The knowledge of the variations of the biliary tree (BT) is very important due to the increasing prevalence and complexity of the hepato-biliary surgery. The most frequent finding1 (60% of the cases) is the presence of a right hepatic duct (RHD) and a left hepatic duct (LHD) converging in a common hepatic duct (CHD). Therefore, in 40% of cases we can find anatomical variations that will be essential study before any hepato-biliary procedure.2 In up to 20% of the cases, we can find a posterior RHC that crosses the midline to drain in the LHC. This anatomical variation is very important when we are considering a left hepatectomy or a donor living surgery.3 The preoperative study of the biliary anatomy will be essential to avoid iatrogenic injuries, which repair could be highly complex, as in the present case.
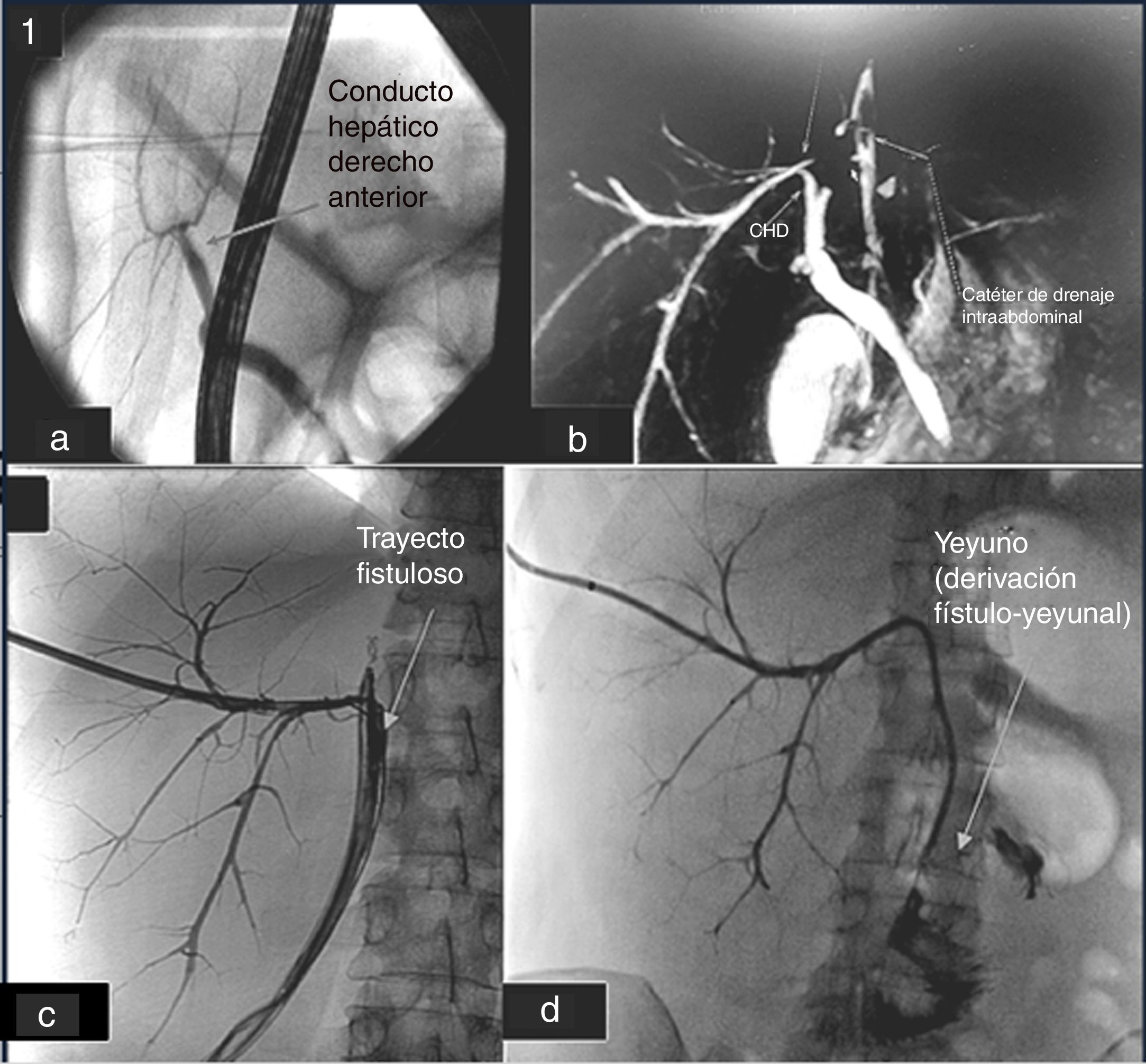
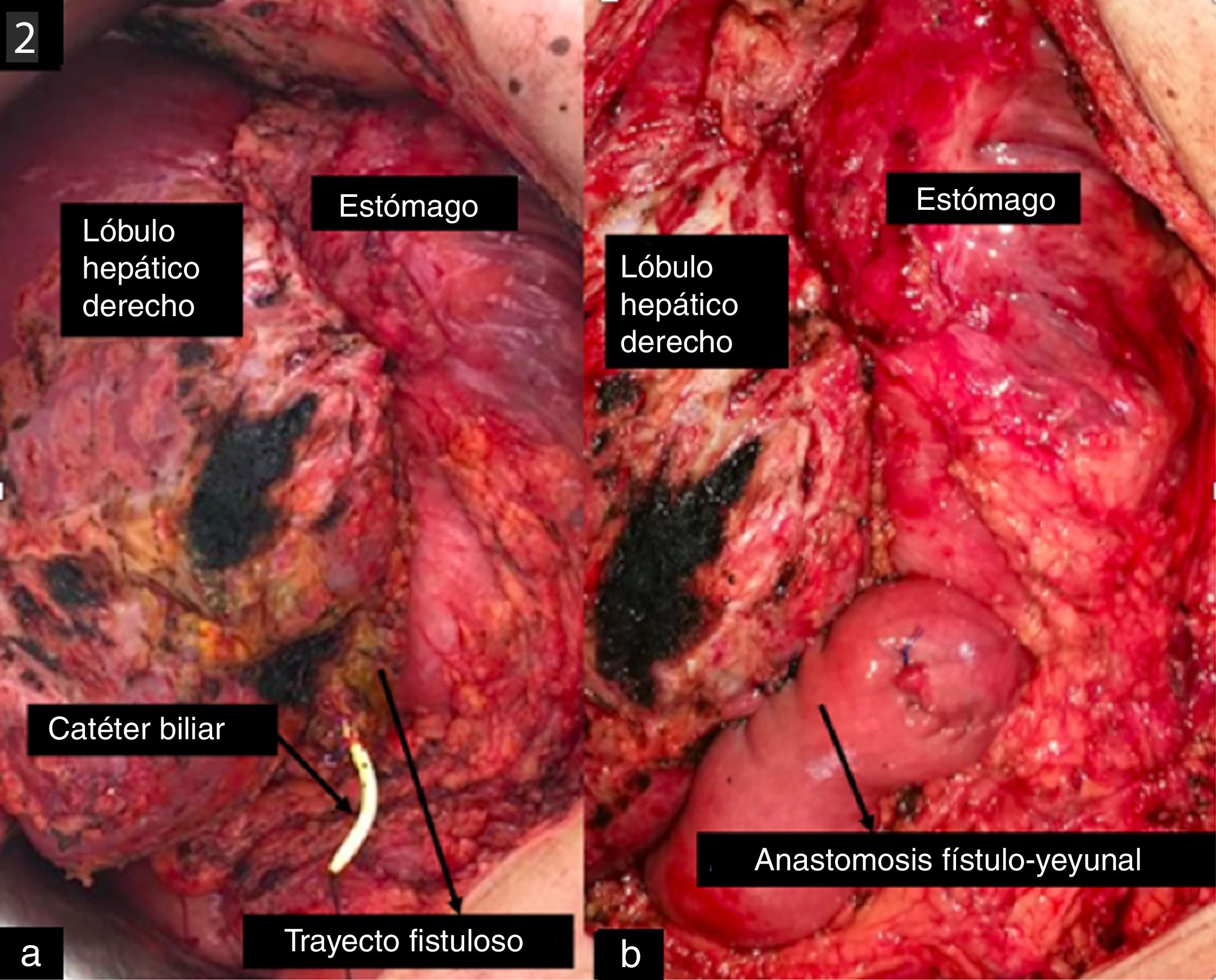
A 43-year-old woman, with intrahepatic cholangiocarcinoma, was proposed for a left hepatectomy with regional lymphadenectomy. The procedure was uneventfull and the histopathological study revealed a well-differentiated intrahepatic cholangiocarcinoma with free margins and 5 positive lymph nodes of the 15 analyzed (pT2bN1). In the preoperative study, no anatomical variations of the BT were described. During the first days, the patient developed a high volume biliary leak without any clinical worsening. An endoscopic retrograde cholangio-pancreatography (ERCP) was performed where we did not find contrast along the posterior RHD. The study was then completed with magnetic resonance (MR). A posterior RHD crossing the midline and drained into the hepatic margin was found. It drained directly in the area where the intra-abdominal drain was located (Fig. 1A). Initially, we proposed interventional treatment by radiological approach in an attempt to create an intrahepatic junction between the posterior RHD and the CHD, prior to consider surgical treatment. It was not possible, so an external biliary catheter was placed (Fig. 1B). After more than 3 months with the external biliary catheter, surgical treatment was proposed in order to try to perform an hepatico-jejunostomy. During the surgery, a fistulous tract was identified with the biliary catheter inside between the right hepatic lobe and the stomach. It had approximately 1 cm diameter and a thick wall of 2−3 mm. In order to avoid a deep dissection of the hepatic hilum, with high risk of new iatrogenic injuries, we decided to perform a Roux-Y hepatico-jejunostomy with the fistulous tract, leaving the biliary catheter along the anastomosis (Fig. 2B). The postoperative was uneventfull. A transcatheter cholangiography was performed (Fig. 2A) where we could identify good contrast flow from the intrahepatic duct to the jejunum without any leakage. Finally, both the intra-abdominal drain and the biliary catheter were removed.
a. CPRE preoperative study. It is not realice the CHDP. b. ColangioRMN posthepatectomy, with CHDP, who drained in to the leak. c. Cholangiography showing right posterior duct draining in the intra-abdominal drain with the biliary catheter inside. d. Cholangiography after perform the fistulo-jejunostomy.
The use of a well-consolidated fistulous tract for a biliary-digestive derivation is a good alternative for the treatment of complex biliary leaks.4 There are different therapeutic options. Firstly, we must consider the observation, because most of the biliary leaks disappear just with a good drain.5 The next step is interventional treatment by endoscopic and/or radiological approach.6 Several procedures can be considered such as: the embolization of the affected biliary duct, the creation of a new biliary tract (biliary-biliary, biliary-gastric or biliary-duodenal), the portal embolization of the parenchima that the leak drains, etc. In the last 5 years, the surgical treatment of complex biliary leak is becoming increasingly important. There are several studies describing an hepatico-jejunostomy with a fistulous tract,7 with good outcomes after short follow-up. The use of the fistulous path to perform the shunt is being proposed as the basis of alternative treatments in complex cases. In most bibliographic reviews they clarify the need to wait between 3 and 4 months7,8 for the formation of a consistent fistulous path that allows an anastomosis to be performed on it. It should be noted, given the prevalence of anatomical variants of BV, and the consequences that may result from lesions thereof,9 the need for a thorough and thorough preoperative study of the biliary tree, by radiologists and surgeons who are experts in the anatomy of VB,10 whenever major hepatobiliary surgery is to be performed.
In conclusion, the preoperative study of the BT anatomy is essential to avoid iatrogenic injuries of the bile duct. In the case of complex biliary leak, the surgical approach with an anastomosis between a fistulous tract and the jejunum, is an effective alternative to avoid a more complex dissection with higher risk of new iatrogenic injuries.
Please cite this article as: López de la Torre Molina B, Caso Maestro O, García Conde Delgado M, Manrique Municio A, Loinaz Segurola C. Fístulo-yeyunostomía como alternativa de tratamiento en la reparación de una fístula biliar compleja. Cir Esp. 2020;98:166–168.