In mild gallstone pancreatitis, cholecystectomy decreases the risk of recurrence. This should be performed during the initial hospitalisation, but even when this is performed, the hospital stay can be prolonged, with an increase in costs and morbidity.
The aim of this study is to compare the complication rate between patients who underwent an early cholecystectomy (<48h) versus a late one (>48h).
Materials and methodsA systematic search was performed in the following databases: PubMed, EMBASE, LILACS and Scielo. Articles on patients with acute, mild gallstone pancreatitis who required a cholecystectomy during their initial hospitalisation were included and compared with those undergoing a late cholecystectomy, in order to evaluate the complications, number of days of hospitalisation and need for readmission. The quality of the studies and the risks of bias were evaluated.
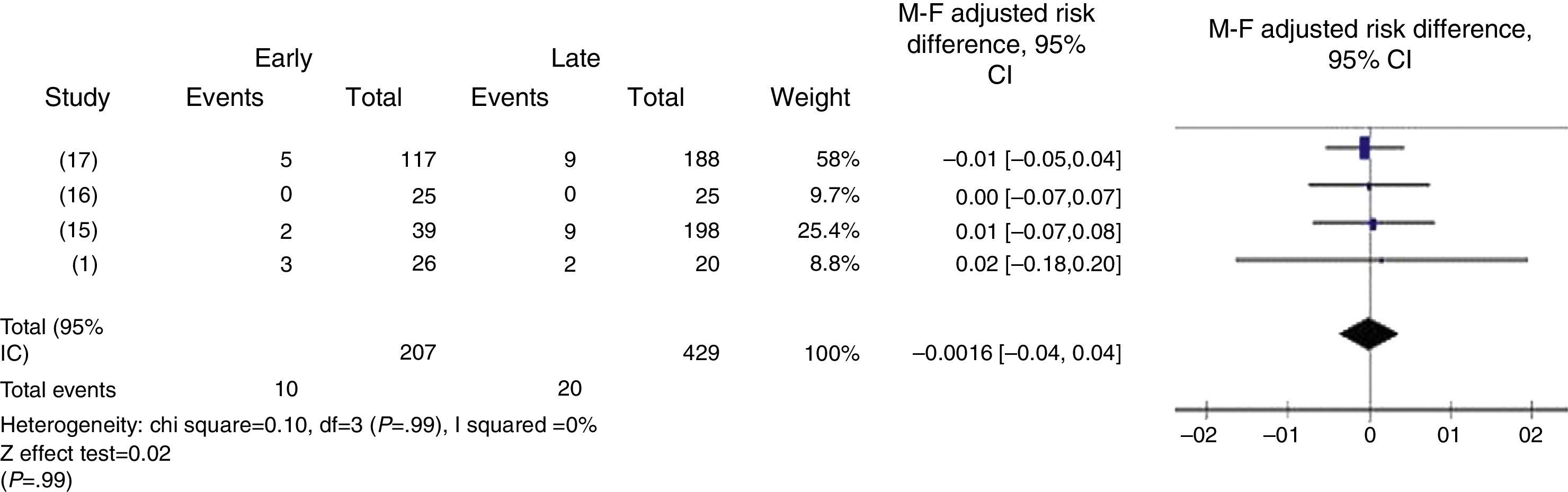
ResultsA total of 580 articles and summaries were identified which included 3 observational studies and a randomised clinical trial. A total of 636 patients who underwent a cholecystectomy during the initial hospitalisation were included. Ten of 207 (4.83%) in the early cholecystectomy group showed some type of complication, and 19 of 429 (4.42%) in the late cholecystectomy group, with a risk difference of −0.0016 IC 95% ([−0.04] to 0.04).
Three of the included studies should be considered of low quality and one of high quality. No publication bias was evidenced.
ConclusionNo differences in complication rate were found between patients who underwent an early cholecystectomy versus a late cholecystectomy; nevertheless, further studies should be carried out in order to confirm these findings.
En pancreatitis biliar leve, la colecistectomía disminuye el riesgo de recurrencia. Esta debe realizarse durante la hospitalización inicial, pero incluso en esta puede prolongarse la estancia hospitalaria, con aumento de costos y morbilidad.
El objetivo de este estudio es comparar las complicaciones entre los pacientes a los que se les realizó colecistectomía temprana (<48h) vs tardía (>48h).
Materiales y métodosSe realizó una búsqueda sistemática en las bases de datos: PubMed, EMBASE, LILACS y Scielo. Se incluyeron artículos de pacientes con pancreatitis aguda biliar leve que fueron llevados a colecistectomía durante la hospitalización inicial de manera temprana comparados con colecistectomía tardía, para evaluar las complicaciones, días de estancia hospitalaria y readmisión. Se evaluaron la calidad de los estudios y el riesgo de sesgos.
ResultadosSe identificaron 580 títulos y resúmenes de los cuales se incluyeron 3 estudios observacionales y un experimento clínico aleatorizado. Un total de 636 pacientes fueron incluidos, a los que se les realizó colecistectomía durante la hospitalización inicial. En 10 de 207 (4,83%) se presentó algún tipo de complicación en el grupo de colecistectomía temprana y 19 de 429 (4,42%) en el de colecistectomía tardía, con diferencia de riesgo de −0,0016 IC 95% ([−0.04]−0.04).
De los estudios incluidos 3 fueron de baja calidad y uno de alta calidad. No se evidenció sesgo de publicación.
ConclusiónNo se encontró diferencia entre los que son llevados a colecistectomía temprana en comparación con colecistectomía tardía en cuanto a complicaciones, sin embargo se deben realizar más estudios para confirmar o refutar estos hallazgos.
Cholelithiasis is still the most frequent cause of acute pancreatitis.1–3 In our area it is thought that 80% of acute pancreatitis cases are biliary in origin.4 Since Acosta and Ledesma5 demonstrated in 1974 that the passage of gallstones through the biliary tract and its transitory obstruction are related to the development of acute pancreatitis, it has been considered that the treatment of pancreatitis of biliary origin is cholecystectomy in order to prevent recurrence which can be up to 30%–40% two weeks after the initial episode.6,7
There has been ongoing controversy regarding the best time to perform a cholecystectomy since the 1980s. In response to this first question it is necessary to differentiate between mild and severe pancreatitis. We use the APACHE II scale to do this; a score greater than 8 classifies the pancreatitis as severe and a score of equal or less than 8 classifies it as mild.8 There is consensus on delaying cholecystectomy for patients with severe acute pancreatitis.2,9 Whereas in patients with mild biliary pancreatitis, it is currently accepted that cholecystectomy should be performed on initial hospitalisation, given the high risk of recurrence of pancreatitis and the patient being readmitted with biliary complications such as cholecystitis and biliary colic.6,10–12 Furthermore, there is no difference in peri-operative morbimortality compared to patients who were newly admitted to perform interval cholecystectomy.
At present, the question comes down to when is the best time to perform cholecystectomy during initial hospitalisation. The strategy used in the General Surgery Department of the Hospital of San José, considers the C reactive protein trend (CRP), and the average hospital stay was 7.1 days,13 a very long time for a disease which has rapid recovery and an excellent prognosis. Despite the fact that cholecystectomy is performed during initial hospitalisation, the average time it takes seems very long, increasing costs, the risk of hospital-acquired infection and morbimortality. Several articles have been published recently in favour of performing early cholecystectomy (<48h) for patients with acute mild biliary pancreatitis, and the objective of this article is to undertake a systematic review and meta-analysis of studies which compare performing early cholecystectomy (<48h) versus late cholecystectomy (>48h) in patients with mild acute pancreatitis, focussing on complications, readmission after 30 days and days of hospital stay, and is directed towards undertaking a clinical trial.
MethodologyType of StudySystematic revision of the literature and meta-analysis.
Inclusion and Exclusion CriteriaArticles were included which compared early (<48h) with late laparoscopic cholecystectomy (>48h) for cases of acute mild biliary pancreatitis reporting postoperative complications, hospital stay, readmission within 30 days post surgery and who underwent laparoscopic cholecystectomy on initial hospitalisation, published after the Atlanta consensus of 1992,14 which classifies pancreatitis into mild and severe.
The following were used as exclusion criteria:
- -
Studies including patients less than 18 years of age.
- -
Studies including patients who had undergone cholecystectomy.
- -
Studies including patients with pancreatitis of other origins and severe pancreatitis.
- -
Studies which included pregnant patients.
The following electronic databases were reviewed: PubMed, EMBASE, LILACS and SCIELO.
In addition, the authors of the chosen articles were contacted to gain further information: Falor et al. provided the complete text of the study.
The search was confined to English and Spanish.
Information Searching ProcedureThe strategy for electronic searching was as follows:
- -
(«cholecystectomy» [MeSH Terms] OR «cholecystectomy» [All Fields]) AND («pancreatitis» [MeSH Terms] OR «pancreatitis» [All Fields]) AND early[All Fields] AND («1992/01/01» [PDAT]: «2012/12/31» [PDAT]).
The titles and abstracts were independently reviewed by 2 authors (LRP and JFP), determining the studies which were included.
The studies included were independently reviewed following the guidelines outlined below: the agreements were reached through the intervention of the expert and principal author (GALD).
- 1.
Year and language of publication.
- 2.
Country.
- 3.
Time taken to complete the study.
- 4.
Inclusion and exclusion criteria.
- 5.
Sample size.
- 6.
Time of early and late intervention.
- 7.
Primary and secondary outcome.
- 8.
Methodological quality.
- -
Primary outcomes: the complications reported in patients with mild acute biliary pancreatitis who had undergone early laparoscopic cholecystectomy from the immediate postoperative period up to 30 days afterwards compared to patients who had undergone late cholecystectomy.
- -
Secondary outcomes: Days of hospital stay post surgery were assessed from the immediate post-operative period to discharge from hospital, in patients with acute mild pancreatitis who were to undergo laparoscopic cholecystectomy, and readmission within the first 30 days of the post-operative period.
The characteristics of the articles and their validity were assessed using Cochrane's GRADEpro.
The abovementioned tool was used independently by 2 authors (LRP and JFP) to assess the methodological quality of each study, as well as the process for extracting each piece of data. Subsequently a comparison was made of this assessment to reduce the risk of bias.
Data AnalysisWith regard to primary outcome, the data on the complications reported in the included studies were grouped and their frequency in the compared groups was determined; risk difference was used as a measurement to perform the meta-analysis; forest plots were created and publication bias assessed using RevMan 5, with Mantell–Haenzel statistical analysis, with fixed effect. The difference in days of hospital stay and readmissions in the postoperative period up to 30 days was reported, in each study included.
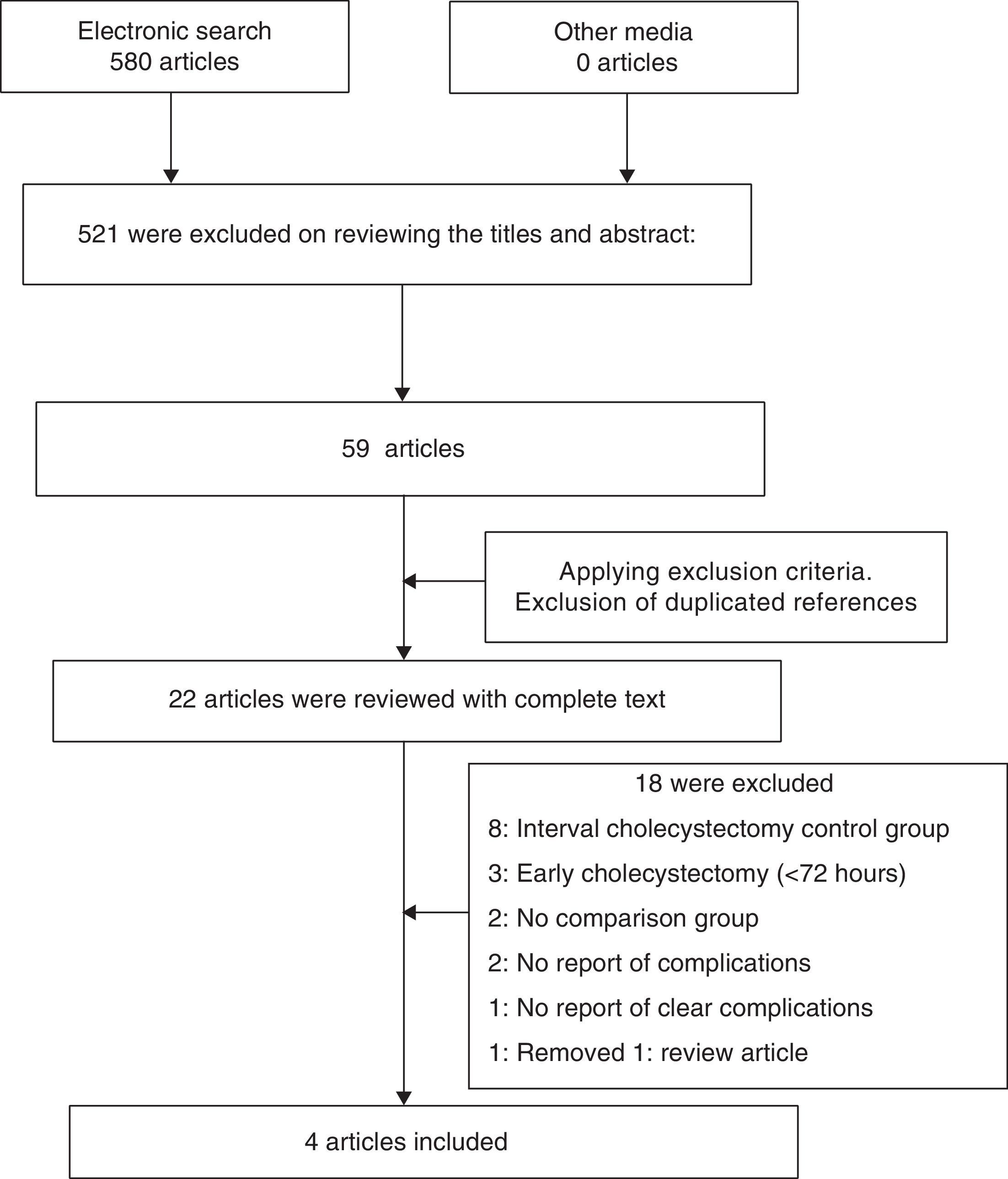
Results580 articles were identified in the initial search. After reviewing the titles, articles with titles which were not relevant were rejected, leaving 59 articles. The eligibility and exclusion criteria were applied. 22 articles were eligible and their entire text was reviewed. This resulted in 5 articles in which early cholecystectomy was compared with late cholecystectomy in patients with mild acute biliary pancreatitis, as well as the complications and the hospital stay of these operations. One article which did meet the eligibility criteria was removed from those included because the report of complications was not clear. The reasons for excluding the remaining articles are detailed in Fig. 1. Of the 4 articles included, 3 are observational and one is a randomised controlled clinical trial.1,15–17 These were quality rated using Cochrane's GRADEpro, which found that the randomised clinical trial was high quality and the 3 observational studies were low quality.
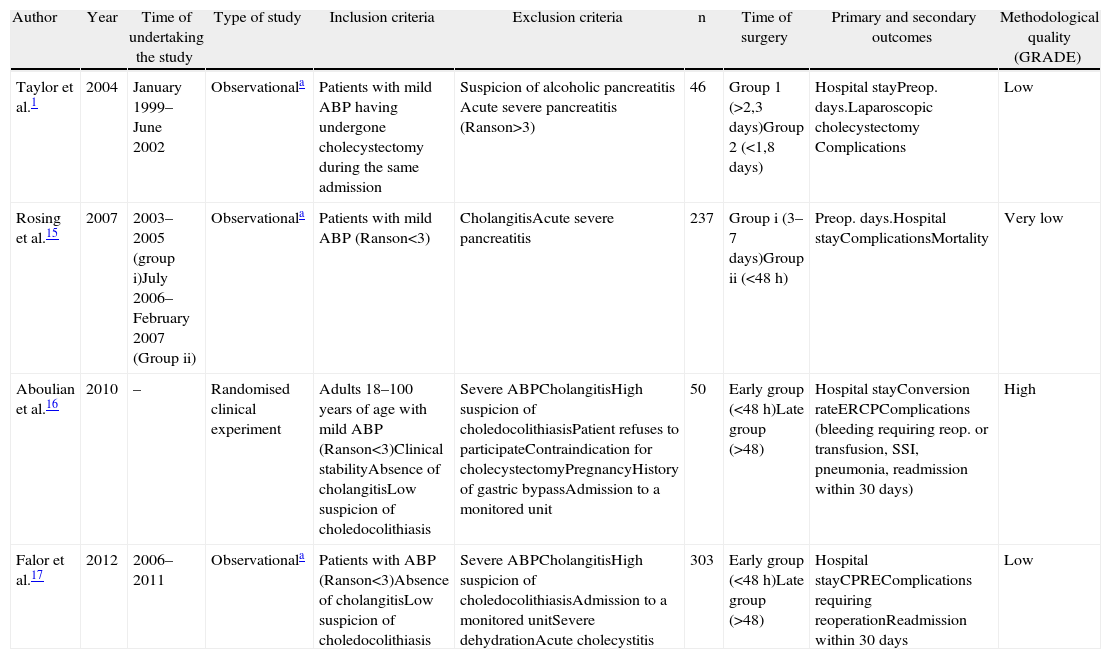
The total number of patients in the included studies was 636, of whom 207 underwent early laparoscopic cholecystectomy (<48h) and 429 patients underwent late laparoscopic cholecystectomy (>48h). The studies’ characteristics are shown in Table 1. Days of hospital stay and complications were reported in all the studies; 3 were observational and one a controlled clinical trial. The severity of the pancreatitis was assessed in all the studies using the Ranson scale.18 The studies are homogenous in terms of population screened, intervention, control and outcome.
Characteristics of the Studies Included.
| Author | Year | Time of undertaking the study | Type of study | Inclusion criteria | Exclusion criteria | n | Time of surgery | Primary and secondary outcomes | Methodological quality (GRADE) |
| Taylor et al.1 | 2004 | January 1999–June 2002 | Observationala | Patients with mild ABP having undergone cholecystectomy during the same admission | Suspicion of alcoholic pancreatitis Acute severe pancreatitis (Ranson>3) | 46 | Group 1 (>2,3 days)Group 2 (<1,8 days) | Hospital stayPreop. days.Laparoscopic cholecystectomy Complications | Low |
| Rosing et al.15 | 2007 | 2003–2005 (group i)July 2006–February 2007 (Group ii) | Observationala | Patients with mild ABP (Ranson<3) | CholangitisAcute severe pancreatitis | 237 | Group i (3–7 days)Group ii (<48h) | Preop. days.Hospital stayComplicationsMortality | Very low |
| Aboulian et al.16 | 2010 | – | Randomised clinical experiment | Adults 18–100 years of age with mild ABP (Ranson<3)Clinical stabilityAbsence of cholangitisLow suspicion of choledocolithiasis | Severe ABPCholangitisHigh suspicion of choledocolithiasisPatient refuses to participateContraindication for cholecystectomyPregnancyHistory of gastric bypassAdmission to a monitored unit | 50 | Early group (<48h)Late group (>48) | Hospital stayConversion rateERCPComplications (bleeding requiring reop. or transfusion, SSI, pneumonia, readmission within 30 days) | High |
| Falor et al.17 | 2012 | 2006–2011 | Observationala | Patients with ABP (Ranson<3)Absence of cholangitisLow suspicion of choledocolithiasis | Severe ABPCholangitisHigh suspicion of choledocolithiasisAdmission to a monitored unitSevere dehydrationAcute cholecystitis | 303 | Early group (<48h)Late group (>48) | Hospital stayCPREComplications requiring reoperationReadmission within 30 days | Low |
ABP, acute biliary pancreatitis.
Two of the observational studies presented selection bias, with differences in the groups being compared which might influence the decision as to whether to operate early or late. In Rosing et al.’s work there is a difference in the average amylasaemia level on admission; it was lower in the early operation group, and the age was younger in Falor et al.’s article.
In Aboulian et al.’s study, on randomisation, the early intervention group was at an advantage compared to the late group in terms of hospital stay. In this case, the surgery affected the result (confusion bias).
There is performance bias in all the studies, because the severity of the pancreatitis was assessed using the Ranson scale, which has to be completed in 24 and 48h. Given the characteristics of the studies, this assessment was not completed in 48h. With regard to the methodological quality of the studies included, according to GRADE, only Aboulian et al.’s study is high quality and the rest are low quality (Table 1).
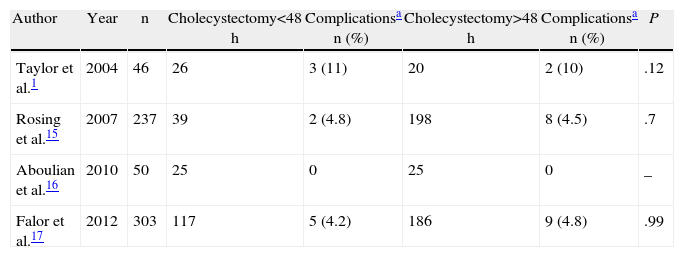
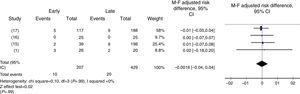
Complications in Early Versus Late CholecystectomyOf the 4 studies included, the total number of patients who underwent early laparoscopic cholecystectomy was 207, of whom 10 patients (4.83%) presented some type of postoperative complication. In comparison, 429 patients underwent late cholecystectomy (>48h) of whom 19 (4.42%) presented some type of complication. The individual outcomes of each study are shown in Table 2.
Post-operative Complications With Early Versus Late Laparoscopic Cholecystectomy in Patients With Mild Acute Biliary Pancreatitis.
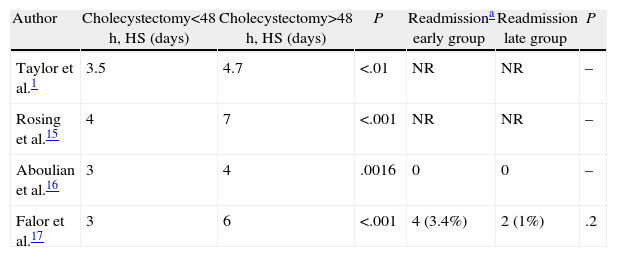
In the 4 studies included there is a statistically significant reduction in hospital stay for the patients in the early cholecystectomy group, 3–4 days compared to 4–7 days in the late group. Readmission after 30 days was only reported in 2 articles (Table 3), without showing any difference between the 2 groups.
Postoperative Hospital Stay and Readmission in Patients With Acute Mild Biliary Pancreatitis According to Early or Late Cholecystectomy Group.
| Author | Cholecystectomy<48h, HS (days) | Cholecystectomy>48h, HS (days) | P | Readmissiona early group | Readmission late group | P |
| Taylor et al.1 | 3.5 | 4.7 | <.01 | NR | NR | – |
| Rosing et al.15 | 4 | 7 | <.001 | NR | NR | – |
| Aboulian et al.16 | 3 | 4 | .0016 | 0 | 0 | – |
| Falor et al.17 | 3 | 6 | <.001 | 4 (3.4%) | 2 (1%) | .2 |
HS, hospital stay; NR, not reported.
In patients with predicted acute mild biliary pancreatitis, with a Ranson scale of less than 3, no differences were seen in the risk of postoperative complications [DR 0.016 (−0.04 to 0.049)] (Fig. 2) with early laparoscopic cholecystectomy (<48h) compared to late laparoscopic cholecystectomy (>48h).
Assessment of Publication BiasNo publication bias was identified, using the funnel plot method.
DiscussionThis is the first systematic review and meta-analysis of studies which compare early (<48h) with late (>48h) cholecystectomy in patients with mild acute biliary pancreatitis. As complications with laparoscopic cholecystectomy are not common, performing a clinical trial to respond to this question seems a remote prospect.
Amongst the studies included, the characteristics of the patients and the prognosis prior to surgery are homogenous (Ranson average 1); therefore, a meta-analysis was undertaken which shows that there is no difference between the 2 operations in terms of number of complications. Fortunately, no mortality or changes of the course of the pancreatitis were reported in any of the studies included. Despite the fact that these outcomes are encouraging, they should be interpreted with caution: in other words, for a patient to benefit from early surgery it must be ensured that their pancreatitis is mild and patients at risk of progressing to severe pancreatitis should be excluded. On this point, we consider that the APACHE II scale performs better than the Ranson score; therefore, this is a weakness in the studies included.
Another important point is to distinguish cholecystitis from biliary pancreatitis, 2 entities which can entail hyperamylasaemia. Therefore it is important to exclude these types of patients, as this can constitute confusion bias, operating on these patients as if they had pancreatitis, when they really have acute cholecystitis.
Other limitations of the study are that 3 of the 4 articles were written by the same group of researchers, which could cause bias in publishing favourable outcomes.
Furthermore, we consider that there should be international consensus on defining the precise time (hours, days) of early cholecystectomy, as the 48h cut-off point is rather arbitrary and, perhaps, unachievable for most surgical departments due to their healthcare services.
We consider that although the existing evidence is of low quality, this outcome is encouraging in terms of changing the paradigm of setting such a delay (which we consider unnecessary) for a disease which is benign and has a good prognosis.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Randial Pérez LJ, Fernando Parra J, Aldana Dimas G. Seguridad de la colecistectomía laparoscópica temprana (<48h) para pacientes con pancreatitis aguda biliar leve: revisión sistemática de la literatura y metaanálisis. Cir Esp. 2014;92:107–113.
Presented at the 38th Columbian Congress of Surgery, August 2012.