The usefulness of percutaneous needles (PN) to replace traditional assistance ports in mini-invasive techniques with a single port is analyzed and their feasibility for conducting a single port laparoscopic cholecystectomy (SPLC) is demonstrated.
Material and methodsA retrospective, linear and descriptive study covering 2431 patients with a diagnosis of acute and non-acute gallbladder disease has been conducted. The patients underwent a single port laparoscopic cholecystectomy using some type of PNs, replacing the assisting ports used in traditional laparoscopic cholecystectomy (TLC). Based on the progressive use of PNs–reins (R), hooked needles (HN) and passing suture needles (PSN)–to carry out the SPLC technique, 3 groups have been established: A, B and C. The results were compared using a Student t test, odds ratio and CI and were analyzed by means of the SPSS software v. 13.0.
ResultsThe use of PNs showed an increased feasibility for the laparoscopic procedure, as they were included in the surgical technique. The R were useful when carrying out the SPLC in 78% of the cases and when the HK were added, the results increased to 88%. When using the 3 types (R, HN and PSN), the results increased by 96%. Statistical significance was obtained with these values: chi 2=67.13 and P<.001; odds ratio and 95% CI became significant when comparing the B/C, A/C, and A–B/C groups.
ConclusionsThe PNs, replacing the assisting ports in laparoscopy, make it possible to attain a feasibility of the process in 96% of the cases. This percentage was similar to what is achieved with the TLC, which places the one port laparoscopy surgery technique as an advantageous and economic alternative. This application of the PNs could be made extensive to other single-port techniques, with a multi-valve platform and natural orifice surgery.
Se analiza la utilidad de agujas percutáneas (AP) sustituyendo puertos de asistencia tradicionales en técnicas miniinvasivas de puerto único, mostrando su factibilidad al realizar colecistectomía laparoscópica con un puerto (CL1P).
Material y métodosEstudio retrospectivo, lineal y descriptivo de 2.431 pacientes intervenidos de CL1P, por enfermedad vesicular aguda y no aguda utilizando algún tipo de AP, sustituyendo los puertos asistenciales usados en colecistectomía laparoscópica tradicional (CLT).
Basado en el uso progresivo de AP: riendas (R), aguja-gancho (AG) y aguja pasa hilos (APH) al desarrollar la técnica CL1P, dividimos 3 grupos: A, B y C. Se compararon resultados utilizando T de student, odds ratio e IC, analizándolos mediante SPSS 13.0.
ResultadosEl uso de las AP mostró incremento en la factibilidad del procedimiento laparoscópico, conforme se integraron en la técnica quirúrgica. Las R tuvieron factibilidad de realizar CL1P en 78% de los casos, integrando AG aumentó a 88% y utilizando R, AG y APH en 96%. Hubo significación estadística con valores: Ji2 de 67,13 y p < 0,001; odds ratio e IC (95%) obtuvieron significación comparando grupos B/C, A/C y A-B/C.
ConclusionesLas AP, sustituyendo puertos asistenciales, permiten alcanzar factibilidad del procedimiento en el 96% de los casos, semejante al que se logra con la CLT, lo cual coloca a la técnica CL1P como una alternativa ventajosa y económica. Esta aplicación de las AP podría ser extensiva a otras técnicas de puerto único, con plataforma multivalvular, y a la cirugía por orificios naturales.
Since 2004, when Anthony Kalloo proposed the new surgical trend of natural orifice transluminal endoscopic surgery (NOTES),1 there have been well-known technical difficulties for the transluminal access of the abdominal cavity through the stomach or colon. This access was based on thin, fragile, weak assisting instruments which, in addition to having a small “biting” action, lack the strength for traction, resulting in inadequate triangulation, unstable insufflation, slow and unsafe hemostasis in addition to the difficulties in closing the stomach.2
This led to the navel becoming the optimal embryological orifice for access. In an attempt to improve esthetic results with the least amount of trauma to the abdominal wall, single-port surgery was developed using multi-instrument trocars.3–6 While there continue to be difficulties with adequate triangulation, crossing of hands, dueling of instruments, laborious navel opening and closure,7–9 attempts have been made at resolving these factors with solutions using special optics sucha as the endoeye, spider and flexible endoscopy.10–12 Some publications describe the use of traction threads for the triangulation of tissues and to release clamps in the multi-instrument port,3,5,10,13–20 significantly reducing the rate of complications compared with the use of instruments.21 Neodymium magnets and secured independent tools have also been used to facilitate single-port surgery.22,23
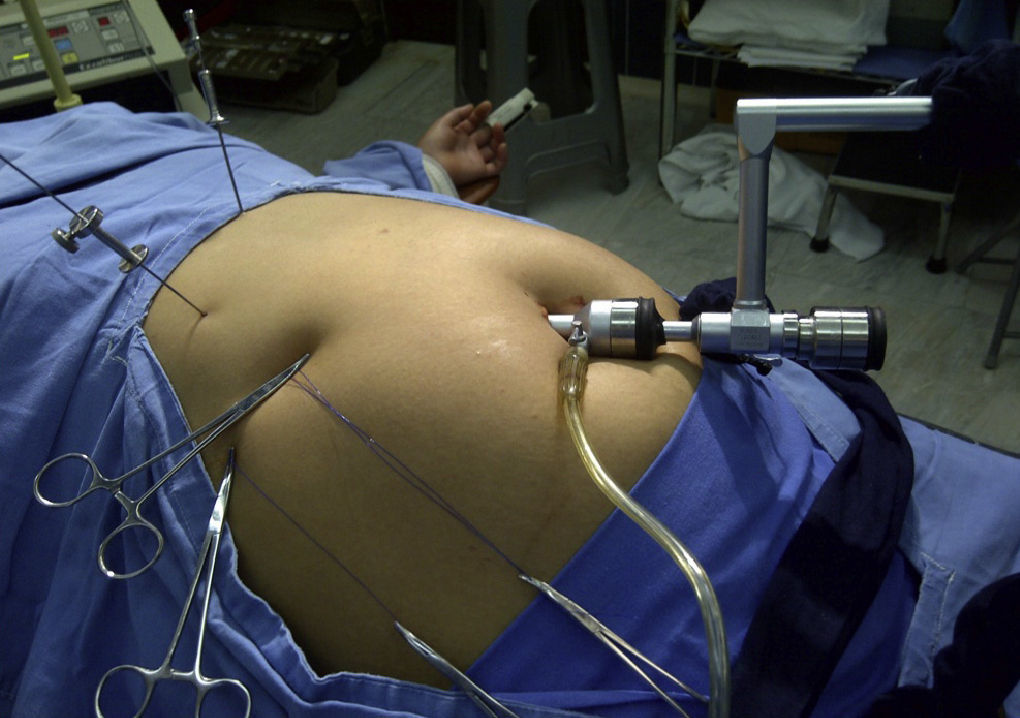
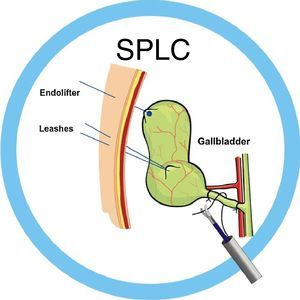
Our surgery group initiated single-port laparoscopic cholecystectomy (SPLC) in 1997, using a 12mm umbilical port24 (Fig. 1), an 11mm surgical laparoscope with a 6mm working channel for the introduction of laparoscopic instruments (5cm×43cm) (Fig. 2), assisted with the use of different types of percutaneous needles (PN).
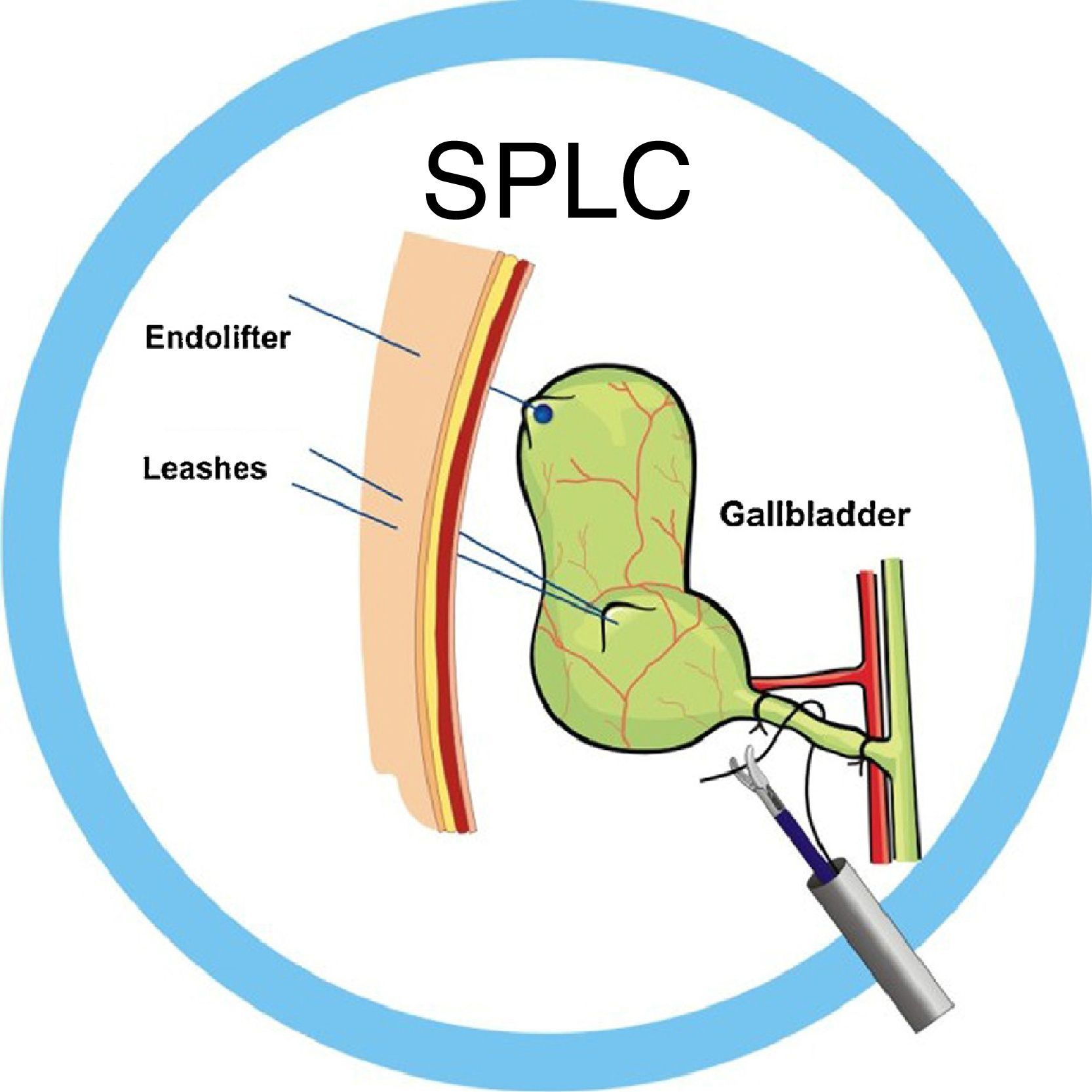
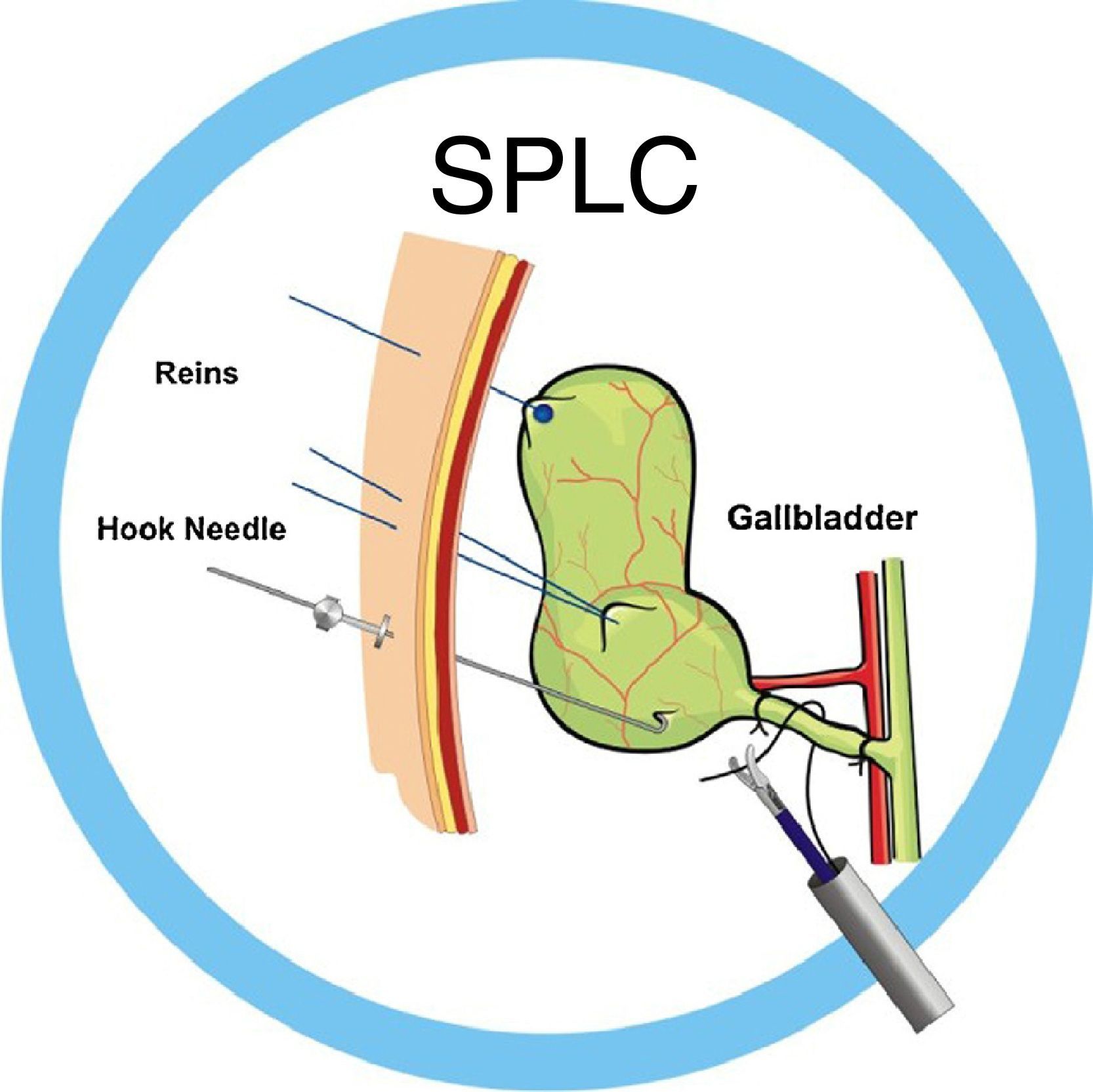
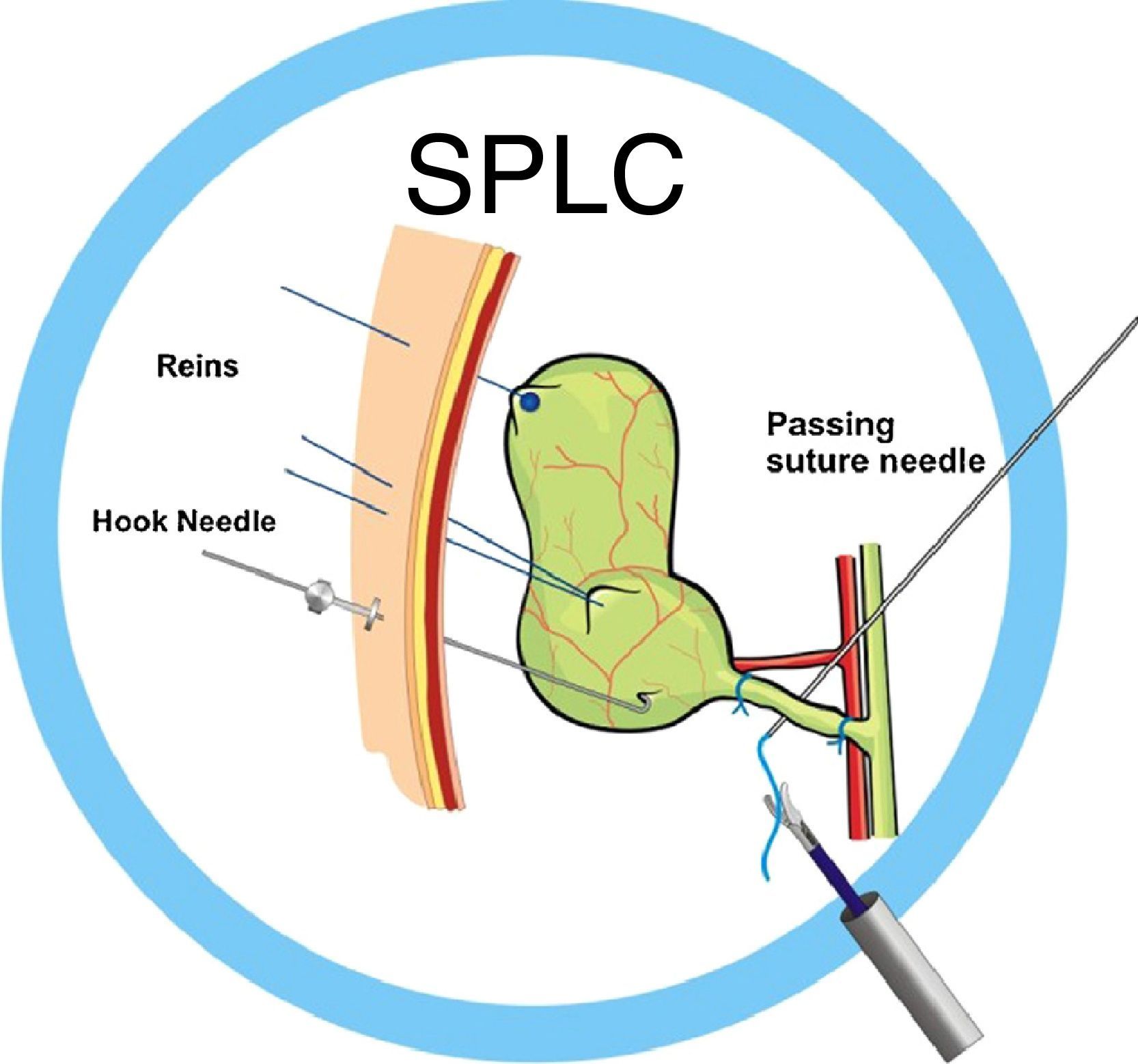
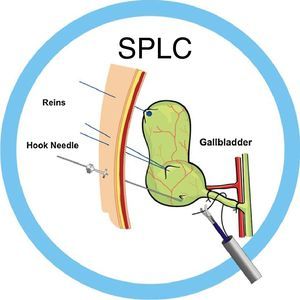
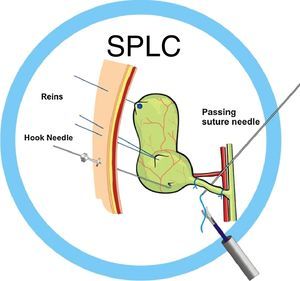
In the first procedures of laparoscopic cholecystectomy, we used 2 traction reins: a laparo-rein (R1)25,26 placed in the bottom of the gallbladder and another leash (R2)27 was introduced percutaneously in Hartmann's pouch for adequate gallbladder traction, although unidirectional (Fig. 3). To achieve lateral mobilization of the gallbladder, a hook-needle (HN) was used27 (Fig. 4). We finally added a suture passing needle (SPN),27 which facilitates the passage of the suture behind the structure to be ligated (Fig. 5) and functions as a retractor or liver separator, performing the functions of contraction during the dissection of the triangle of Calot and the hemostatic maneuvers, if necessary. This technique was used without patient selection both in acute and non-acute gallbladder disease.24,28
The objective of this paper is to present the role that PN play by substituting traditional laparoscopic cholecystectomy (TLC) assisting ports and the feasibility of their use in single-port techniques.
Material and MethodsA retrospective, linear and descriptive study from December 1997 to December 2010 at the Hospital Regional Sesver and Hospital Fausto Dávila Solís, both in Poza Rica (Veracruz, Mexico). The non-probabilistic sample included 2431 patients who had undergone SPLC using some type of PN substituting assisting ports used in TLC. The patients had given their informed consent for the procedures.
The inclusion criteria were: patients of both sexes, of any age, with acute and non-acute disease. Excluded from the study were those patients with a diagnosis of gallbladder cancer or choledocholithiasis and those with contraindications for laparoscopic surgery. The patients were classified into 3 groups depending on the type of PN used for the SPLC technique: group A – patients in whom two types of reins were used (R1-R2); group B–patients in whom R1-R2 were used along with HN; and group C – patients in whom R1-R2, HN and SPN were used. The specialized instruments as well as the PN (R1, HN and SPN) were all made by our team.
The R2 were made with a 75cm nylon 2–0 suture with a 60mm straight cutting needle (Mononylon, Ethicon®). The R1 were created by adding a 3mm×2mm silastic button to the end opposite the needle.
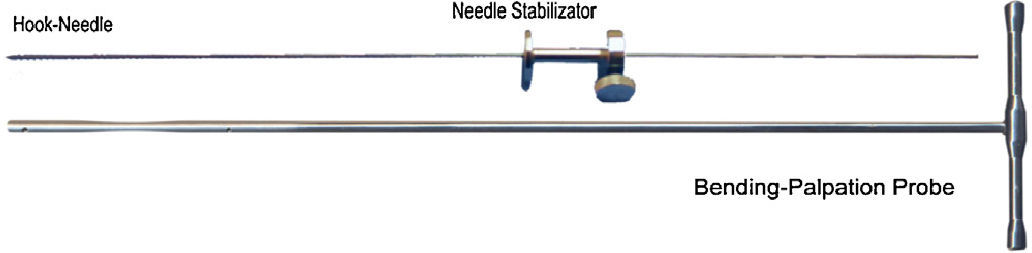
The HN are 20cm-long surgical stainless steel needles with a cutting tip at one end.
The SPN are 17cm long, 1.6mm in diameter and come with a punch that enables them to be introduced into the cavity. One end has a Luer-Lok fitting to make it easier to introduce the suture in the abdominal cavity.
Patient medical reports were used to collect the data. The variables analyzed in the 3 groups were: feasibility for carrying out laparoscopic cholecystectomy with the SPLC technique, without the need to convert the procedure to traditional laparoscopic cholecystectomy (TLC) or open cholecystectomy (OC) and operative time.
Feasibility was defined as the availability of surgical, technical and material resources in order to reproduce the established SPLC technique, as well as the skills and experience necessary to perform it (PN in all 3 modalities: R1-R2, HN and SPN) with the instruments necessary to ensure the benefits of this mini-invasive technique for scarless surgery. This variable was measured with the criteria that are used to define the conversion to TLC or to OC: the need to resort to elements or assisting ports used in TLC, using a subxiphoid port and 2 subcostal ports or mini-instruments; and second, if the open technique was resorted to (OC).
The operative time is defined as the time used from the beginning of the surgical procedure with the skin incision until concluding total incision closure. This was measured in minutes.
These variables were subjected to the recommended descriptive statistical analysis. For qualitative variables, Chi2 and OR (odds ratio) were used. Our results are expressed with OR values and 95% confidence intervals (95% CI). A P≤.05 was considered statistically significant. Quantitative variables are expressed with means and SD.
The SPLC technique or scarless surgery is explained in the textbook written by the author.28 With the recommended pneumoperitoneum through the umbilical incision, a 12mm laparoscopic port is placed to provide access for a 10mm surgical laparoscope (0°, 27cm) with a 6mm working channel (CL-11-1145S). In the subxiphoid region, the SPN (CL-4005 Suture Passing Needle) is introduced percutaneously, the mandrel is withdrawn and the right liver lobe is raised, exposing the gallbladder. A straight needle (1mm diameter) is introduced percutaneously in the subcostal region along the mid-clavicular line. It is bent with the needle-bending instrument (CL-2005-45 Bending-Palpation Probe), creating a 45° hook that is used to raise the gallbladder and expose the bottom of the gallbladder. The HN (CL-2005-HN2), fitted with a stabilizer (CL-4006 Needle Stabilizer) at its extra-abdominal end for manipulation and fixation, provides the traction necessary to dissect the tissues (Fig. 6).
After exposing the top of the gallbladder, a 60mm-long straight needle with 2/0 nylon (U6042-75LT Atramat) is introduced into the cavity through the working channel of the laparoscope with Kelly forceps (13-1419i-45), passing through the bottom of the gallbladder and coming out at the subcostal/anterior axillary line, creating traction with the R1, bringing the top of the gallbladder to the wall of the abdomen, securing the R1 with the Kelly forceps, flush with the skin. The gallbladder content is suctioned with a suction needle (CL-3005-45 1.8mm Puncture Needle) through the channel of the surgical laparoscope at Hartmann's pouch. The HN is resituated in the body of the gallbladder, exposing Hartmann's pouch, where the R2 was placed, with percutaneous introduction and exteriorization, 4cm under the HN, favoring the exposure of the hepatic hilum during dissection and the cleavage plane during gallbladder detachment.
At this time, the gallbladder traction (bottom and Hartmann's pouch) with the reins and the placement of the HN provides exposure and facilitates the dissection of the critical elements of Calot's triangle, which is performed with laparoscopic Kelly forceps (13-1419i-45) and the 90° dissecting spatula (CL-2001-45) aided by the SPN acting as a liver retractor with the necessary countertraction. Once the cystic artery and duct are visible and dissected, the SPN is placed behind the cystic duct, introducing a polyamide or polypropylene 2/0 suture measuring 150cm in length (SS-0642-150NL Anchor Suture, Atramat), surrounding it and extracting both suture ends through the laparoscope, ligating with an extracorporeal Roeder or GEA knot,29 positioning it in the desired site with a knot pusher with integrated cut (CL-2002-45). We repeat the procedure, leaving one distal and 2 proximal knots, which are cut with scissors (13-1309i-45 Metzenbaum Scissor).
The same is done with the cystic artery, detaching the gallbladder with an insulated hook (CL-2010-45 Telescopic Electrode-L-shaped), manipulating the PN and favoring optimal exposure. Once the cholecystectomy has concluded, we withdraw the HN from the gallbladder, extracting it with claw forceps (13-1606i-45) through the umbilical port, or unbending it with the needle-bending instrument and extracting it through the abdominal wall. The surgical specimen was extracted through the umbilical orifice together with the umbilical port and the laparoscope.
If needed, we leave a mini-drain (child feeding tube, K-31) with the catheter introduction syringe (CL-4003-45). The SPN allows for raising the right liver lobe and reviewing the bed, suctioning CO2 with a suction cannula (CL-3006-45 and 31-2258). We only close the anterior aponeurosis at the umbilical level using size 0 nylon or polypropylene, using a hook for the closure of the aponeurosis (CL-2004). No stitch or suture are used in any of the micro-orifices of the percutaneous needles or at the umbilical opening, where the skin edges are brought together with the help of a 20cm elastic bandage. The coordination and understanding of the technique by the surgical team (surgeons, assistants and surgical technician) are essential for it to be performed optimally.
In the beginning, the SPLC technique was performed with a combination of Storz laparoscopic instruments and others we had made ourselves (needle bender instrument, insulated telescopic hook, knot pusher with integrated cut) and the PN (R1, HN and SPN). Currently, the instruments and endo-sutures have been perfected for the technique and are manufactured by the Compañía Internacional Farmacéutica (IFSA®).
The R2 are currently being substituted with R1 (U6042075LT), which, with their stoppage mechanism, avoid an entry micro-orifice in the skin.28
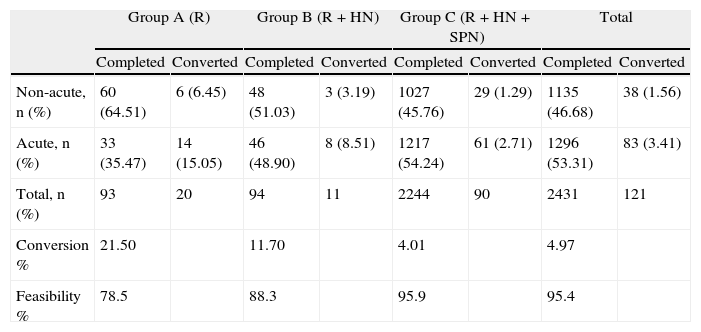
ResultsResults can be observed in Table 1, in accordance with acute or scheduled gallbladder disease for group A (December 1997–June 1998), using only 2 assisting reins (R1-R2), 93 patients were treated surgically, 20 of which were converted (21.50%): 17 (18.27%) to TLC and 3 (3.22%) to OC. The feasibility rate was 78.49% and mean operative time was 96min.
Feasibility Percentage by Acute or Non-acute Disease and Groups Classified According to the Type of Percutaneous Needles Used.
| Group A (R) | Group B (R+HN) | Group C (R+HN+SPN) | Total | |||||
| Completed | Converted | Completed | Converted | Completed | Converted | Completed | Converted | |
| Non-acute, n (%) | 60 (64.51) | 6 (6.45) | 48 (51.03) | 3 (3.19) | 1027 (45.76) | 29 (1.29) | 1135 (46.68) | 38 (1.56) |
| Acute, n (%) | 33 (35.47) | 14 (15.05) | 46 (48.90) | 8 (8.51) | 1217 (54.24) | 61 (2.71) | 1296 (53.31) | 83 (3.41) |
| Total, n (%) | 93 | 20 | 94 | 11 | 2244 | 90 | 2431 | 121 |
| Conversion % | 21.50 | 11.70 | 4.01 | 4.97 | ||||
| Feasibility % | 78.5 | 88.3 | 95.9 | 95.4 | ||||
Group A using reins; group B using reins and hook-needle (R+HN); group C using reins, hook-needle and suture passing needles (R+HN+SPN).
In group B (July 1998–December 1998), using 2 classes of PN (R1-R2 and HN), we operated on 94 patients, converting 11 (11.7%): 7 to TLC (7.44%) and 4 to OC (4.25%). The feasibility was 88.29% and mean surgical time 78min.
In group C (January 1999–December 2010), using 3 types of PN (R1-R2, HN and SPN), 2244 patients were operated on. 90 patients were converted (4.01%): 23 (1.02%) to TLC and 67 (2.98%) to OC, with a feasibility of 95.98% and mean operative time of 68min.
Mean operative time of the 3 groups was 80.66min (range 15–230min).
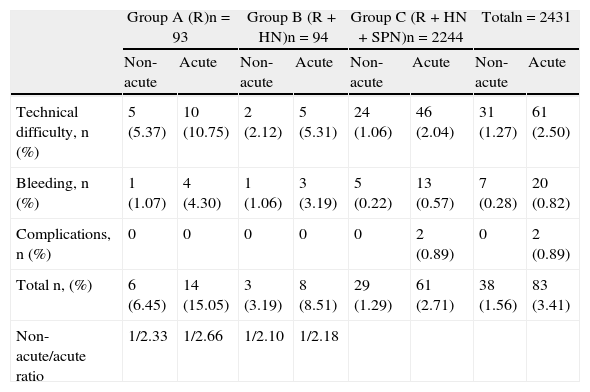
The conversion was similar for the 3 groups, reported in 1.56% for non-acute cholecystitis and 3.41% for acute, for a total of 4.97%. The non-acute/acute ratio for each group was: group A 1/2.3, group B 1/2.6 and group C 1/2.1 (Table 3).
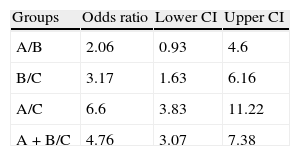
When we analyzed the feasibility and conversion results between groups, there was a significant difference of 67.13 and P<.001. The OR analysis between groups A, B and C are shown in Table 2, finding greater feasibility in group C with a high statistical significance (95% CI). Finally, the analysis of conversion type (TLC or OC) of the 3 groups did not reveal significant differences with CI below 95%, (OR A/B: 0.03302; B/C: 0.010; A/C: 0.0605; AB/C: 0.100).
Comparative Results of Odds Ratios and 95% Confidence Intervals With Regards to Feasibility and Conversion Among the 3 Patient Groups Treated.
| Groups | Odds ratio | Lower CI | Upper CI |
| A/B | 2.06 | 0.93 | 4.6 |
| B/C | 3.17 | 1.63 | 6.16 |
| A/C | 6.6 | 3.83 | 11.22 |
| A+B/C | 4.76 | 3.07 | 7.38 |
Group A using reins; group B using reins and hook-needle (R+HN); group C using reins, hook-needle and suture passing needles (R+HN+SPN).
Distribution of the Cause for Conversion by Groups, as well as by Non-acute or Acute Gallbladder Disease.
| Group A (R)n=93 | Group B (R+HN)n=94 | Group C (R+HN+SPN)n=2244 | Totaln=2431 | |||||
| Non-acute | Acute | Non-acute | Acute | Non-acute | Acute | Non-acute | Acute | |
| Technical difficulty, n (%) | 5 (5.37) | 10 (10.75) | 2 (2.12) | 5 (5.31) | 24 (1.06) | 46 (2.04) | 31 (1.27) | 61 (2.50) |
| Bleeding, n (%) | 1 (1.07) | 4 (4.30) | 1 (1.06) | 3 (3.19) | 5 (0.22) | 13 (0.57) | 7 (0.28) | 20 (0.82) |
| Complications, n (%) | 0 | 0 | 0 | 0 | 0 | 2 (0.89) | 0 | 2 (0.89) |
| Total n, (%) | 6 (6.45) | 14 (15.05) | 3 (3.19) | 8 (8.51) | 29 (1.29) | 61 (2.71) | 38 (1.56) | 83 (3.41) |
| Non-acute/acute ratio | 1/2.33 | 1/2.66 | 1/2.10 | 1/2.18 | ||||
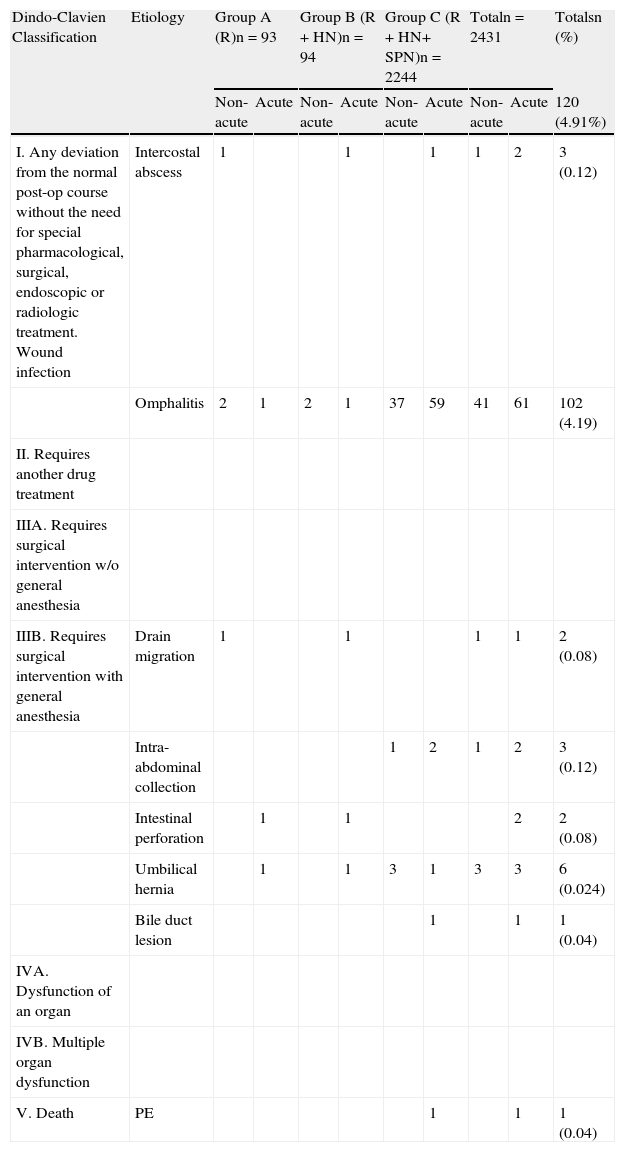
The complications according to the Dindo–Clavien classification30 are shown by groups in Table 4.
Dindo–Clavien Classification of the Complications in Groups A, B and C by Non-acute and Acute Gallbladder Disease.
| Dindo-Clavien Classification | Etiology | Group A (R)n=93 | Group B (R+HN)n=94 | Group C (R+HN+ SPN)n=2244 | Totaln=2431 | Totalsn (%) | ||||
| Non-acute | Acute | Non-acute | Acute | Non-acute | Acute | Non-acute | Acute | 120 (4.91%) | ||
| I. Any deviation from the normal post-op course without the need for special pharmacological, surgical, endoscopic or radiologic treatment. Wound infection | Intercostal abscess | 1 | 1 | 1 | 1 | 2 | 3 (0.12) | |||
| Omphalitis | 2 | 1 | 2 | 1 | 37 | 59 | 41 | 61 | 102 (4.19) | |
| II. Requires another drug treatment | ||||||||||
| IIIA. Requires surgical intervention w/o general anesthesia | ||||||||||
| IIIB. Requires surgical intervention with general anesthesia | Drain migration | 1 | 1 | 1 | 1 | 2 (0.08) | ||||
| Intra-abdominal collection | 1 | 2 | 1 | 2 | 3 (0.12) | |||||
| Intestinal perforation | 1 | 1 | 2 | 2 (0.08) | ||||||
| Umbilical hernia | 1 | 1 | 3 | 1 | 3 | 3 | 6 (0.024) | |||
| Bile duct lesion | 1 | 1 | 1 (0.04) | |||||||
| IVA. Dysfunction of an organ | ||||||||||
| IVB. Multiple organ dysfunction | ||||||||||
| V. Death | PE | 1 | 1 | 1 (0.04) | ||||||
It should be mentioned that the leakage of bile caused by the perforation of the gallbladder wall is limited by the prophylactic puncture and suction. When there is bile spilling, aspiration/lavage is used, although this is not considered a complication as there have been no secondary post-surgery collections or abscesses.
DiscussionThe increase in the percentage of feasibility of the SPLC technique when using PN has been confirmed in our experience. However, there is still much evidence to be corroborated in future research. The SPLC technique, unlike single-incision laparoscopic techniques with multi-valve platforms, is not assisted with other forceps. It is therefore comprehensible that, without the help of PN, its feasibility is 0%.
The substitution of assisting ports for PN was done gradually, responding to the need and demand that the technique presented. Currently, the skills that the experienced laparoscopic surgeons needs include: management of a laparoscope with a working channel, traction reins with percutaneous needles, handling of a hook needle and extracorporeal knots. During the courses given by the author, the learning curve takes an average of 36h of simulator practice and 5 supervised procedures.
The mechanism used by the PN elements for assistance in counter traction and triangulation are based on the traction of the walls of the organ for their manipulation. This is unlike the use of traditional laparoscopy clamps that compress the swollen tissue, which explains the greater feasibility even in acute gallbladder disease.
Additionally, the operative cost of the procedure is reduced indirectly and proportionally since the PN are economical compared with the ports and instruments of CT.
Operative time, hospital stay, analgesia required depending on the post-surgical pain and post-surgical complications of this SPLC technique, compared with other single-port techniques and TLC, make it a feasible, safe and attractive alternative with advantageous esthetic results.31–36
In the future, consideration could be given to combining this with other single-port techniques,23,24 with some type of multi-instrument port to avoid the conflict of many instruments in little space.22 The application of this technique should also be studied in laparoscopic procedures for appendectomies, inguinal hernia repair, hysterectomies, anti-reflux surgery, transvaginal cholecystectomies, transgastric cholecystectomies, etc.27,28,37
Conflict of InterestsThere is no conflict of interests related to the present study.
Please cite this article as: Dávila F, Tsin D, González G, Dávila MR, Lemus J, Dávila U. Utilidad de las agujas percutáneas en la factibilidad de la colecistectomía laparoscópica con un puerto. Cir Esp. 2014;92:261–268.
This paper was presented as an open paper during the 2nd International Congress of Digestive System Surgery, organized by the Mexican Association of Digestive Surgery (AMCAD) in the city of León (Guanajuato, Mexico) on July 29, 2012.