine the thickness and mobility of the flap and its interaction with daily activities. Scar tissue and hernias were also identified.
After the bariatric surgery, the patients had scheduled office visits with an endocrinologist who monitored patient weight and diet after surgery as well as diabetes, which is prevalent in this type of patients. If patients do not present a stabilized weight in the period of 6 months-one year before dermolipectomy, the procedure is not recommended. It is also not recommended in patients with BMI >35. The reason for adjusting surgical times is for patients to have appropriate nutritional and metabolic status, which provides a lower risk of complications and allows patients to reach their ideal weight in order to obtain better esthetic results. Patients with albumin <4g/dl or hemoglobin <12g/dl were not treated surgically.
Related contraindications are smoking, severe cardiopulmonary disease or important psychiatric alterations. As for smoking, Krueger and Rohrich1 recommend abstaining from smoking 4 weeks before and 4 weeks after the scheduled surgery. If the patient cannot stop smoking, Manassa recommends limiting the dissection and resection of the skin flap.2
Finally, patients were informed about the benefits and risks of the intervention. In addition, patients were asked why they had decided to undergo the procedure (functional or esthetic problems) and what expectations they had for the surgery.
Description of the TechniqueAs the first surgical technique, the 72 patients underwent gastric bypass for morbid obesity. Laparotomy was used in 14 cases, while the approach was laparoscopic in the other 58, 2 of which had to be converted to open surgery. After a mean time transpired between surgeries of 28.9±16.9 months, dermolipectomy and abdominoplasty were scheduled.
The dermolipectomy surgical technique included the following steps:
- -
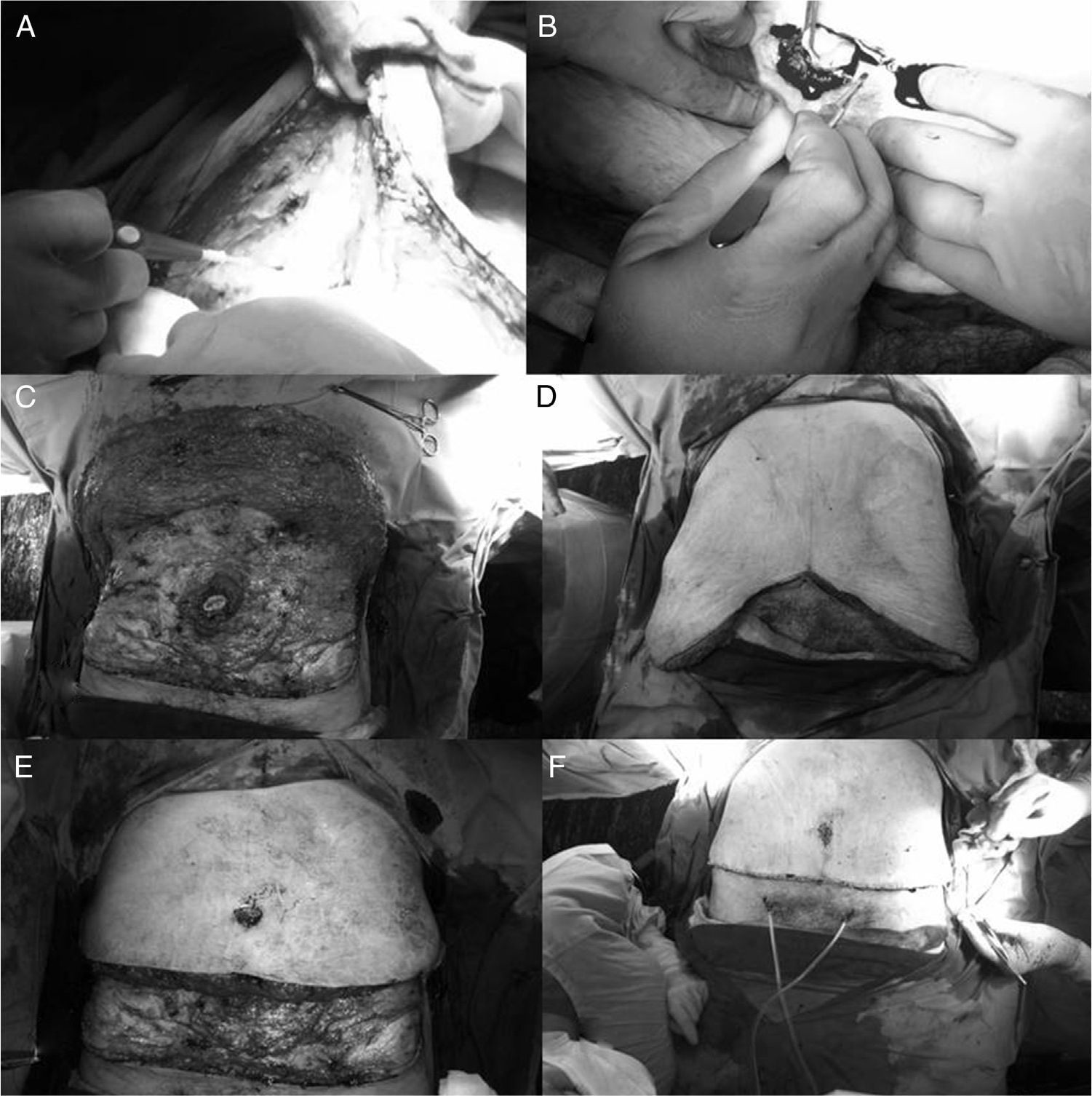
An incision was made at the upper edge of the pubic triangle that was extended horizontally toward both sides to both anterior superior iliac spines (Fig. 1A).
Fig. 1.Intraoperative images: (A) detaching the upper flap; (B) peri-umbilical incision; (C) detaching the upper flap until the costal edge, preserving the navel; (D) estimation of the tissue to be resected; (E) resection of the excess tissue; (F) suturing the new navel, placement of drains and closure by planes.
(0.26MB). - -
Supra-aponeurotic cranial detachment of the upper edge. The large flap is lifted and cut along the midline to the navel where, by means of a circular incision, it is separated from the abdominal flap, continuing up to the xiphoid appendix and costal margins (Fig. 1 B and C).
- -
The operating table is raised to an angle of 15° in anti-Trendelenburg position, using a temporary midline suture to secure the flap. The assistant pulls down on each side of the upper flap to estimate the excess tissue to be resected (Fig. 1D and E).
- -
The position is marked to externalize the navel before the final suture. The navel is externalized with the aid of long stitches and it is secured to the surrounding skin with nylon 6/0 sutures with simple interrupted stitches. Two suction drains are placed and closure is performed (Fig. 1F).
Antibiotic prophylaxis was used with second- or third-generation cephalosporins and thromboembolism prophylaxis included low molecular weight heparin in all cases.
Statistical AnalysisThe comparison between qualitative variables was done by applying Pearson's χ2 test, χ2 for linear trends and Fisher's exact test. The comparison between quantitative and qualitative variables was analyzed with Student's t test if the quantitative variable had a normal distribution and with the Mann–Whitney test if the distribution was non-parametric.
The variables that in the univariate analysis reached a level of significance of P<0.1 were entered into a multivariate analysis using logistic regression, calculating the “odds ratio” with a 95% confidence interval. The SPSS version 15.0 program for Windows was used (SPSS; Chicago, IL, USA).
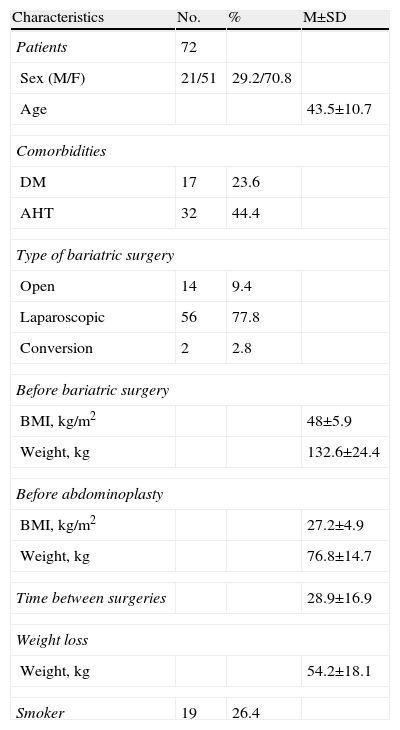
ResultsThis study included 72 patients who underwent abdominoplasty after bariatric surgery. Their general characteristics appear in Table 2.
General Characteristics of the 72 Patients Treated.
| Characteristics | No. | % | M±SD |
| Patients | 72 | ||
| Sex (M/F) | 21/51 | 29.2/70.8 | |
| Age | 43.5±10.7 | ||
| Comorbidities | |||
| DM | 17 | 23.6 | |
| AHT | 32 | 44.4 | |
| Type of bariatric surgery | |||
| Open | 14 | 9.4 | |
| Laparoscopic | 56 | 77.8 | |
| Conversion | 2 | 2.8 | |
| Before bariatric surgery | |||
| BMI, kg/m2 | 48±5.9 | ||
| Weight, kg | 132.6±24.4 | ||
| Before abdominoplasty | |||
| BMI, kg/m2 | 27.2±4.9 | ||
| Weight, kg | 76.8±14.7 | ||
| Time between surgeries | 28.9±16.9 | ||
| Weight loss | |||
| Weight, kg | 54.2±18.1 | ||
| Smoker | 19 | 26.4 | |
Thirty-three of these patients presented some type of complication (45.8%), the most frequent of which was seroma (23.6%). Others included: infection (13.9%), bleeding (11.1%) and important hematoma (6.9%) that required transfusion (6.9%), necrosis of the skin (6.9%) and necrosis of the navel (4.2%). Eight patients needed re-operation (11.1%). There was no postoperative mortality.
Comorbidities were frequent, such as arterial hypertension (44.4%) and diabetes mellitus (23.6%). With regard to smoking, 26.4% of the patients were smokers; 24.2% of the smokers suffered some type of complication, while in the group of non-smokers the complication rate was 28.2%. In the comparative study of the different complications and comorbidities as risk factors for complications, no statistically significant correlation was found.
In blood tests, mean albumin levels were 4.18g/dl and mean hemoglobin was 13.19g/dl.
Using a survey, the level of satisfaction 6 months after surgery scored: grade 1 (very satisfied) 51.4%; grade 2 (satisfied) 31.9%; grade 3 (unsatisfied) 8.3%; grade 4 (very unsatisfied) 8.3%.
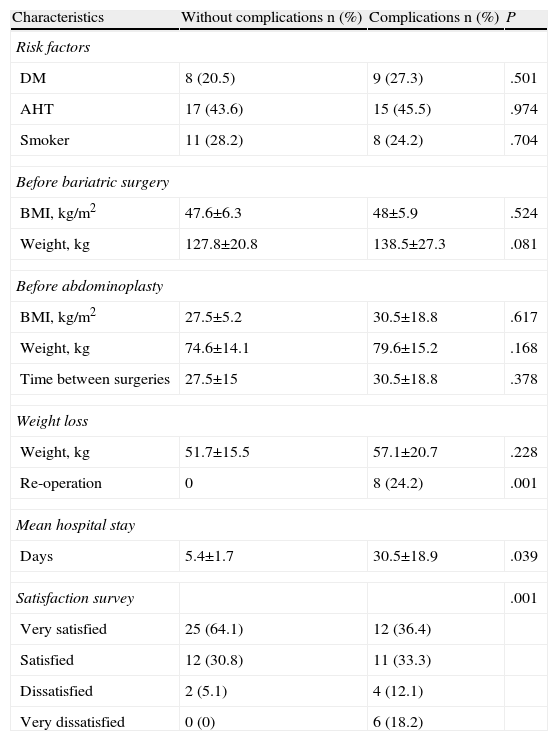
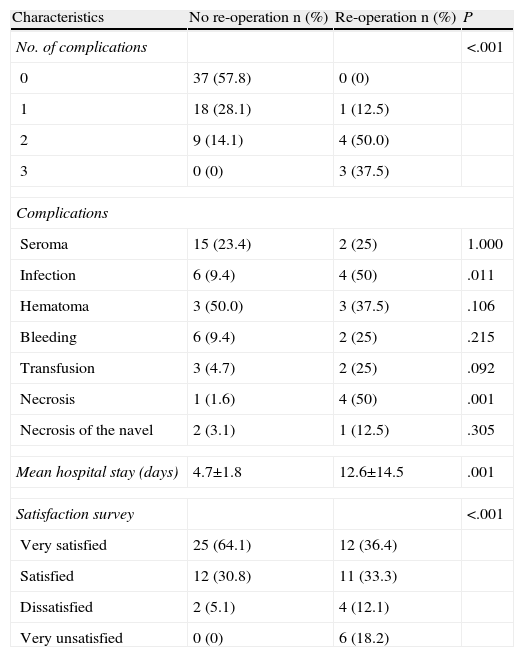
As for the comparative study among patients with (n=33) or without complications (n=39) with the different variables studied, we observed that there was no difference between the two groups regarding demographic variables, comorbidities and pre- and post-surgical status. There were significant differences in the degree of satisfaction of the patients (P<.001) when compared with the appearance of complications and re-operation. Eight patients were re-operated on (24.2%) out of the 33 that presented complications, 4 due to bleeding and 4 for debridement and cleaning of the wound due to infection. There was a correlation between the number of complications and the re-operation rate. A significant relationship was found between the increased mean hospital stay and the higher rate of re-operation (4.7±1.8 days in non-re-operated patients vs 12.6±14.5 days of re-operated patients) and therefore the lower degree of satisfaction (P<.001) (Tables 3 and 4).
Comparative Study Between Patients With (n=33) or Without Complications (n=39) and the Different Variables.
| Characteristics | Without complications n (%) | Complications n (%) | P |
| Risk factors | |||
| DM | 8 (20.5) | 9 (27.3) | .501 |
| AHT | 17 (43.6) | 15 (45.5) | .974 |
| Smoker | 11 (28.2) | 8 (24.2) | .704 |
| Before bariatric surgery | |||
| BMI, kg/m2 | 47.6±6.3 | 48±5.9 | .524 |
| Weight, kg | 127.8±20.8 | 138.5±27.3 | .081 |
| Before abdominoplasty | |||
| BMI, kg/m2 | 27.5±5.2 | 30.5±18.8 | .617 |
| Weight, kg | 74.6±14.1 | 79.6±15.2 | .168 |
| Time between surgeries | 27.5±15 | 30.5±18.8 | .378 |
| Weight loss | |||
| Weight, kg | 51.7±15.5 | 57.1±20.7 | .228 |
| Re-operation | 0 | 8 (24.2) | .001 |
| Mean hospital stay | |||
| Days | 5.4±1.7 | 30.5±18.9 | .039 |
| Satisfaction survey | .001 | ||
| Very satisfied | 25 (64.1) | 12 (36.4) | |
| Satisfied | 12 (30.8) | 11 (33.3) | |
| Dissatisfied | 2 (5.1) | 4 (12.1) | |
| Very dissatisfied | 0 (0) | 6 (18.2) | |
Comparison Between Patients Who Required and Those Who Did Not Require Re-operation.
| Characteristics | No re-operation n (%) | Re-operation n (%) | P |
| No. of complications | <.001 | ||
| 0 | 37 (57.8) | 0 (0) | |
| 1 | 18 (28.1) | 1 (12.5) | |
| 2 | 9 (14.1) | 4 (50.0) | |
| 3 | 0 (0) | 3 (37.5) | |
| Complications | |||
| Seroma | 15 (23.4) | 2 (25) | 1.000 |
| Infection | 6 (9.4) | 4 (50) | .011 |
| Hematoma | 3 (50.0) | 3 (37.5) | .106 |
| Bleeding | 6 (9.4) | 2 (25) | .215 |
| Transfusion | 3 (4.7) | 2 (25) | .092 |
| Necrosis | 1 (1.6) | 4 (50) | .001 |
| Necrosis of the navel | 2 (3.1) | 1 (12.5) | .305 |
| Mean hospital stay (days) | 4.7±1.8 | 12.6±14.5 | .001 |
| Satisfaction survey | <.001 | ||
| Very satisfied | 25 (64.1) | 12 (36.4) | |
| Satisfied | 12 (30.8) | 11 (33.3) | |
| Dissatisfied | 2 (5.1) | 4 (12.1) | |
| Very unsatisfied | 0 (0) | 6 (18.2) | |
After the univariate comparison, a multivariate model was constructed, and the only variable that was an independent predictor for re-operation was the number of complications, with an OR of 16.89 (95%CI: 2.52–112.75; P=.004).
In 9 patients (6.4%), there was a coexisting midline incisional hernia. In the laparoscopic surgery group (5 patients), the location was in the area of the supraumbilical trocar, while in the cases with open surgery (4 patients) the hernia was in some segment of the incisional scar. In 7 patients, due to the small size of the orifice, the hernias were corrected with simple sutures, and the remaining 2 cases required PPL mesh placement.
DiscussionObesity has become the epidemic of the 20th century. Along with it, the practice of bariatric surgery has increased enormously in recent decades and is considered the only long-term solution to the problem. At the same time, the number of post-bariatric surgery patients looking for a solution to the excess skin and subcutaneous tissue after massive weight loss has likewise increased.3,4
Dermolipectomy with abdominoplasty is a frequent surgical procedure, with more than 100 years of experience since it was first described by Kelly5 in 1899. In 1977, Grazer and Goldwyn6 were the first to report the complications of abdominoplasties. They surveyed 958 plastic surgeons and, by reviewing 10490 surgical interventions, they found an overall rate of complications of about 14%. Hensel7 published a rate of 32%, Van Uchelen8 24% and Stewart9 18%. All these series contained cases of abdominoplasty done in the general population. There are fewer publications about obese patients and post-bariatric surgery.10
In this retrospective study, we analyzed 72 patients who had undergone dermolipectomy and abdominoplasty. The overall rate of complications was 45.8%, which concurs with other percentages provided by the literature (20%–50%).3,11,12 The most frequent complication is seroma, which in our experience was 23.6% and ranged in other publications from 0.3% to 90%.13
In the literature, there are different studies that analyze the complications associated with these procedures and there is great controversy about the associated risk factors and the possibility of preventing these complications.3 We have not been able to find any risk factors that can be influenced in order to avoid complications, according to the associated comorbidities such diabetes mellitus, arterial hypertension, BMI or smoking as proposed by many papers, all of which are associated with high rates of complications.11 Nevertheless, since the number of patients with comorbidities in our study is small, we cannot make any specific recommendations.
In 1977, Mosely and Finseth14 reported the effects of smoking on wound healing. There are studies that have found a greater incidence of flap necrosis, wound dehiscence and poorer esthetic results in smokers.1,14,15 In 2003, Manassa et al.2 found a wound infection rate of 47.9% in smokers and only 14.8% in non-smokers. In our paper, we have not found differences, although our results could be influenced by our recommendation to quit smoking or to reduce tobacco consumption both 4 weeks before and 4 weeks after surgery.16
Other studies, like the one by De Ciuceis,17 have demonstrated that arterial hypertension and diabetes affect microvascularization and capillaries, which influences tissue perfusion and the exchange of nutrients and has negative consequences for proper healing. In our study, the presence of these comorbidities did not have a significant influence on the results, probably due to the thorough preoperative preparation involving a multidisciplinary team from different specialties (endocrinologists, anesthetists, etc.).
Like Kerviler,18 we believe in the importance of stabilized weight. Bariatric surgery causes a nutritional imbalance, resulting in vitamin and protein deficiencies that have a negative effect on healing. During the first year, these patients have a low nutritional reserve as they lose 50% of vitamins and proteins. This is why we wait about 24 months after bariatric surgery before the second surgical intervention. In one study, Agha-Mohamadi and Hurwitz19 found a lower rate of complications when patients were administered nutritional support. Although it is not quite clear how this influences abdominoplasty, the results emphasize the importance of the timing between surgeries.
Massive weight loss produces excess skin that creates new psychological and functional consequences such as hygiene problems, rash or infection, sex life limitations, embarrassment or problems in personal relationships. There have been many studies3,20 published about the quality of life of patients after bariatric surgery, and there are even papers3,4 that show how strikingly unprepared patients are for the consequences of massive weight loss. This may also negatively affect quality of life just as much as the previous obesity did, and may even be a risk for weight gain.
In our series, we measured the level of satisfaction with a simple survey using the Likert scale, which showed the high rate of satisfaction (>80%) of our patients. In the personal interview with an independent observer, the degree of dissatisfaction was fundamentally related to the postoperative complications of the surgical procedure and, curiously, not with the esthetic result.
As for the comparative study between patients with (n=33) or without (n=39) complications, we found a significant correlation between longer hospital stay and higher rate of re-operations and, therefore, a lower degree of satisfaction in patients who have some type of complication and a longer postoperative recovery. There were no cases of postoperative mortality. In spite of being a routine procedure, this type of surgery entails an important rate of complications, as over 10% of patients require re-operation. This prolongs mean hospital stays, which is the most influential determinant in the cost-effectiveness of the procedure.21 Therefore, after observing the high incidence of complications in our series, different prevention strategies have been proposed: shortening surgical times in order to reduce hypothermia and excessive tissue exposure, avoiding extensive resections that increase the risk of hemorrhage and infection, limiting the superior dissection or surgery done in two different procedures, the use of the harmonic scalpel to improve coagulation and the sealing of vessels, or new surgical glues to prevent seromas or hematomas.
In our practice, we often find patients with great expectations prior to abdominoplasty, based on either the experience of someone they know or from the internet. It is for this reason that we believe it is extremely important to inform these patients in the preoperative period and bring them around to a more realistic way of thinking.
This is the counterpoint to specialists who underestimated the role of reconstructive surgery after bariatric surgery, which they thought of as mere plastic surgery. Later research, however, has concluded that it has a positive effect on patients.3,4,22 Therefore, reconstructive surgery should be included in the continued treatment of patients who undergo morbid obesity surgery as it will also contribute to improving the long-term results of bariatric surgery.
ConclusionComplications during the immediate postoperative period as well as after discharge are relatively frequent. This lengthens both mean hospital stay along with later follow-ups in the outpatient setting. In our study, we have not identified risk factors that help prevent this type of complications, which makes it important to provide patients with the correct information about this type of surgery.
Nevertheless, the degree of dissatisfaction is related with the post-operative complications of the surgical procedure and not with the esthetic results. In spite of all of this, reconstructive surgery should be included in the treatment of patients who undergo bariatric surgery as it contributes to improving long-term results.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: García-García ML, Martín-Lorenzo JG, Campillo-Soto Á, Torralba-Martínez JA, Lirón-Ruiz R, Miguel-Perelló J, et al. Complicaciones y nivel de satisfacción tras la realización de una dermolipectomía y abdominoplastia después de efectuar una cirugía bariátrica. Cir Esp. 2014;92:254–260.