Advanced laparoscopic surgery requires supplementary training outside the operating room. Clinical simulation with animal models or cadavers facilitates this learning.
ObjectiveWe measured the impact on clinical practice of a laparoscopic colorectal resection training programme based on surgical simulation.
Materials and methodsBetween March 2007 and March 2012, 163 surgeons participated in 30 courses that lasted 4 days, of 35h (18h in the operating room, 12h in animal models, and 4h in seminars). In May 2012, participants were asked via an on-line survey about the degree of implementation of the techniques in their day-to-day work.
ResultsSeventy surgeons (47%) from 60 different hospitals answered the survey. Average time elapsed after the course was 11.5 months (2–60 months). A total of 75% initiated or increased the number of surgeries performed after the training. The increase in practice was >10 cases/month in 19%, and <5 cases/month in 56% of surgeons. Thirty-eight percent of participants initiated this surgical approach.
ConclusionsSeventy-five percent of the surveyed surgeons increased the clinical implementation of a complicated surgical technique, such as laparoscopic colorectal surgery, after attending a training course based on clinical simulation.
La cirugía laparoscópica avanzada necesita complementar el aprendizaje fuera del quirófano. La simulación clínica con animales o cadáveres favorece este aprendizaje.
ObjetivoMostrar el grado de impacto en la práctica quirúrgica diaria en los cirujanos que realizaron un curso clínico-experimental de cirugía colorrectal laparoscópica.
Material y métodoEntre marzo de 2007 y marzo de 2012, realizamos 30 cursos de 4 días de duración, durante 35h (18 en quirófano, 12 en animales de experimentación y 4 en seminarios), en los que participaron 163 cirujanos. En mayo de 2012, vía online, se les remitió una encuesta con la finalidad de evaluar el impacto que este curso podía haber tenido en su práctica diaria de cirugía colorrectal laparoscópica.
ResultadosEl número de encuestas contestadas fue de 70 (47%), que correspondían a cirujanos de 60 hospitales diferentes. El periodo medio tras el curso fue de 11,5 meses (2–60). El 75% de los cirujanos iniciaron o aumentaron el número de cirugías que realizan después del curso, siendo este aumento menor de 5 casos/mes en el 56% y mayor de 10 casos/mes en el 19%. El 38% iniciaron esta vía de abordaje.
ConclusionesEl 75% de los cirujanos encuestados aumentaron la implementación clínica de una técnica quirúrgica compleja como es la cirugía colorrectal por vía laparoscópica, después de realizar un curso de entrenamiento apoyado en simulación clínica.
In recent years surgical simulation has been increasingly used in Spain in general surgical training as a learning tool to complement the traditional methods as it meets many of the needs arising in today's healthcare context.1,2
There are several factors which make surgical simulation widely accepted from the point of view of surgical technique: it promotes the integration of complex surgical knowledge and skills3; it improves the efficiency of movements, reduces the number of errors and the time taken to complete a task; it increases the extent to which learning is retained when compared with traditional teaching methods; it speeds up the learning curve; surgical skills are transferred to the care environment and it has been associated with reduced complications in patients.4
At present, most surgical teaching still involves learning from other more experienced surgeons acting as mentors. This training can be complemented using courses showing experts performing surgery on patients.5 However, a growing number of publications describe the use of virtual reality simulation models,6 on animals or cadavers,7 as a valid training model for laparoscopic surgery. One determining factor in the choice of a particular training technique is its effect on the clinical implementation of new procedures. However, the publications which describe the training models seldom reflect the extent to which the different learning models are being implemented clinically.8
The objective of this publication is to verify that the surgeons undertaking training programmes based on surgical simulation of laparoscopic colorectal surgery are increasing the rate at which this surgical technique is being implemented in their patients.
Materials and MethodsWe present an observational and longitudinal study undertaken from March 2007 to March 2012, the object of which was to analyse the clinical impact that 30 training programmes might have had for 163 surgeons. The programmes were based on surgical simulation of laparoscopic colorectal surgery performed in the Valdecilla University Hospital and in the experimental facilities of the Valdecilla virtual hospital.
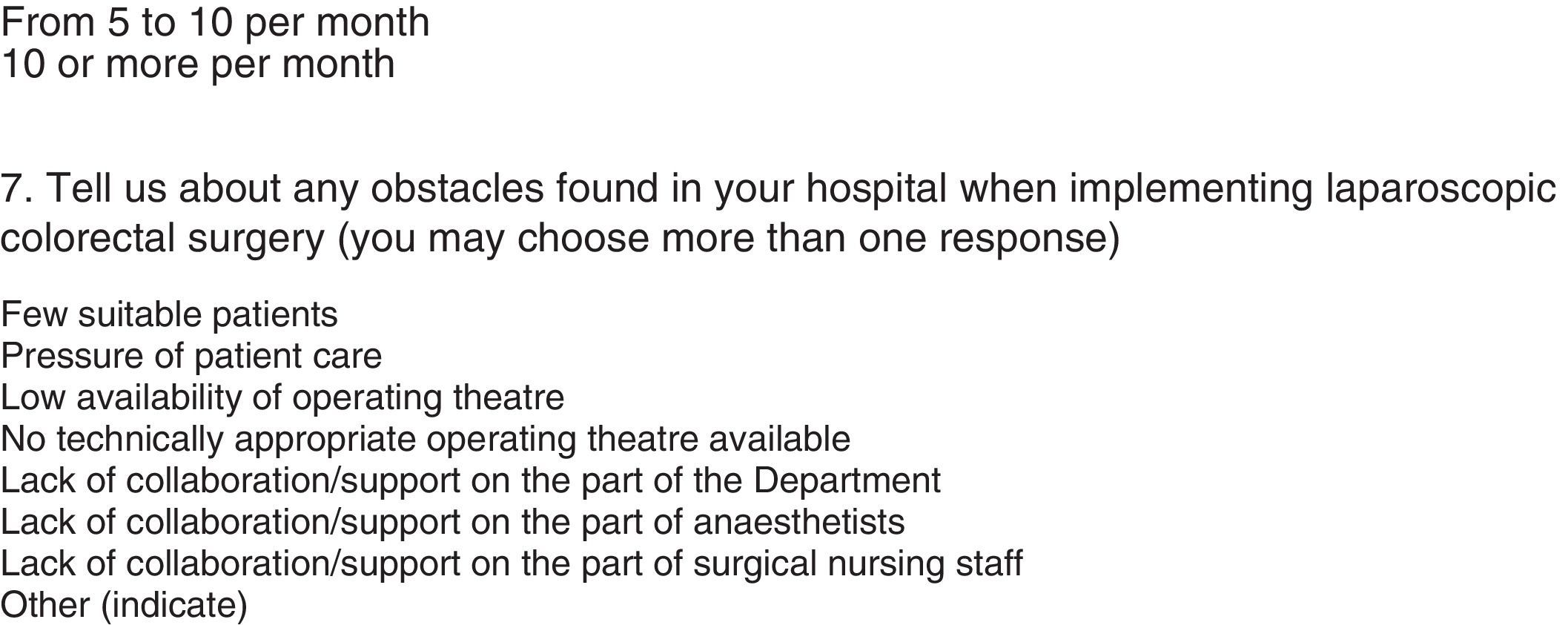
These surgeons, from 86 different hospitals, were sent an on-line survey to measure the degree of impact on clinical practice of these techniques in their hospitals of origin after the course and to assess any difficulties. The questions they were asked included: their individual experience in laparoscopic colorectal surgery prior to the course; the number of colectomies in their department and the amount performed by laparoscopy; the extent of clinical implementation after the course expressed in number of cases/month; obstacles or difficulties in implementation (Appendix A).
The design of the course (35h over 4 days) was divided into 3 parts with different content. The first involved 3 surgical sessions with 5 patients where an expert surgeon performed the laparoscopic surgical technique. After each intervention, the stages of the basic techniques were deconstructed and the expert analysed each with the course participants.
The second stage involved experimental operating theatres, over 3 days of 4h each. On the first day the trainees performed intestinal anastomoses on pig entrails ex vivo, using an endotrainer, on an individual basis. Over the next 2 days, left and right colectomies were performed on live animals following the stages shown during the surgery on the patient. At the end of each of these sessions, a debriefing took place in order to think through and analyse the technical stages performed during each procedure.
The third stage was developed during the last day, and lasted 5h, when the instructors and the trainees examined the action protocols pre- and post-surgery and the surgical details dealt with during the clinical sessions which were backed up with videos. The objective of all of this was to prepare an action protocol which could later be implemented in their hospitals.
The trainees were monitored by the same surgeons that had operated on the patients, both during the endotrainer training and during the colon resections performed on animals; so that each instructor worked with 2 trainees. Likewise, during the practice session a direct, objective, structured and scaled assessment was made reflecting times, the quality parameters of the anastomoses and the key technical stages in the colectomies performed.
All the course participants were given a survey to assess the course when it ended. After completion of the course, a further survey was sent to them by e-mail for follow-up of their activity and to gather data in real time.
The statistical analysis consisted of the description of the categorical variables by the distribution of frequencies and percentages of each category. When the surveys were compared during and after the training, the Chi-square test was used to assess possible association. The recommended Wilson method was used to calculate the confidence interval of a proportion.
The analysis was made using the R9 programme and P<.05 was considered statistically significant.
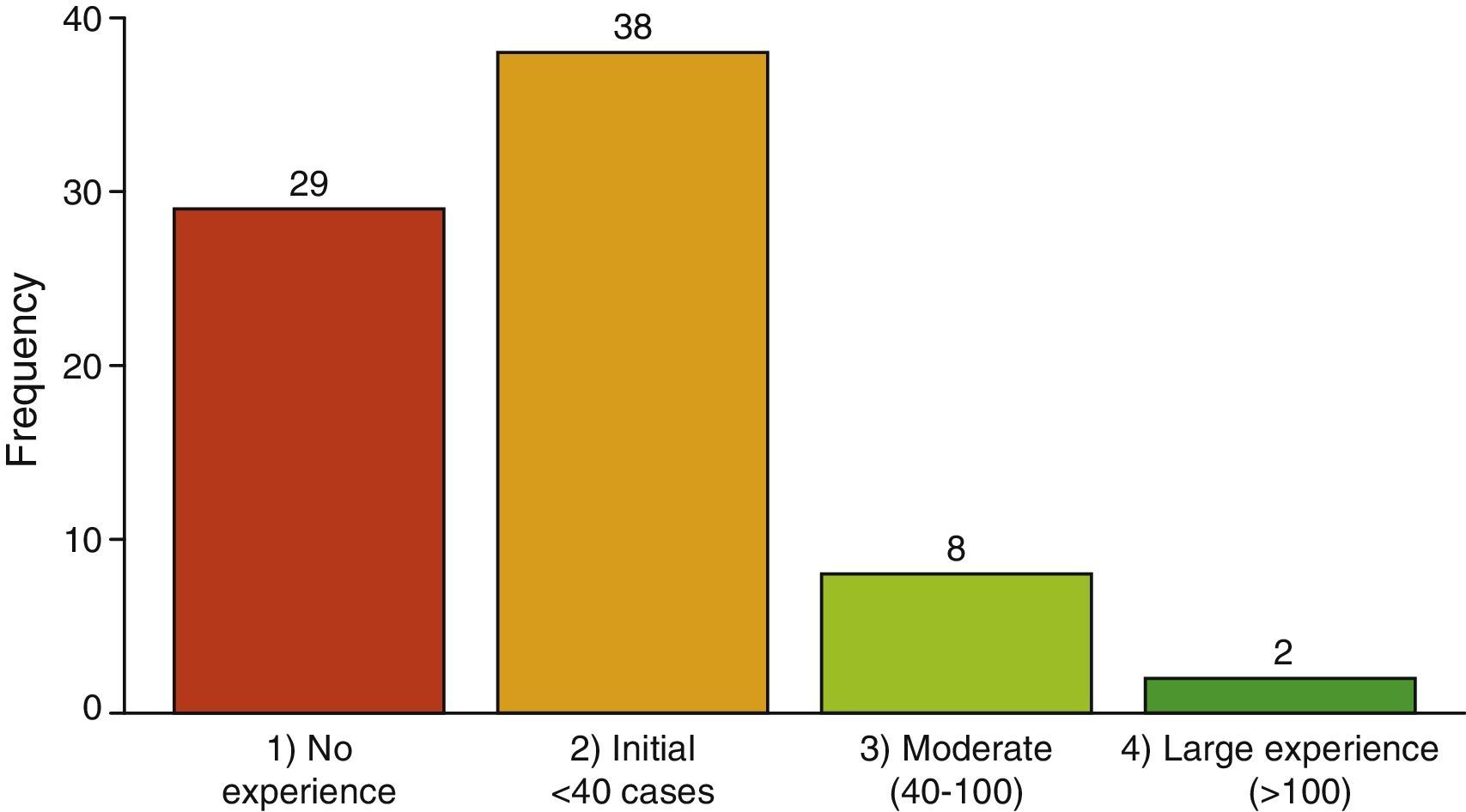
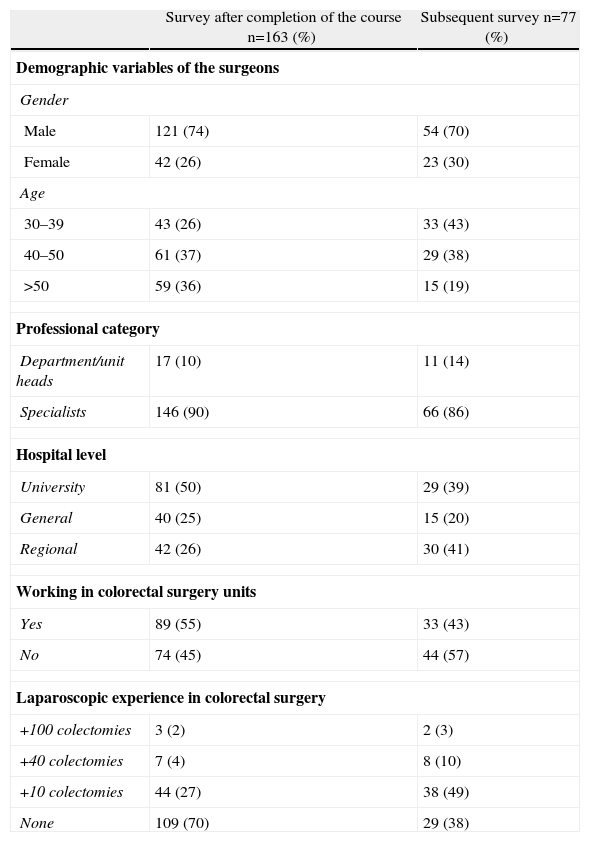
ResultsThe survey was sent to 163 surgeons, 77 responses were received from 60 different hospitals. They were distributed per year of running the course as shown in Fig. 1. The general characteristics of the respondents and the comparison of the data between received surveys and those obtained during the running of the course are shown in Table 1. When the demographic variables of the surgeons, their working environment and their surgical activity are compared before and after surgery, it can be observed that 47% answered surveys is a representative sample which does not significantly differ from the sample prior to the course. It is worth noting that most of the surgeons who responded were under 40 years of age and those with prior experience in colorectal laparoscopy with a significant difference (χ2=7.83; P=.020).
General Characteristics of the Population Surveyed.
| Survey after completion of the course n=163 (%) | Subsequent survey n=77 (%) | |
| Demographic variables of the surgeons | ||
| Gender | ||
| Male | 121 (74) | 54 (70) |
| Female | 42 (26) | 23 (30) |
| Age | ||
| 30–39 | 43 (26) | 33 (43) |
| 40–50 | 61 (37) | 29 (38) |
| >50 | 59 (36) | 15 (19) |
| Professional category | ||
| Department/unit heads | 17 (10) | 11 (14) |
| Specialists | 146 (90) | 66 (86) |
| Hospital level | ||
| University | 81 (50) | 29 (39) |
| General | 40 (25) | 15 (20) |
| Regional | 42 (26) | 30 (41) |
| Working in colorectal surgery units | ||
| Yes | 89 (55) | 33 (43) |
| No | 74 (45) | 44 (57) |
| Laparoscopic experience in colorectal surgery | ||
| +100 colectomies | 3 (2) | 2 (3) |
| +40 colectomies | 7 (4) | 8 (10) |
| +10 colectomies | 44 (27) | 38 (49) |
| None | 109 (70) | 29 (38) |
One hundred and twenty-two of the respondents surveyed had attended other laparoscopic training courses, an average of 2 per surgeon, 55 of them could be considered advanced laparoscopic surgery training courses.
The previous experience of the trainees in basic laparoscopic surgery techniques (appendectomy, cholecystectomy, anti-reflux techniques) was an average of 194 procedures/surgeon.
Thirty-three percent of surgeons were performing laparoscopic colorectal surgery prior to the course and 6% of them had performed more than 40 colectomies.
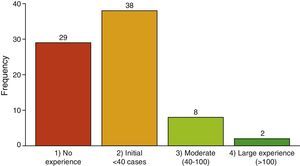
Forty-three percent (95% CI: from 32% to 54%) of the survey respondents were from hospitals with colorectal surgery units. Moreover, 38% (95% CI: from 28% to 49%) of them had no previous experience in this type of laparoscopic surgery. Only 3% (95% CI: from 1% to 9%) of the survey respondents had a large experience (more than 100 laparoscopic colectomies/year). If this experience is broken down into hospital experience, it can be observed that 56% of the surgeons from a first-level hospital had no experience compared to 26% of surgeons from third-level hospitals.
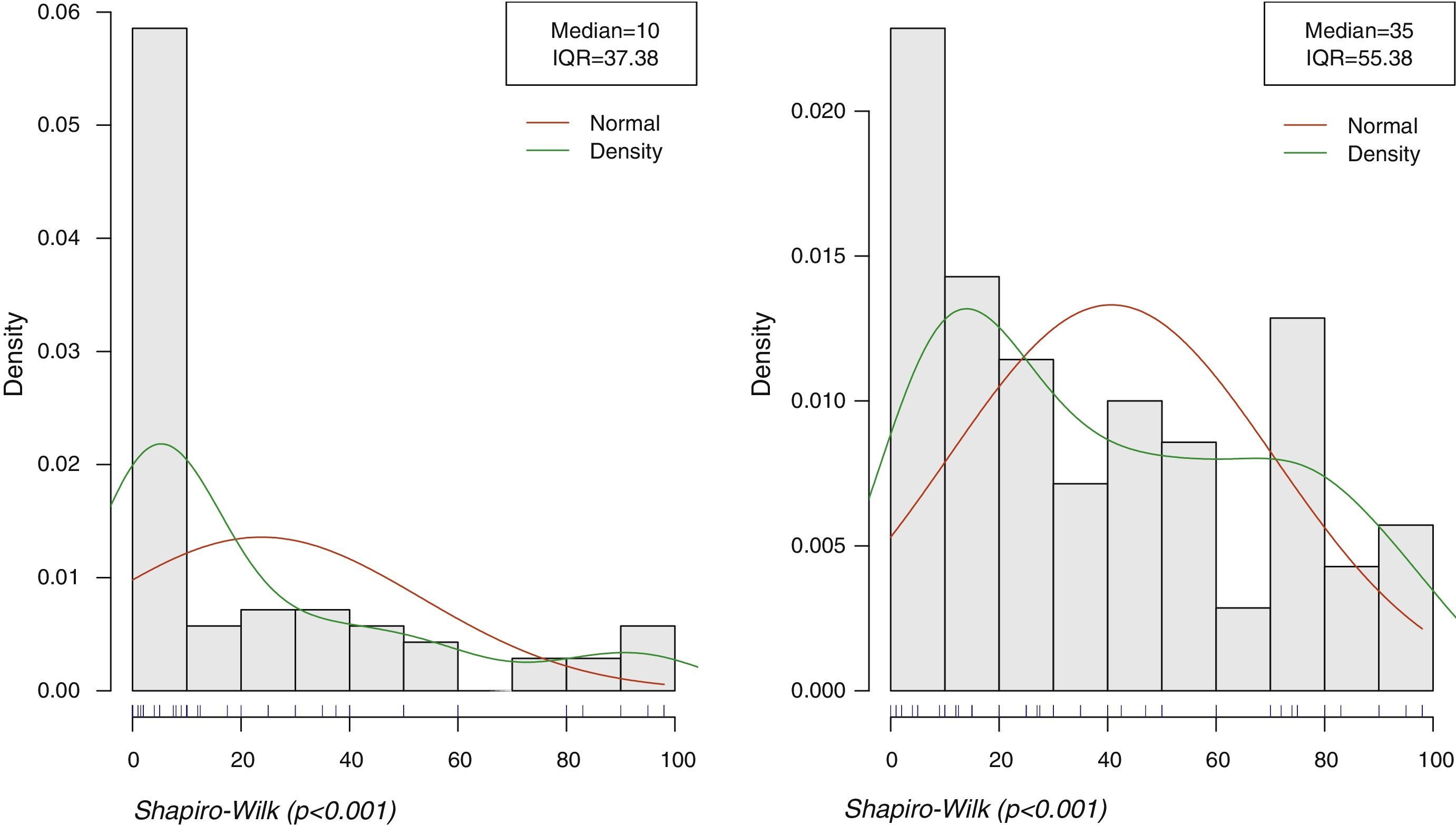
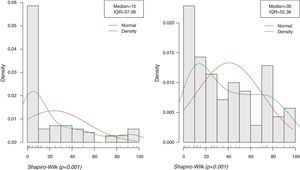
The main objective of this study is to analyse the extent to which the surgical technique taught during the course was implemented in the surgeon's daily clinical practice; therefore they were asked about the percentage of colon laparoscopic procedures before and after the training course, in their hospitals of origin. The left-hand graph in Fig. 2 shows the percentage of laparoscopic colectomies performed prior to the course (n=70, median=35%, IQR=5.38%); in other words, there is an obvious improvement of 25% (increasing from 10% to 35%).
Distribution of the percentages of laparoscopic colorectal surgery. Axis of abscissas: percentage of colectomies performed by laparoscopy/year. Axis of ordinates: number of respondents. The percentages prior to training are shown on the left-hand graph which follow a very asymmetric distribution with median=10% (IQR=37.4). The right-hand graph shows the percentages after a post-training period, and its distribution is also asymmetric with median=35% (IQR=55.4). The Shapiro–Wilk test, as it is significant, indicates that this is not a normal distribution.
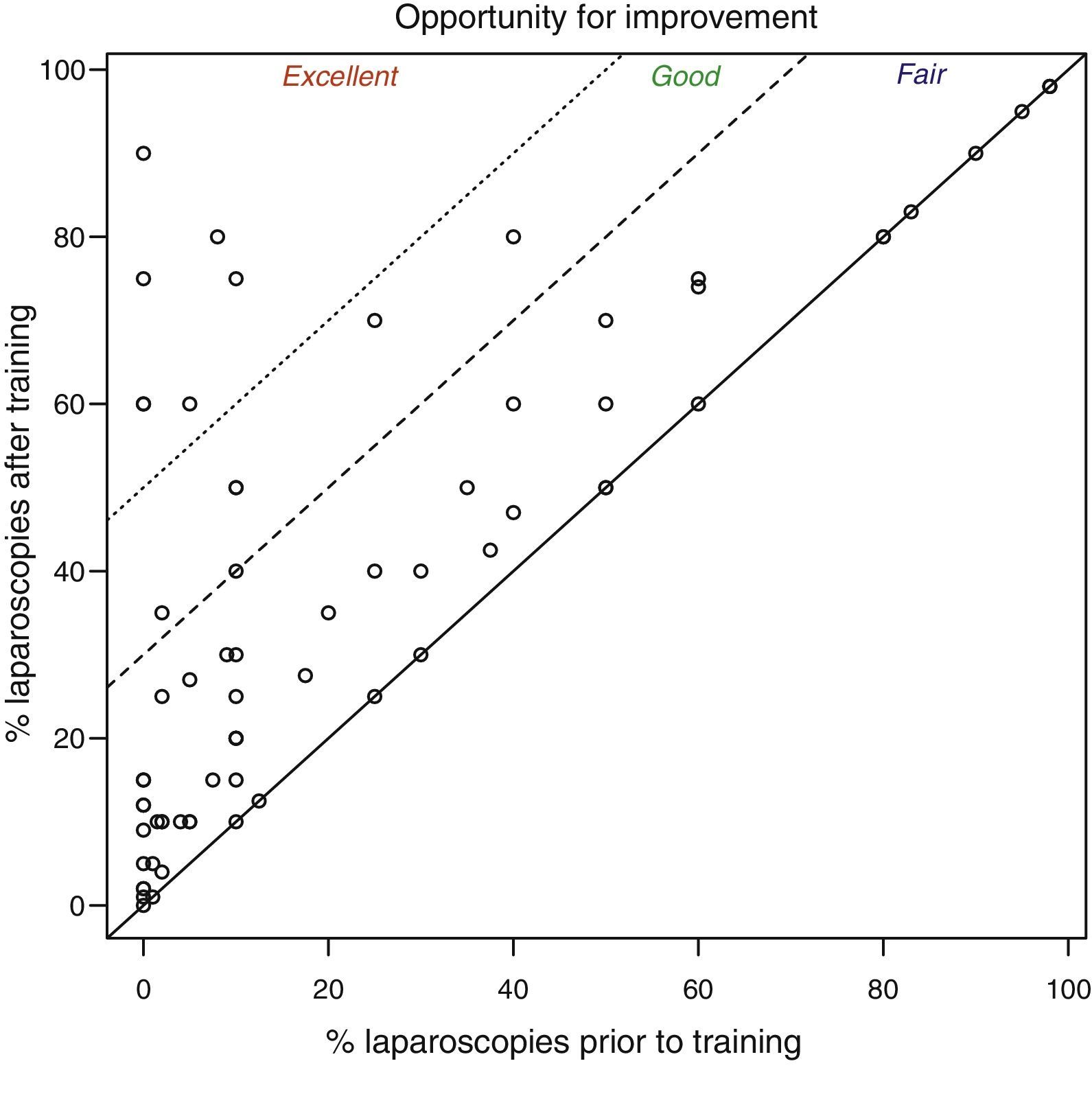
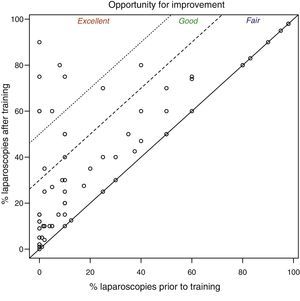
The degree of improvement was studied in the respondent group who improved and to that end, the percentage of laparoscopic colorectal operations they performed before the training are shown on the axis of abscissas and those performed after the training on the axis of ordinates. The points on the diagonal represent trainees for whom no change was observed. The points above the diagonal indicate an improvement (an increase of laparoscopic interventions after training) and the points below it indicate a decrease. Fig. 3 shows this information and it can be observed that a few trainees fall on to the diagonal, i.e., their surgical practice does not change at all after undertaking the course. There is a group of 39 surgeons, 57% (95% CI: from 45% to 68%) whose practice improved (between 1% and 25%). Six surgeons, 9% (95% CI: from 4% to 18%) showed good improvement (between 26% and 50%). Seven trainees showed an excellent improvement (more than 50%) 10% (95% CI: from 5% to 20%).
If this positive change, which is known as “opportunity for improvement”, is associated with the level of the hospital in which the respondents worked it can be observed that the small group of surgeons who showed an excellent improvement worked in a regional hospital and those whose improvement was good worked in a university or third level hospital.
The overall rating of the course as it was undertaken was 4.3 out of 5; the score for the experimental sessions was 4.8 and communication from and with the trainers 4.6. Out of the 77 trainees who responded, 49 awarded the maximum score (64%; 95% CI: from 53% to 74%), regardless of their position in the hospital (χ2=2.41, P=.492).
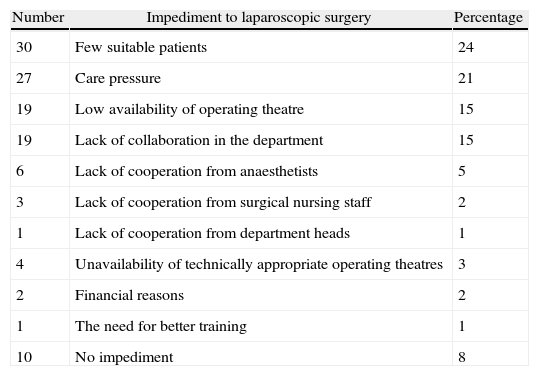
The key limitations explaining why the number of cases undertaken did not increase further are shown in Table 2. Healthcare pressure and there being few suitable candidate patients for laparoscopy with colorectal disorders is also worth highlighting. Some respondents (10) did not provide a reason in the survey, but they did not use this surgical approach.
Impediments to Increasing Laparoscopic Surgery.
| Number | Impediment to laparoscopic surgery | Percentage |
| 30 | Few suitable patients | 24 |
| 27 | Care pressure | 21 |
| 19 | Low availability of operating theatre | 15 |
| 19 | Lack of collaboration in the department | 15 |
| 6 | Lack of cooperation from anaesthetists | 5 |
| 3 | Lack of cooperation from surgical nursing staff | 2 |
| 1 | Lack of cooperation from department heads | 1 |
| 4 | Unavailability of technically appropriate operating theatres | 3 |
| 2 | Financial reasons | 2 |
| 1 | The need for better training | 1 |
| 10 | No impediment | 8 |
Despite the fact that at present there is clear evidence of the oncological safety and the superiority of the laparoscopic approach for colon surgery, in terms of short term outcomes, its use in clinical practice remains relatively low, with figures currently reaching 33% in the U.S.A., 30%11,12 in England and Australia and 26%13 in France. Spain is near the figure shown in the Viking project for rectal cancer of 21%.14 However, this is difficult to establish because there is no national register.
There are difficulties in implementing the laparoscopic approach in colorectal surgery in Spain for various reasons.5 It is technically difficult; hospitals are designed for health care and not for training and patient safety could be compromised during training periods.15
Different training activities are currently being undertaken to tackle this problem. Traditionally, the first stage in training involves attending courses where an expert performs surgery on patients. There are very few studies to assess the effect of this type of course on the process for increasing competence levels.8 The next stage usually consists of learning with patients under the mentorship of an expert, gradually introducing more complicated cases. It has been demonstrated that mentoring, in selected cases, reduces morbidity and conversion rates when compared with non-mentoring.4,16 In recent years, training supported by virtual reality simulators, animals and cadavers is increasingly used due to the level of evidence of its efficiency.4,6 However, there are few studies to reflect the extent of clinical implementation of the procedures taught.
Our study shows that 75% of the surgeons experienced an increase in operated patients after the course. In 57% of those, the percentage of colon surgery performed by laparoscopy increased to 25%, the total of these operations after the course reached an average of 35%. This percentage matches figures published in national registers.10–13 It should be noted that 38% of the surgeons had never used the laparoscopic approach prior to undertaking the course.
Other groups8 have published that, in a course showing live surgery on patients, the number of surgeons positively implementing observed techniques was 70%, although they mention that only 18% had no previous experience in colorectal laparoscopy. In recent publications, when cadavers were used in training, the number of surgeons who went on to perform the procedures in their clinical practice increased from 53% to 81%, and 26% increased at least one clinical case per week.17
There may be some limitations in these outcomes as the follow-up period was not the same for all the respondents from the time they completed the course until they participated in the survey. In addition this survey does not reflect other training activities undertaken after the course. However, we observe that for 21 (68%) out of 31 surgeons undertaking the course before or during 2010, implementation was high or very high. For 33 (83%) out of the 40 who took the course in 2011–2012, implementation was high or very high. There seems to be improved implementation for those who took the course in the past two years, with an OR=2.24 (95% CI: 1–7) but this is not significant (exact Fisher test, P=.171).
The number of trainees under 40 years of age who responded was 43% while they only represented 26% of the total number undertaking the course. Likewise, 62% of those who were performing laparoscopic colorectal surgery prior to the course responded while the total of those who stated that they did so prior to the course was 33%. Although the number of surgeons who responded to the survey did not exceed 50%, it is worth noting that they came from 60 different hospitals that included 13 general hospitals, 22 university hospitals and 25 regional hospitals; therefore, the sample in terms of the Spanish hospital network is large.
The respondents pointed out that the longer duration of laparoscopic operations compared to open surgery could present a challenge in implementing this technique, as this would limit the availability of operating theatres. Furthermore, many of the respondents work in small hospitals, with no colorectal surgery units and a small number of patients, which makes it less possible to make an adequate selection of patients.
ConclusionsOur data shows that 75% of the surgeons increased their clinical implementation of laparoscopic colorectal surgery, after undertaking a training course based on surgical simulation.
Conflict of InterestThe authors declare that there is no conflict of interests.
Please cite this article as: Manuel Palazuelos C, Alonso Martín J, Martín Parra JI, Gómez Ruiz M, Maestre JM, Redondo Figuero C, et al. Efecto de la simulación quirúrgica en la implementación clínica de procedimientos colorrectales laparoscópicos. Cir Esp. 2014;92:100–106.