Duodenal switch (DS) is considered one of the most effective techniques to achieve weight loss and reduce comorbidities in patients with morbidly obesity.
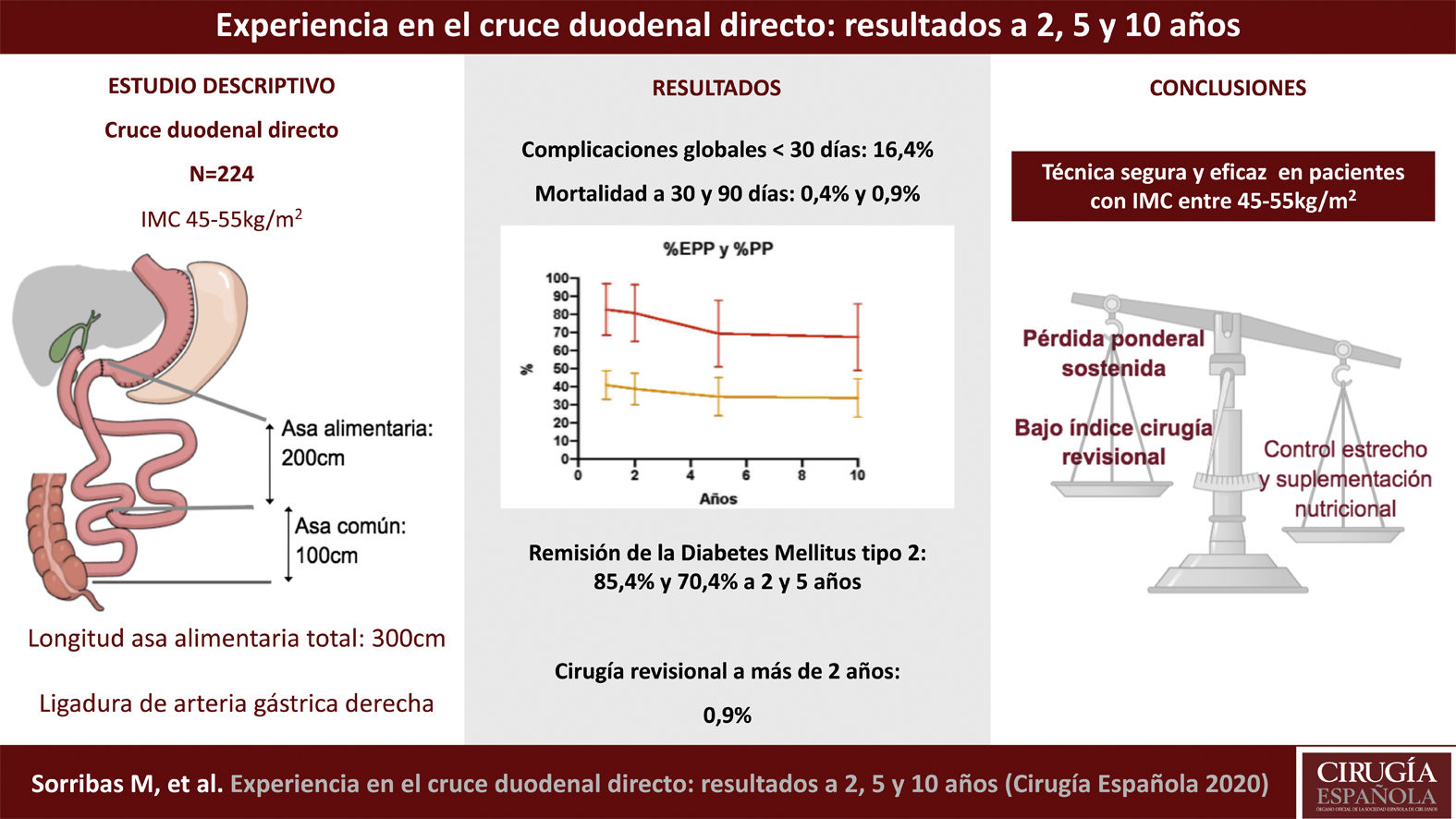
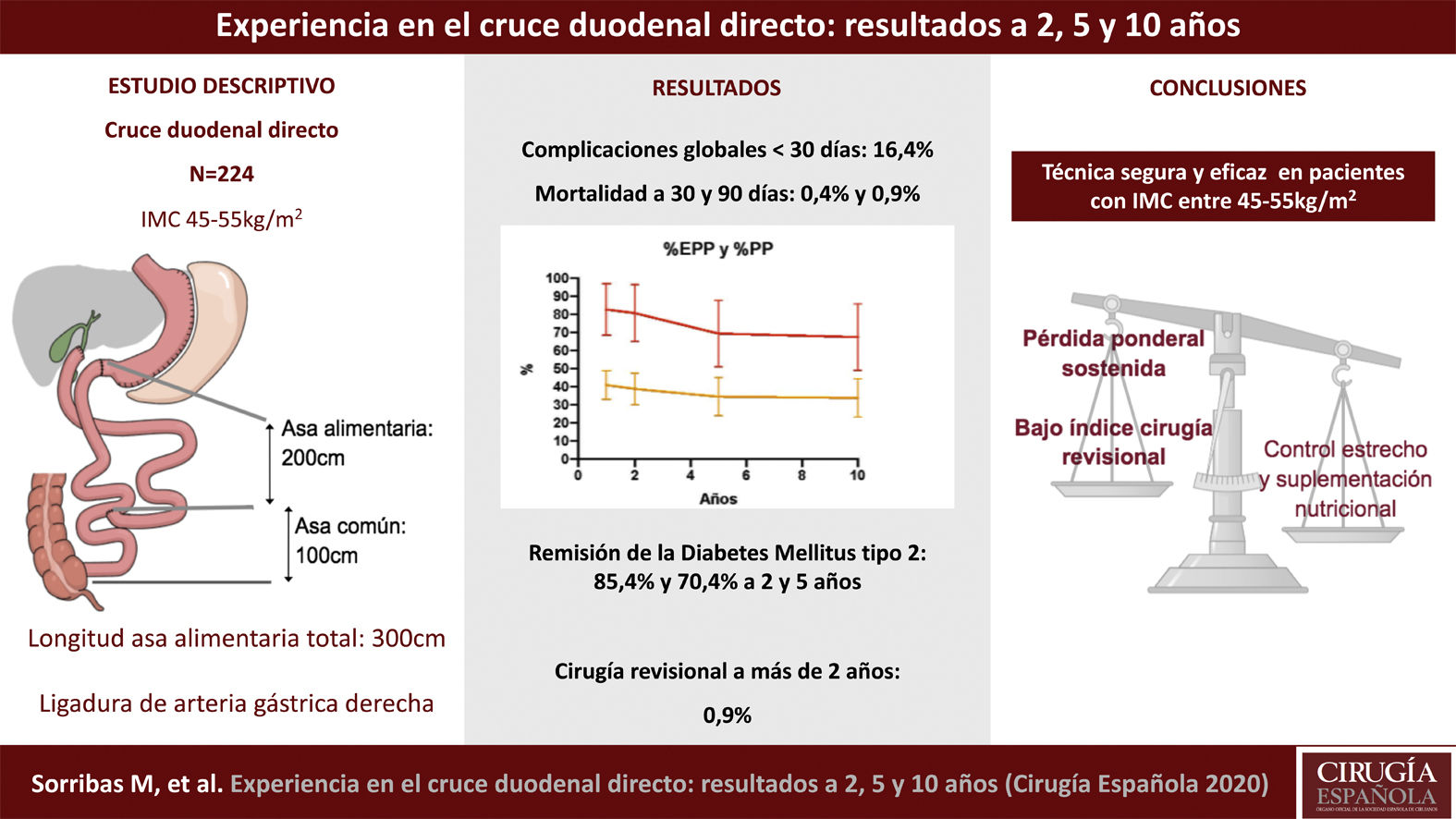
Material and methodsDescriptive single-center study. 224 patients were analyzed who underwent direct laparoscopic DS in our center. The objective was to describe the results of weight, resolution of comorbidities, nutritional supplementation and postoperative complications at 2, 5 and 10 years.
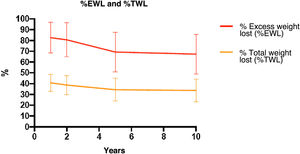
ResultsThe mean age of the cohort was 49.3 [23−65] years and the mean weight and BMI were 131.8 [20] kg and 49.8 [5] kg/m2. The excess weight lost percentage at 2, 5 and 10 years was 80.6[15]%, 69.3[18]%, 67.4[18]%, respectively. Complete remission of diabetes was evidenced at 2 and 5 years in 35 (85.4%) and 27 (70.4%) patients. In the immediate postoperative period, the complication rate for Clavien-Dindo ≥ III was 15 patients (6.7%) and mortality at 30 and 90 days was 1 (0.4%) and 2 (0.9%) patients. Revisional surgery was performed in 2 patients (0.9%). 80% of the patients required an extra nutritional supplement up to 10 years after surgery.
ConclusionsDirect DS is a safe and effective technique in patients with a BMI between 45 and 55 kg/m2. Weight loss is maintained with a low rate of revision surgery. It is a metabolically effective technique that entails the need for a close postoperative follow-up to assess nutritional supplementation
El cruce duodenal (CD) se considera una de las técnicas más efectivas para lograr la pérdida de peso y disminuir las comorbilidades en pacientes con obesidad mórbida.
Material y métodosEstudio descriptivo unicéntrico en el que se analizaron 224 pacientes intervenidos de CD directo con ligadura de la arteria gástrica derecha laparoscópico. El objetivo fue describir los resultados ponderales, resolución de comorbilidades, suplementación nutricional y complicaciones postquirúrgicas a dos, cinco y 10 años.
ResultadosLa edad media de la cohorte fue de 49,3 (23−65) años, el peso e índice de masa corporal (IMC) medio fueron de 131,8(20) kg y 49,8(5) kg/m2. El porcentaje de exceso de peso perdido a dos, cinco y 10 años fue de 80,6(15)%, 69,3(18)%, 67,4(18)%, respectivamente. La remisión completa de la diabetes a dos y cinco años se evidenció en 35 (85,4%) y 27 (70,4%) pacientes. En el postoperatorio inmediato, la tasa de complicaciones Clavien-Dindo ≥ III fue en 15 pacientes (6,7%) y la mortalidad a 30 y 90 días fue de uno (0,4%) y dos (0,9%) pacientes. La necesidad de cirugía revisional se realizó en dos pacientes (0,9%). El 80% de los pacientes requirió en algún momento suplementación nutricional extra a partir de los dos años de la cirugía.
ConclusionesEl CD directo es una técnica con un bajo índice de complicaciones quirúrgicas en pacientes con un IMC entre 45 y 55 kg/m2. El control metabólico y la pérdida ponderal es sostenida con un bajo índice de cirugía revisional. Aún así, conlleva la necesidad de un seguimiento postquirúrgico estrecho para la valoración de suplementación nutricional.
Obesity is a chronic, multifactorial disease that requires a multidisciplinary approach. In the Spanish population, the prevalence of obesity in adults (25–60 years) has increased from 14.5% in 2003 to 22%–28% today.1 The only treatment for obesity that has been shown to be effective in the long term is bariatric surgery (BS). The Spanish Society of Obesity Surgery (Sociedad Española de Cirugía de la Obesidad, SECO) and the Spanish Society of Endocrinology (Sociedad Española de Endocrinología, SEEDO) maintain the BS indication criteria agreed upon by the NIH in 1991 (body mass index [BMI] ≥35 kg/m2 with comorbidities, or BMI ≥40 kg/m2).2 Starting in 1973, when Dr. García Díaz in Seville and in 1976 Dr. Sánchez Ortega and Dr. Masdevall3 performed the first BS in Spain, the number and type of surgical interventions has increased progressively. Since then, the results obtained have provided evidence on different surgical techniques in order to optimize weight loss, metabolic and quality-of-life results in obese patients.3
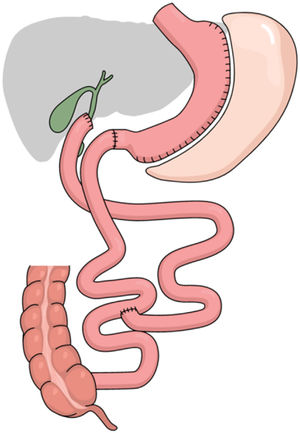
Our hospital BS program was created in 2002, initially performing techniques such as gastric bypass and vertical banded gastroplasty. In 2006, sleeve gastrectomy and direct biliopancreatic diversion with duodenal switch (DS) were introduced. Progressively, and as a treatment for weight regain and/or reflux after sleeve gastrectomy, revision surgery appeared. Likewise, to reduce complications in cases of super obesity, two-stage surgery was introduced in the DS and Single-Anastomosis Duodenum Ileal Switch (SADIS) techniques. DS was described by Hess and Marceau in 19984,5 as a modification of the biliopancreatic diversion (BPD) technique described by Scopinaro. This technique consists of sleeve gastrectomy with preservation of the antrum/pylorus (instead of a horizontal gastrectomy) and a Roux-en-Y reconstruction with a biliopancreatic limb length of 100 cm (instead of 50 cm) and an alimentary limb length between 150 cm and 200 cm (instead of 100 cm).4,5 In Spain, Dr. Aniceto Baltasar was the first surgeon to perform DS and became the benchmark in DBP in our country.6 DS is one of the techniques with the best long-term weight and metabolic results. Despite this, according to the registry of the International Federation for Surgery of Obesity (IFSO), DS only represents 1.5% of all bariatric surgeries. The main fear of DS is the complexity of the technique in duodenal dissection and the risk of injury to the portal triad. To simplify the technique, measures like right gastroepiploic and/or gastric artery ligation have been described. The good results and low risk of complications of DS (direct or in 2 stages) have led to a change in the paradigm of malabsorptive surgery, turning DS into a hypoabsorptive technique that achieves the benefits of malabsorptive techniques without nutritional complications that have confined DS between the abyss of malnutrition and superobesity.7
The objective of this study is to describe our experience with direct laparoscopic DS and the outcomes 2, 5 and 10 years after surgery by analyzing anthropometric parameters, evolution of comorbidities, need for nutritional supplements and short/long-term complications.
MethodsWe conducted a single-center retrospective descriptive study. From a global series of 281 patients operated on for DS between May 2006 and December 2019, we analyzed the 224 patients who underwent direct laparoscopic DS surgery. BS was indicated following the criteria of the position statements of the Spanish societies for obesity surgery.8
Preoperative circuitPrior to surgery, all patients were evaluated by a multidisciplinary team. Two weeks before surgery, the patients followed a 600−800 kcal hypocaloric high-protein liquid diet to force weight loss.
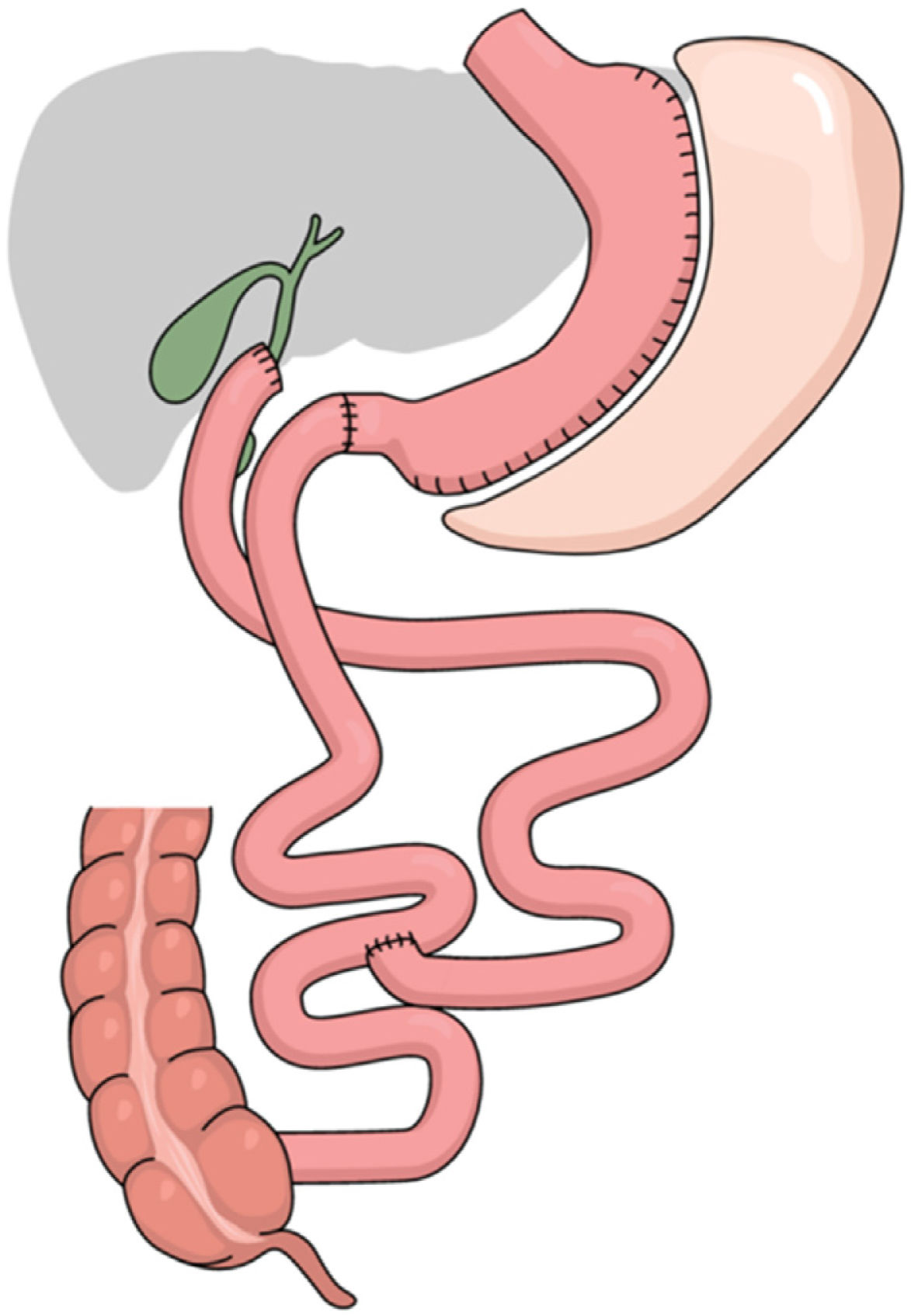
Surgical technique: simplified duodenal switch with right gastric artery ligation and common loop length of 100 cm and alimentary loop length of 200 cm (Fig. 1)
Placement of the patient in the French position, using 30° optics and six trocars (Fig. 2). Surgery was divided into different surgical stages: (I) Dissection of the antrum and duodenal portion up to 2 cm distal to the pylorus, with clipping of the right gastroepiploic and right gastric arteries; (II) Sleeve gastrectomy with antral preservation stented with a 36Fr orogastric tube; (III) Exploration of the esophageal hiatus, proceeding with the reduction and closure of crura in case of hiatal hernia; (IV) division of the duodenum with a 60 mm/3.5 mm endostapler and bioabsorbable suture line reinforcement; (V) Intestinal loop measurements: 100 cm common limb and 200 cm alimentary limb, for a total length of 300 cm; (VI) Manual end-to-side duodenal-ileal anastomosis in 2 planes with 2/0 and 3/0 resorbable monofilament; (VII) Base of limb with linear semi-mechanical side-to-side ileo-ileal anastomosis with 45 mm/2.5 mm endostapler; (VIII) Closure of the mesenteric defect and Petersen’s space with continuous non-absorbable suture. (IX) Sutures were checked for leaks with air and methylene blue; (IX) Transection of the biliopancreatic limb with a 60 mm/2.5 mm endostapler for Roux-en-Y reconstruction of the gastrointestinal tract; (X) Placement of a drain tube at the duodenal stump and angle of His.
Follow-upDuring postoperative hospitalization, the team of dietitians was in charge of reinforcing nutrition and supplementation guidelines before hospital discharge, including the recommendation of generic or specific multivitamin supplements for hypoabsorptive surgery, including a protein powder for one month, 1200 mg of calcium with 800 IU of cholecalciferol daily, together with 16 000 IU hydroferol every 15 days during the first three months, after which the dosage was adjusted according to lab test values. After discharge, follow-up visits were scheduled for 1, 3, 6, 12, 18, and 24 months after surgery, followed by annual visits for up to six years.
ObjectivesThe main objective was the evaluation of anthropometric changes 2, 5 and 10 years after DS. The secondary objective was to analyze the evolution of associated comorbidities, postoperative complications, associated mortality, and the need for nutritional supplementation.
Anthropometric parametersWeight and height were recorded at each annual visit for up to six years, and subsequently up to 10 years by phone. Weight changes were analyzed according to BMI (BMI, weight/height), percentage of total weight loss (%TWL, calculated as initial weight-current weight/initial weight × 100) and percentage of excess weight lost (%EWL, calculated as initial weight ̶ current weight/initial weight ̶ ideal weight, [BMI 25 kg/m2] × 100). Cases with BMI > 35 kg/m2 were considered failed weight loss.
Evolution of related metabolic diseasesFor the remission of T2DM, the Buse et al. criteria9 were applied; meanwhile, the remission of hypertension and dyslipidemia was determined by the absence of the need for medical treatment. The need for nutritional supplements was evaluated two years after surgery.
Statistical analysisFrequency tables and percentages were used for qualitative data and measures of central tendency for quantitative variables. In all cases, statistical significance was a P < .05. The IBM-SPSS v.20 statistical program was used.
ResultsBaseline demographic dataFrom May 2006 to December 2019, 281 patients underwent DS surgery, 234 of which were treated in one operation and 224 by laparoscopy. This study analyzes the 224 cases of direct laparoscopic DS. The mean age was 49.3 (23−65) years, and 73.7% were women (n = 165). The mean weight and BMI were 131.8(20) kg and 49.8(5) kg/m2. Preoperatively, 18.3% (n = 41) had type 2 diabetes mellitus (T2DM), 60.7% (n = 136) hypertension, 34.8% (n = 77) dyslipidemia, and 62.5% (n = 140) obstructive sleep apnea syndrome (OSA).
Follow-upThe percentage of patients who were followed up for 2 years was 83% (n = 171), for 5 years 81% (n = 132), and for 10 years 85% (n = 51).
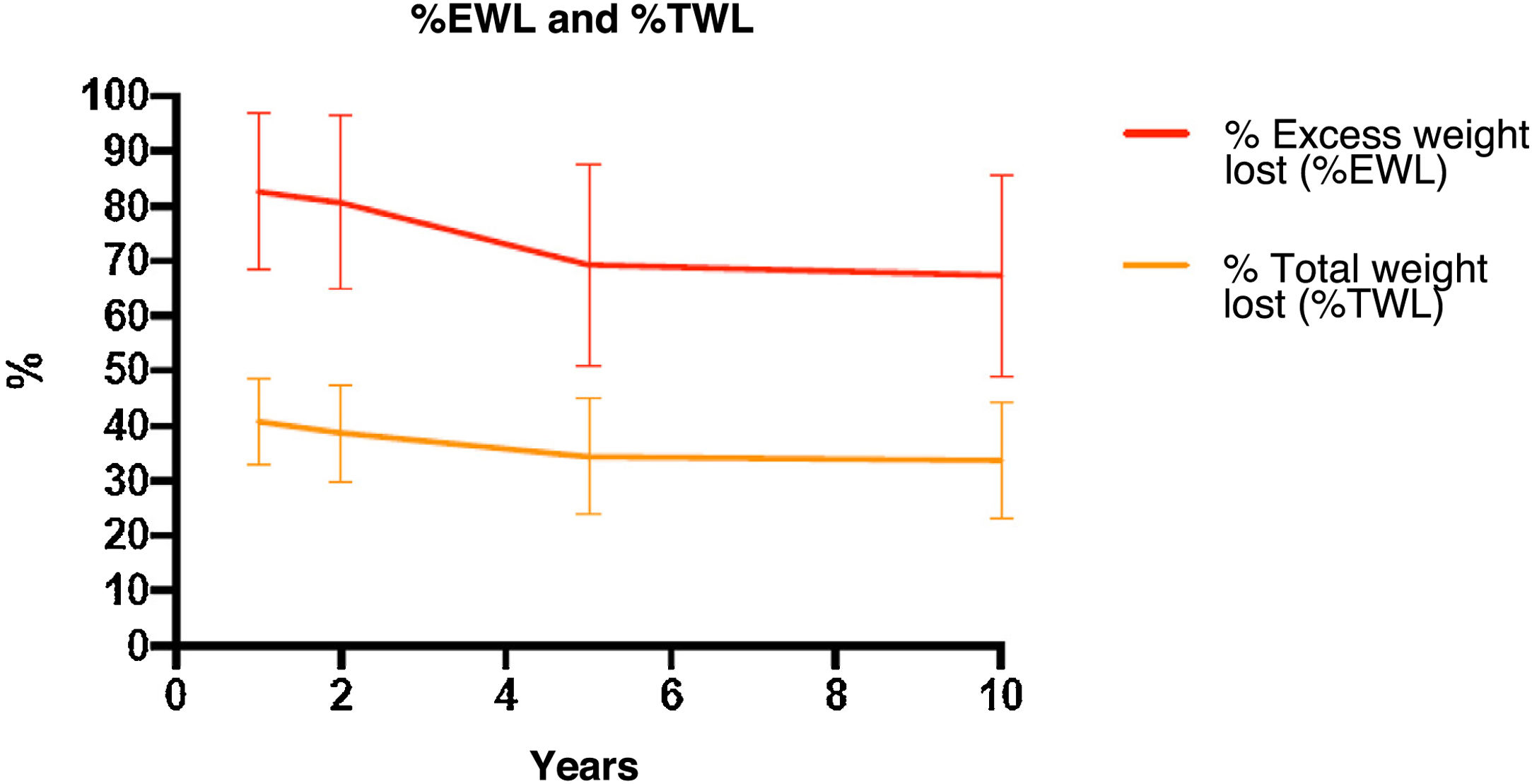
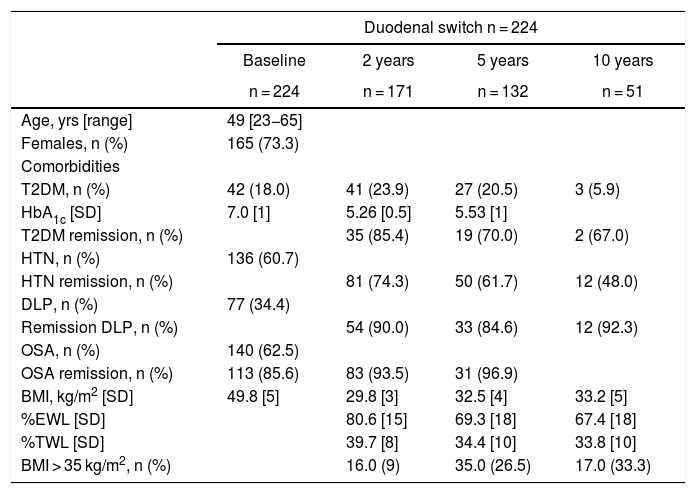
Weight evolutionTable 1 and Fig. 3 show the changes in weight. Weight loss after 2, 5 and 10 years was sustained, with a %EWL of 80.6(15)%, 69.3(18)%, and 67.4(18)%, respectively. The percentage of patients with inadequate weight loss (BMI > 35 kg/m2) after 2 years was 9.5% (n = 171), after 5 years 26.5% (n = 132), and after 10 years 33.3% (n = 51).
Baseline demographic data, weight evolution and remission of comorbidities.
| Duodenal switch n = 224 | ||||
|---|---|---|---|---|
| Baseline | 2 years | 5 years | 10 years | |
| n = 224 | n = 171 | n = 132 | n = 51 | |
| Age, yrs [range] | 49 [23−65] | |||
| Females, n (%) | 165 (73.3) | |||
| Comorbidities | ||||
| T2DM, n (%) | 42 (18.0) | 41 (23.9) | 27 (20.5) | 3 (5.9) |
| HbA1c [SD] | 7.0 [1] | 5.26 [0.5] | 5.53 [1] | |
| T2DM remission, n (%) | 35 (85.4) | 19 (70.0) | 2 (67.0) | |
| HTN, n (%) | 136 (60.7) | |||
| HTN remission, n (%) | 81 (74.3) | 50 (61.7) | 12 (48.0) | |
| DLP, n (%) | 77 (34.4) | |||
| Remission DLP, n (%) | 54 (90.0) | 33 (84.6) | 12 (92.3) | |
| OSA, n (%) | 140 (62.5) | |||
| OSA remission, n (%) | 113 (85.6) | 83 (93.5) | 31 (96.9) | |
| BMI, kg/m2 [SD] | 49.8 [5] | 29.8 [3] | 32.5 [4] | 33.2 [5] |
| %EWL [SD] | 80.6 [15] | 69.3 [18] | 67.4 [18] | |
| %TWL [SD] | 39.7 [8] | 34.4 [10] | 33.8 [10] | |
| BMI > 35 kg/m2, n (%) | 16.0 (9) | 35.0 (26.5) | 17.0 (33.3) | |
BMI = body mass index; T2DM = Diabetes Mellitus type 2; HTN = hypertension; DLP = dyslipidemia, OSA: obstructive sleep apnea.
Preoperatively, 41 patients had a diagnosis of T2DM with a history of T2DM of 6.0(4) years. In total, 13 of these patients (31%) were receiving insulin treatment. Mean baseline HbA1c was 7.0(1)%, which decreased to 5.3(0.5)% and 5.5(1)% after 2 and 5 years, respectively. According to the Buse criteria, complete remission of T2DM after 2 and 5 years was 85% (n = 35) and 70% (n = 19); after 10 years, 2 patients out of 3 presented remission. Despite the recurrence of T2DM, 2 and 5 years after surgery 100% and 96.3% of the patients maintained an HbA1c <7%, respectively. All diabetic patients abandoned treatment except for 3 patients in whom it was replaced by oral hypoglycemic medications. The remission of dyslipidemia, arterial hypertension, and OSA was greater than 50% after 2, 5 and 10 years (Table 1).
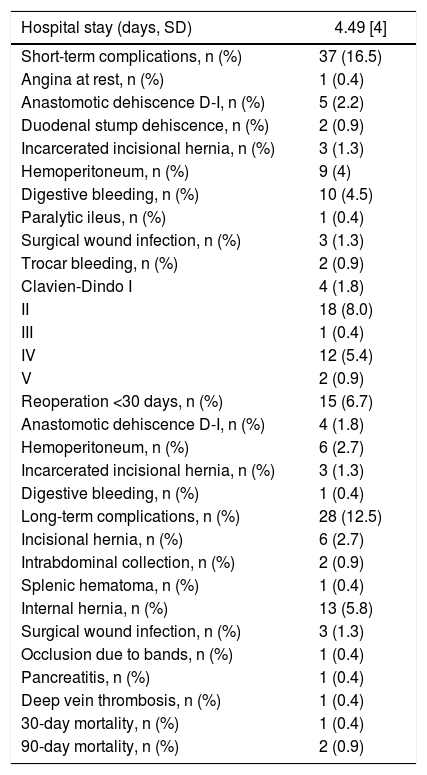
Postoperative complications16.4% (n = 37) of the patients presented complications in the immediate postoperative period (<30 days), and 6.7% (n = 15) were serious complications (Clavien-Dindo ≥ III) (Table 2). The urgent reoperation rate within 30 days of surgery was 6.3% (n = 14). The medium-long term complication rate (>30 days) was 12.5% (n = 28). The 30-day mortality rate was 0.4% (n = 1), and the 90-day rate 0.9% (n = 2), in both cases secondary to refractory sepsis of abdominal origin associated with multiple-organ failure caused by dehiscence of the duodeno-ileal anastomosis. Revision surgery after DS was 0.9% (n = 2): conversion from DS to gastric bypass was performed in one patient due to gastroesophageal reflux secondary to gastric stenosis, and in another patient closure of the mesenteric orifice and Petersen’s space due to recurrent subocclusive crises. The overall mean hospital stay was 4.5(5) days.
Hospital stay and postoperative complications.
| Hospital stay (days, SD) | 4.49 [4] |
|---|---|
| Short-term complications, n (%) | 37 (16.5) |
| Angina at rest, n (%) | 1 (0.4) |
| Anastomotic dehiscence D-I, n (%) | 5 (2.2) |
| Duodenal stump dehiscence, n (%) | 2 (0.9) |
| Incarcerated incisional hernia, n (%) | 3 (1.3) |
| Hemoperitoneum, n (%) | 9 (4) |
| Digestive bleeding, n (%) | 10 (4.5) |
| Paralytic ileus, n (%) | 1 (0.4) |
| Surgical wound infection, n (%) | 3 (1.3) |
| Trocar bleeding, n (%) | 2 (0.9) |
| Clavien-Dindo I | 4 (1.8) |
| II | 18 (8.0) |
| III | 1 (0.4) |
| IV | 12 (5.4) |
| V | 2 (0.9) |
| Reoperation <30 days, n (%) | 15 (6.7) |
| Anastomotic dehiscence D-I, n (%) | 4 (1.8) |
| Hemoperitoneum, n (%) | 6 (2.7) |
| Incarcerated incisional hernia, n (%) | 3 (1.3) |
| Digestive bleeding, n (%) | 1 (0.4) |
| Long-term complications, n (%) | 28 (12.5) |
| Incisional hernia, n (%) | 6 (2.7) |
| Intrabdominal collection, n (%) | 2 (0.9) |
| Splenic hematoma, n (%) | 1 (0.4) |
| Internal hernia, n (%) | 13 (5.8) |
| Surgical wound infection, n (%) | 3 (1.3) |
| Occlusion due to bands, n (%) | 1 (0.4) |
| Pancreatitis, n (%) | 1 (0.4) |
| Deep vein thrombosis, n (%) | 1 (0.4) |
| 30-day mortality, n (%) | 1 (0.4) |
| 90-day mortality, n (%) | 2 (0.9) |
Short-term complications: <30 days post-op; Long-term complications: >30 days post-op. Anastomosis D-I: duodenal-ileal anastomosis. SD: standard deviation.
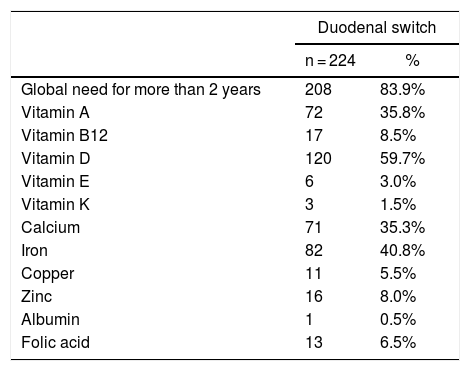
As Table 3 shows, after more than two years, most of the patients required at some point some type of nutritional supplement apart from the usual multivitamin and calcium supplement for the treatment of abnormal nutritional levels, without specifying the existence of deficit. Only one patient (0.5%) presented hypoalbuminemia more than 2 years after surgery, which was resolved with protein supplementation.
Need for extra nutritional supplementation with basic supplementation.
| Duodenal switch | ||
|---|---|---|
| n = 224 | % | |
| Global need for more than 2 years | 208 | 83.9% |
| Vitamin A | 72 | 35.8% |
| Vitamin B12 | 17 | 8.5% |
| Vitamin D | 120 | 59.7% |
| Vitamin E | 6 | 3.0% |
| Vitamin K | 3 | 1.5% |
| Calcium | 71 | 35.3% |
| Iron | 82 | 40.8% |
| Copper | 11 | 5.5% |
| Zinc | 16 | 8.0% |
| Albumin | 1 | 0.5% |
| Folic acid | 13 | 6.5% |
This cohort study shows that direct DS, with an alimentary limb length of 200 cm and a common limb length of 100 cm, is a safe and effective technique in the short and long term in patients with a BMI between 45 and 55 kg/m2.
According to the meta-analyses by Buchwald and Ding et al., DS is the bariatric surgery with the best medium- and long-term weight loss results, maintaining a %EWL greater than 70% and a %TWL around 36% and 46% after 5 and 10 years.10,11 Likewise, the randomized study and reviews by Hedberg et al., which compare the results of DS with gastric bypass, have shown the superiority of DS, mainly in patients with BMI > 48 kg/m212 and in BMI > 50 kg/m2.13 The main limitations of these studies are the heterogeneity of the study population and the type of DS. Most of the studies analyzed include the results of DS with different lengths of the biliopancreatic limb (70−100 cm) and total length (250−350 cm).14–18 In this context, it is important to highlight that, depending on the length of the loops and initial BMI, results can vary greatly. In terms of weight, the weight loss of our patients was relatively lower, probably due to the greater length of the total intestinal loop (300 cm) and higher mean initial BMI. Biertho carried out two randomized studies according to the length of the total loop.19,20 In the first, he compared the short and long DS (biliopancreatic limb 150 cm and 100 cm, with a common limb of 100 cm) and observed greater weight loss in the short DS at the expense of a greater need for supplementation of vitamin D, magnesium and copper.19,20 The second compared DS with a common limb of 200 cm and 100 cm, observing similar weight loss but greater weight regain in the DS with a long common limb.21 Depending on the patient’s initial BMI, weight loss is also different. The descriptive studies by Himpens14 and Fielding16 show that, in patients with a BMI < 50 kg/m2, the percentage of weight loss is higher than in patients with a BMI > 50 kg/m2 (90%–93% and 68%–70%, respectively).14,16
At the metabolic level, and in agreement with our cohort, both the review by Gagner, as well as the meta-analyses by Ding, Hedberg and the studies by Himpens14 and Gagner22 with a 10-year follow-up show remission rates for T2DM of 80.0%–87.5%, hypertension 80.9% and dyslipidemia 93.3%.11,13,14,22
With regards to serious postoperative complications, our series is similar to the Biertho study that included more than 1000 patients, in which he reports an overall rate of complications at <30 days of 5%, the most frequent of which was duodenal stump fistula (0.7%). Mortality in DS ranges from 0.2%–1.3%, which is also true in our cohort.23 Compared to other techniques, postoperative complications and mortality in DS are slightly higher than those of gastric bypass or sleeve gastrectomy.13 In the long term, the rate of revision surgery in our series is lower than in other cohorts, probably given the greater length of the total loop length and the smaller number of patients at 10 years. In studies with follow-up times of more than 10 years and a total loop length of 250 cm, the rate of long-term emergency surgery is 13.3%, mainly caused by internal hernia (6%), while revisional surgery is 2.9%, insufficient weight loss 1.3%, and malnutrition 1.4%.24,25
In parallel, the nutritional deficiency rate increases as the length of the common limb and total loop decreases.16,18 In DS, the most frequent deficiencies are fat-soluble vitamins, mainly vitamin A (20%–38%), D (28%–74%) and other nutrients such as iron (22%–40%) and zinc (17%–28%).17,25 Protein deficiency is the most feared complication of DS. In our series, the need for protein supplementation was 0.5%, and we had no cases of conversion due to malnutrition. It is important to differentiate hypoalbuminemia (which can be 2%–18% in the medium term) from severe protein malnutrition that requires revisional surgery.16,17,26 According to Topart’s descriptive study, the rate of revision surgery in DS due to malnutrition depends on the length of the common alimentary limb, which is 0.5% in patients with a common channel of 100 cm (as in our series) and 18% in patients with a 50-cm common limb.17 In recent years, the length of the total alimentary loop in the DS has been modified to minimize collateral nutritional effects. Depending on the adherence and type of multivitamin supplementation, the need for supplementation differs. In our study, the rate of need for extra supplementation was high. Topart emphasizes the need to increase the dosage of post-DS supplementation, mainly calcium, vitamin D, A and iron, and/or administer DS-specific multivitamins to decrease the need for supplementation due to nutritional deficiencies.17 Likewise, Gagner reports less of a need for extra supplementation (2%), in cases with the use of specific multivitamins and proper compliance with baseline supplementation and follow-up.7
Despite the good results, the DS technique represents less than 1.5% of the procedures performed worldwide. The complexity of the technique, together with the fear of complications arising from duodenal dissection, prevails among bariatric surgery teams. Certain measures have been described to simplify the technique. Our hospital has adapted the DS to the knowledge of the Whipple technique with pyloric preservation, performing the duodenal-ileal anastomosis with ligation of the right gastric and gastroepiploic artery. Marchesini described that this measure does not increase the risk of anastomotic dehiscence or fistula of the duodenal stump but favors performing the duodenal-ileal anastomosis without tension and can be a resource in patients with short mesentery or hepatomegaly.27 Cottam further simplifies the duodenal approach by describing ligation of the gastroepiploic artery as the only measure without the need for ligation of the right gastric artery.28
The main limitation of our study is the low number of patients followed for 10 years and the lack of analytical parameters to be able to describe in more detail the existence of nutritional deficiencies and the evolution of remission of comorbidities. Since our results demonstrate a need for supplementation in most of our patients at some point beyond two years and most series report a long-term rate of revision surgery higher than ours, we feel the need to expand the follow-up of our patients and emphasize the use of specific supplementation for hypoabsorptive surgery in patients with duodenal switch.
ConclusionsDirect DS, with an alimentary limb length of 200 cm and a common limb length of 100 cm, is a technique with a low rate of surgical complications in patients with a BMI between 45 and 55 kg/m2. In the medium and long term, weight loss is sustained with a low rate of revision surgery due to inadequate weight loss or weight regain. Likewise, DS has proven to be an effective technique at the metabolic level. Despite this, the need for nutritional supplements corresponds with the type of hypoabsorptive technique. Thus, the medium- and long-term follow-up of patients with DS must be guaranteed before selecting the technique.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sorribas M, Casajoana A, Sobrino L, Admella V, Osorio J, Pujol-Gebellí J. Experiencia en la derivación biliopancreática tipo cruce duodenal: resultados a 2, 5 y 10 años. Cir Esp. 2022;100:202–208.