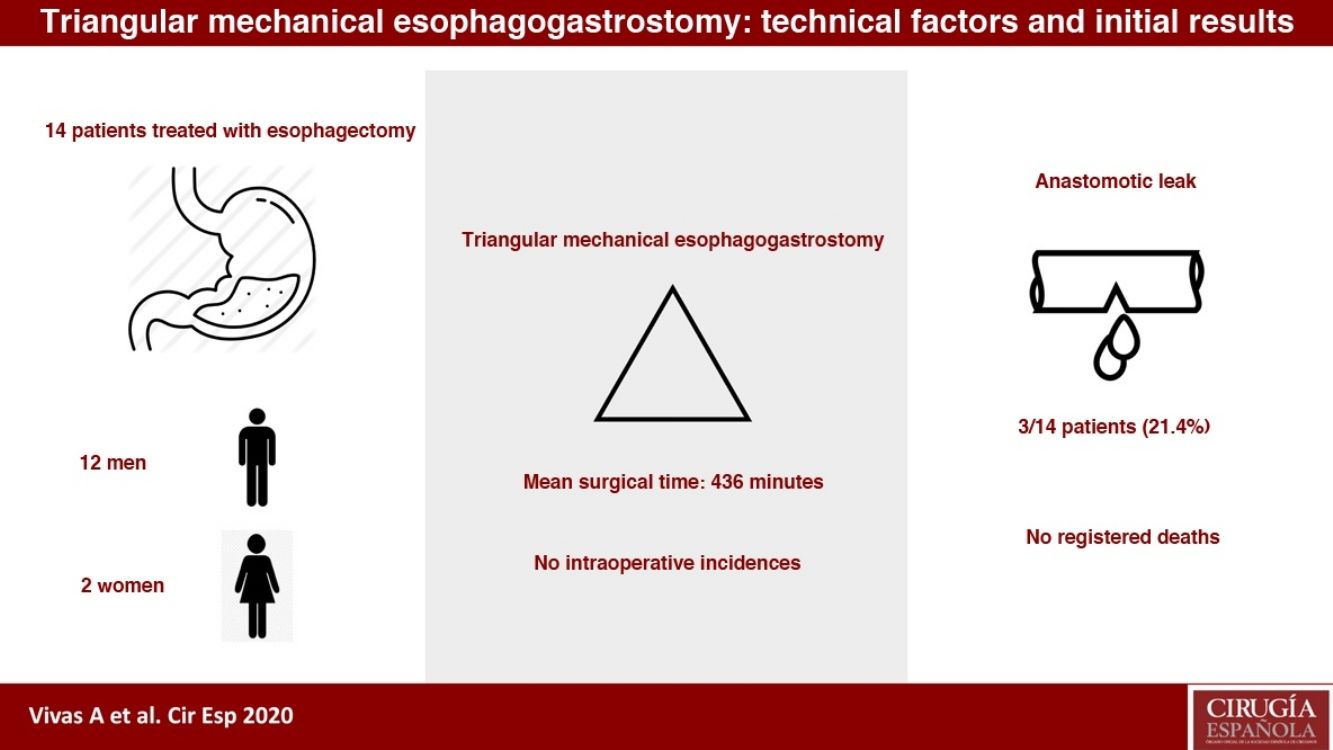
Esophageal cancer represents the eighth neoplasm worldwide. The therapeutic approach is interdisciplinary, with surgery being the most effective option. Several techniques have been proposed to perform esophagogastrostomy after esophagectomy, among them mechanical triangular esophagogastrostomy (MT), with a little experience published in the Western literature on the latter. The objective of this study is to describe the technical aspects and initial results of MT anastomosis.
MethodsA retrospective review of the patients who underwent esophagectomy according to the McKeown technique was performed, those in which MT anastomosis was implemented, between October 2017 and March 2020 in our hospital.
Results14 patients were included, with a mean age of 63 years. The mean operative time was 436 min (360–581), being diagnosed of anastomotic leak (AL) 3 of the 14 patients (21.4%), as well as 3 patients presented anastomotic stenosis (AS). The median stay was 20 days, without any death in the series.
DiscussionMultiple publications suggest the superiority in terms of AL and AS of the mechanical triangular anastomosis, which was also observed in our series, in which despite the small sample, a rapid improvement was observed in the indicators after the first cases. Therefore, this type of anastomosis may be a safe option for performing esophagogastric anastomosis after esophagectomy, being necessary more definitive conclusive studies.
El cáncer de esófago representa la octava neoplasia a nivel mundial. El abordaje terapéutico es interdisciplinar, siendo la cirugía la opción más eficaz. Se han planteado varias técnicas para la realización de la esofagogastrostomía posterior a la esofagectomía, entre ellas la esofagogastrostomía triangular mecánica (TM), con muy poca experiencia publicada en la literatura occidental. El objetivo de este estudio es describir los aspectos técnicos y resultados iniciales de la instauración de anastomosis triangular mecánica.
MétodosSe realizo una revisión retrospectiva de los pacientes sometidos a esofaguectomía según técnica de McKeown, en los cuales se realizó anastomosis TM, entre octubre de 2017 y marzo de 2020 en nuestro hospital.
ResultadosFueron incluidos 14 pacientes, con una media de edad de 63 años. El tiempo operatorio promedio fue de 436 minutos (360–581), siendo diagnosticados de fuga anastomótica (FA) 3 de los 14 pacientes (21,4), así como también 3 pacientes presentaron estenosis anastomótica (EA). La mediana de estancia fue de 20 días, sin ningún exitus en la serie.
DiscusiónMúltiples publicaciones sugieren la superioridad en términos de FA y EA de la anastomosis triangular mecánica (TM), observándose esto también en nuestra serie, en la cual a pesar de lo reducido de la muestra, se observó una rápida mejoría en los indicadores posterior a los primeros casos, por lo que este tipo de anastomosis puede ser una opción segura para la confección de la anastomosis esofagogástrica posterior a la esofaguectomía, siendo necesarios más estudios conclusiones definitivas.
Esophageal cancer ranks as the 8th most frequent cancer in the world and mainly affects men (male-to-female ratio 10:3). Alcohol and tobacco are the most widely documented risk factors, although there are many others, including gastroesophageal reflux disease. The prognosis is unfavorable, with a 5-year survival rate of 15%–25%. Due to its aggressiveness and capacity for locoregional invasion, esophageal cancer is also the 6th leading cause of oncological mortality1,2.
The therapeutic approach is interdisciplinary: endoscopy, chemotherapy, radiotherapy and surgery, the latter of which is the most effective option. Surgical treatment is not exempt from complications, the most feared of which is anastomotic leak (AL), which occurs in some 10%–30% of patients3. AL prolongs hospital stay, increases perioperative morbidity, and has a mortality rate between 20% and 35%4,5. Its risk factors include the surgical technique, tumor location, patient nutritional status, etc.6. Several techniques have been proposed for performing esophagogastrostomy, both mechanical (linear, circular and triangular) and manual, which have been compared in several meta-analyses with no statistically significant differences7,8. In the Western literature, experience with the use of triangular mechanical (TM) cervical esophagogastrostomy is very limited. It is in east Asian literature where we find the largest number of publications about this technique. Several of these publications have indicated that mechanical anastomosis has a lower rate of anastomotic dehiscence and anastomotic stricture (AS), without having conclusively demonstrated these differences9 and, within mechanical anastomoses, TM anastomosis has been associated with a lower incidence of postoperative complications10,11. The objective of this study is to describe the technical factors and the initial results of the establishment of TM anastomosis as an option for esophagogastrostomy.
Material and methodsAll patients in the series underwent esophagectomy following the McKeown technique (surgery in 3 stages: thoracoscopic, laparoscopic and open cervical approach), with TM esophagogastrostomy. All of them were operated on by expert esophagogastric surgeons. Diagnosis was made by upper gastrointestinal endoscopy and pathological confirmation as well as staging thoracic-abdominal-pelvic CT scan.
In all cases, esophagectomy was performed according to the McKeown technique, by means of thoracoscopy, laparoscopy and cervical incision with tubulized gastric pull-up (Akiyama technique12) and cervical TM esophagogastrostomy.
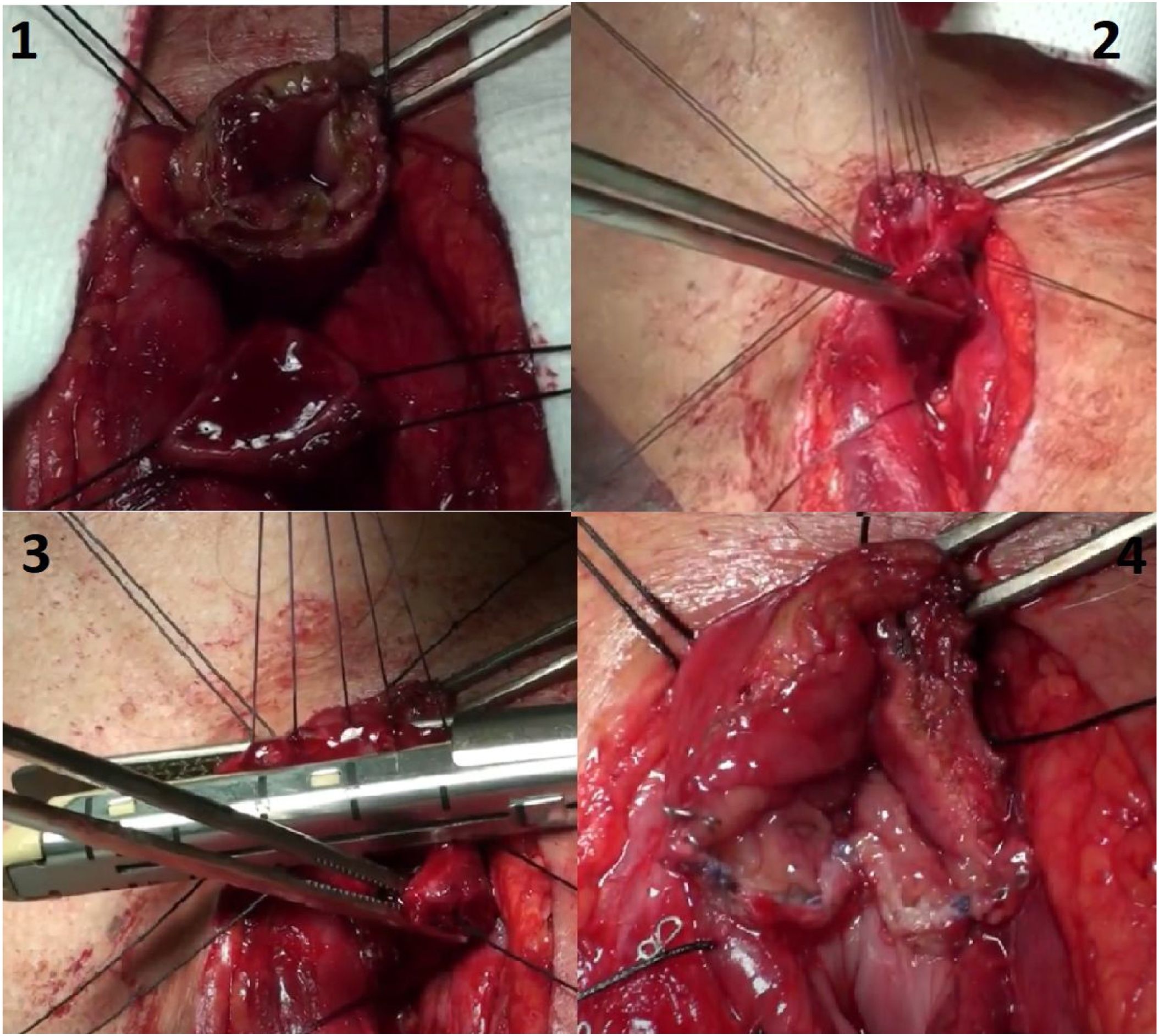
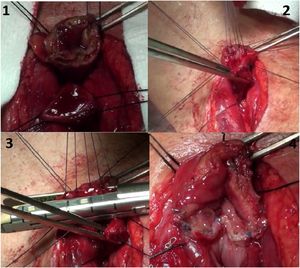
In the first step, using a thoracoscopy with the patient in left lateral decubitus, mediastinal lymphadenectomy and esophageal mobilization were performed. Afterwards, the patient was placed in the supine position, and gastric dissection was performed laparoscopically to prepare the gastric tube. Finally, through left lateral cervicotomy, an end-to-end TM esophagogastric anastomosis was created between the cervical esophageal remnant and gastroplasty that had been pulled up. For this anastomosis, the circumference is divided into 3 sides: posterior, anteromedial and anterolateral. The posterior side is made first, initially with 5 traction points for symmetrical traction, and then it is divided and stapled with a 60 mm endo-stapler (Endo-GIA60-3 mm; Covidien®) (Fig. 1). The same action is then repeated on the anterolateral and anteromedial sides, thereby performing the same action on the remaining 2 sides of the triangle. Subsequently, the anastomosis is checked for leaks, and a nasogastric tube is left in place.
We analyzed all patients treated at our hospital with esophagectomy in whom TM anastomosis was performed between October 2017 and March 2020. We recorded patient demographic variables, such as age and sex, as well as clinical variables, including tumor staging (TNM), date of surgery and the use of neoadjuvant therapy (chemotherapy or radiotherapy). The diagnosis of anastomotic leak was defined by the development of compatible symptoms in the postoperative period, confirmed by radiological or endoscopic tests, and then classified according to the Esophagectomy Complications Consensus Group (ECCG)13. Finally, the diagnosis of anastomotic stenosis was established by the appearance of symptoms and confirmed by endoscopy as well as the need for specific treatment after diagnosis.
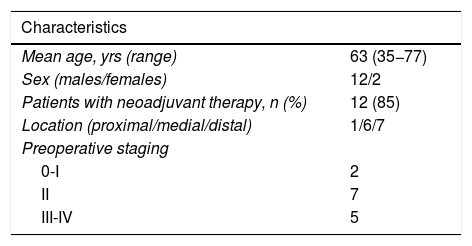
ResultsFourteen patients were included in the study (12 men, 2 women; mean age 63 years), 13 of whom had been diagnosed with esophageal adenocarcinoma and one with total occlusion due to a benign cause. Neoadjuvant treatment was administered in 12 patients. The distal third was the most frequent site of presentation (7 patients). Patient clinical characteristics are shown in Table 1.
Preoperative clinical characteristics of patients treated with esophagectomy with TM esophagogastrostomy.
| Characteristics | |
|---|---|
| Mean age, yrs (range) | 63 (35−77) |
| Sex (males/females) | 12/2 |
| Patients with neoadjuvant therapy, n (%) | 12 (85) |
| Location (proximal/medial/distal) | 1/6/7 |
| Preoperative staging | |
| 0-I | 2 |
| II | 7 |
| III-IV | 5 |
The average operative time was 436 min (360–581). There were no immediate complications in any of the patients during their stay in the post-anesthesia recovery unit. Anastomotic dehiscence was diagnosed in 3 out of the 14 patients: 2 with ECCG type II AL, and one ECCG type III. Two of these 3 AL occurred in the first 7 patients of the series. Reoperation was required in 3 patients, only one due to anastomotic dehiscence; in the remaining 2 patients, the causes were pyloric stenosis and colon hernia through the esophageal hiatus. Median hospital stay was 20 days, with a mean of 25.4 days (9–69). No deaths occurred in the series.
Two of the patients who presented AL were treated with negative pressure therapy (Endo-SPONGE®, B. Braun), with good evolution. Anastomotic stenosis developed in 3 out of the 14 cases, 2 of which were in patients with postoperative AL and were managed favorably with endoscopic dilation.
DiscussionDespite progress in techniques and therapeutic resources, the surgical treatment of esophageal cancer remains complex14. This complexity translates into multiple techniques for esophageal resection, and, at the same time, various reconstructive options are available. These options largely depend on the segment of the digestive tract with which the esophagus is reconstructed (commonly the stomach, colon, or small intestine), the location of the anastomosis (cervical or thoracic) and the anastomotic technique (manual or mechanical). The technique is one of the variables that most affects morbidity and postoperative progress15.
In the case of cervical anastomoses, the AL rate of the anastomosis between the esophageal remnant and the gastric pull-up is higher than intrathoracic anastomoses (Ivor Lewis)16. Multiple studies have compared the rate of anastomotic complications of manual versus mechanical anastomoses. The review by Kim and Takabe17 stands out, in which several non-randomized studies described a lower rate of AL in mechanical anastomoses. However, none of the randomized controlled trials reported statistically significant differences in AL rates.
When comparing mechanical anastomoses, several publications suggest that TM anastomosis is superior to circular mechanical and manual anastomoses in terms of AL and AS rates18. Toh et al.9 compared the results of triangular stapling and manual anastomosis and concluded that the triangular stapling technique reduces the frequency of anastomotic complications, including benign strictures or leaks. In addition, Furukawa et al.15 compared manual anastomoses, circular stapling and TM, and the AL rate with the triangular anastomosis was 8.3%, similar to the Takemura et al. rate19. In our series, triangular anastomosis was performed with the same technique used by Toh et al: on the posterior side with inversion of both ends, and on the medial and lateral sides with everted edges. We obtained an AL rate higher than that of other larger series, but in a much smaller group of patients, which was influenced by the characteristics of our environment. We also found differences with these series regarding the prior morbidity of the patients and a much higher proportion of neoadjuvant treatment: all of these are risk factors for the development of AL. Likewise, they were the first cases approached with the TM anastomosis technique, and 2 of the 3 cases that developed AL were among the first patients of the series. The incidence later decreased as the learning curve progressed. All complications were treated satisfactorily, with no mortality associated with esophagectomy in the 14 patients in the group.
AS, with subsequent dysphagia after esophagectomy, is a complication that greatly affects quality of life after surgery20. Ischemia of the pull-up segment and the type of anastomotic technique are the main risk factors for developing AS21. Worrell et al.22 analyzed the complications between mechanical and manual anastomoses: the incidence of AS was 38% in manual anastomoses compared to 26% in mechanical anastomoses, and AL was found to be a predictor for the development of AS. In addition, the study by Furukawa et al.15 observed that the incidence of AS was 8.3% in the TM anastomosis, which is lower than observed in the other anastomotic techniques. In our series, AS was observed in 21.4% of the patients, mainly in the first patients of the series and related with the previous appearance of anastomotic leak, which showed good response to endoscopic treatment.
Other studies, such as the Hayata et al. article23, have compared the incidence of AL and AS between circular mechanical anastomosis and TM anastomosis. Similar rates of postoperative stenosis were found in both groups (17% and 19%, respectively), but the incidence of AL was much lower in the TM anastomosis group (2% versus 11%), a result that was not statistically significant.
As the literature shows (mainly from hospitals in the eastern hemisphere), the TM esophagogastrostomy technique may be associated with a lower frequency of anastomotic complications, although solid conclusions have not been reached. Despite the small sample size of our series, the postoperative results were favorable, as a rapid improvement was observed in the indicators after the first cases in which this technique was used. Thus, this type of anastomosis can be considered a valid and safe option for creating the cervical esophagogastric anastomosis after esophagectomy. It should be noted that further studies are needed with higher methodological quality, some of which are underway24, in order to provide more definitive results.
Conflict of interestsThe authors have no financial, personal, or professional conflicts of interests to declare.
Please cite this article as: Vivas López A, Rodríguez Cuellar E, García Picazo A, Narváez Chávez C, Gómez Rodríguez P, Ortiz Aguilar M, et al. Esofagogastrostomía triangular mecánica: aspectos técnicos y resultados iniciales. Cir Esp. 2022;100:230–234.