The radiological finding of free air in the abdominal cavity is generally considered a surgical emergency. It is associated with perforated abdominal viscus in more than 90% of cases.1–3 Nevertheless, the remaining 10% are not caused by perforation; these cases of non-surgical, asymptomatic, benign, idiopathic pneumoperitoneum are a diagnostic and therapeutic dilemma.2
We present the case of a 77-year-old woman with amyotrophic lateral sclerosis (ALS) who presented dysphagia and nocturnal hypoventilation, so she was admitted to the pneumology department for percutaneous endoscopic gastrostomy (PEG) and adaptation to non-invasive mechanical ventilation (NIMV).
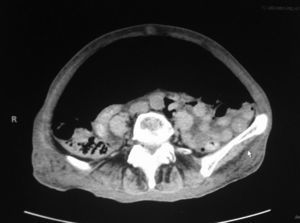
During PEG placement, we observed a superficial tear in the cardias with a small amount of self-limited bleeding. The general surgery department was called in 7 days later due to the appearance of pneumoperitoneum on a chest radiograph, accompanied by increased abdominal perimeter and pain. Given the clinical and hemodynamic stability of the patient, an abdominal CT scan was done to rule out complications. The scan showed abundant pneumoperitoneum that was displacing and compressing the abdominal viscera in the caudal direction. The gastrostomy catheter was well placed, and no free fluid was observed (Fig. 1). With the diagnostic suspicion of benign pneumoperitoneum, we decided upon non-surgical treatment. Because of the distension, abdominal pain and risk for compartment syndrome, percutaneous drainage of the pneumoperitoneum was carried out with an Abbocath in the left flank, leaving in a 8F pigtail catheter (Fig. 2). After a large amount of air was released, the distension disappeared and the patient reported an improvement in symptoms. The follow-up radiograph showed that the pneumoperitoneum was largely reduced.
The patient currently remains asymptomatic, with NIMV and enteral nutrition through the gastrostomy. The PEG is kept open during NIMV and abdominal drainage is continuous.
The most frequent cause of pneumoperitoneum is previous surgery due to the postoperative retention of air, which is usually resolved during the first week after surgery.4–6 Benign pneumoperitoneum can be classified according to the source of the air, the most frequent of which is the thoracic cavity, followed by the gastrointestinal tract and the female genital apparatus.4,5
Mechanical ventilation is the most frequent thoracic cause of pneumoperitoneum due to the increased intra- and extra-alveolar pressure.4–7 The passage of air from the thorax to the abdomen is explained by the presence of anatomical orifices or porous diaphragm syndrome,2,8 which usually occur in areas of weakness, such as the posterolateral and parasternal regions.9 Risk factors include high pressure in the respiratory tract, high tidal volumes, unexpandable lung, preexisting pulmonary disease and respiratory distress syndrome.9 In our case, mechanical ventilation with positive pressure at the end of expiration increases intrathoracic pressure and the risk for dissection of the peritoneal cavity.4–8
Pneumoperitoneum is also associated with gastrointestinal endoscopic processes: after polypectomy with electrocautery,10 microperforations, air dissection through the lymph nodes or submucosal channels into the peritoneal cavity, and air filtration through the thin, intact walls of the intestine, with no perforation.9 Instrumental perforations represent between 0.1 and 1% of diagnostic explorations and 3% of therapeutic procedures.10
The incidence of pneumoperitoneum after the placement of a percutaneous gastrostomy is approximately 25%. The cause is usually the insufflation of high-pressure air in the gastric chamber, associated with microperforations.9 In our case, the placement of the gastrostomy but, above all, the lesion in the cardias seems to be the origin of the pneumoperitoneum, which increased due to the NIMV.
Cystic pneumatosis of the colon would be the most frequent cause of non-surgical pneumoperitoneum if we excluded the causes related with therapeutic procedures.2–9 In 30% of cases, the presentation of pneumoperitoneum is spontaneous. Its benign etiology makes for a positive prognosis and the treatment of choice is conservative.
Other more anecdotal causes of pneumoperitoneum are gynecological. These occur when the air passes into the abdominal cavity through the vagina and the Fallopian tubes.2
In our case, the cause of the pneumoperitoneum was the adaptation to NIMV associated with the placement of a gastrostomy and the lesion of the cardias. Given the hemodynamic stability of the patient and because CT scans had not detected any complications, a conservative approach was the most appropriate. Bedside abdominal decompression was necessary to avoid compartment syndrome.9
We can conclude that, when given the presence of pneumoperitoneum, a suspected perforated abdominal viscus is the first diagnosis and, therefore, urgent laparotomy should be done. Nevertheless, in selected cases where the pathologic/medical history, physical examination and complementary techniques do not suggest peritonitis, non-surgical management with close patient monitoring can be considered.2 Within the conservative treatment for this type of cases, percutaneous drainage should be assessed in order to avoid compartment syndrome.
Conflict of InterestNone.
Please cite this article as: Gutiérrez Andreu M, Yuste García P, Gómez Rodríguez P, de la Cruz Vigo F. Tratamiento conservador «in situ» del neumoperitoneo. Cir Esp. 2015;93:127–129.