Visceral aneurysms are relatively rare, but clinically they are relevant lesions that should be given consideration. The most common are splenic artery aneurysms (SAA), which represent about 60% of visceral aneurysms. Other more uncommon visceral locations are the hepatic artery (20%), superior mesenteric artery (5.5%), celiac trunk (4%), gastric and gastroepiploic arteries (4%), intestinal arteries (3%), pancreatic arteries (2%), gastroduodenal artery (1.5%) and very rarely in the inferior mesenteric artery (1%).1 In addition to their limited clinical presentation, visceral aneurysms are treated by cardiovascular surgeons, general surgeons, radiologists and angiologists; therefore, the overall experience of a team is never extensive and the experience of an individual surgeon may be very limited. The growing use of ultrasound and other imaging techniques has increased their detection, which is usually incidental.2,3
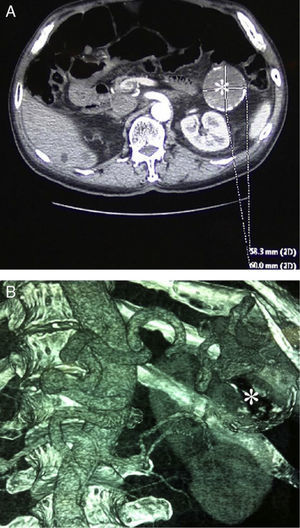
We present the case report of a 52-year-old male with diabetes, hypertension and acromegaly, who had undergone a transsphenoidal pituitary adenomectomy. He had severe aortic failure and ascending aortic aneurysms, and a calcified giant fusiform splenic aneurysm (58mm×60mm) was detected incidentally during computed tomography (CT, Fig. 1).
In spite of the patient's high risk profile, we decided to carry out standard surgery. This was due to the existence of numerous preoperative factors for failure of correct endovascular exclusion, such as the large size of the neck of the aneurysm as well as excessive tortuosity of the splenic artery.
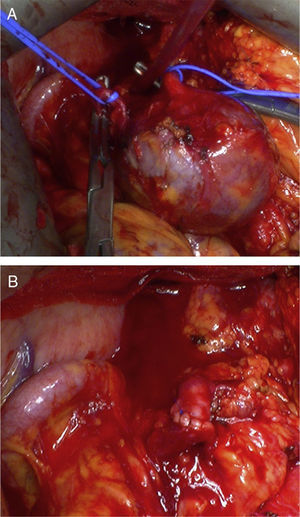
By means of a left subcostal laparotomy, the greater omentum was dissected using ligatures up to the omental sac and the aneurysm was located in the middle of the splenic artery, adjacent to the pancreas. After administering 1mg/kg of intravenous heparin and dissecting and clamping the proximal and distal ends of the splenic artery, aneurysmectomy was carried out with later direct revascularization by means of an end-to-end anastomosis with continuous 5.0 polypropylene sutures. The final result was good and there were no complications (Fig. 2). The patient was discharged on the 10th day post-op with normal platelet count (207000cm3) and normal CT angiography. Six months later, he remained asymptomatic, with a normal follow-up CT angiogram.
Currently, more asymptomatic incidental cases of visceral aneurysms are being reported due to the widespread use of ultrasound and CT as imaging tests.2,3 They can also be detected by means of radiography, generally seen as oval calcifications. SAA are usually saccular, located proximally in 5%, mid artery in 35% and distally in 60%. In 20% of the cases, multiple locations are found, so other locations should always be screened for aneurysms.1 Most cases are asymptomatic, with a risk of rupture between 2 and 46%, especially in pregnant women or patients with portal hypertension.4 The overall mortality for ruptured SAA is 25%–75%, while the mortality of standard surgery is 0.5%–1.5%.4,5 Generally, the classic indications of surgery are a size larger than 2cm, symptomatic SAA or in pregnant women or in those who desire to become pregnant (any size).6
There are several methods of treatment, such as open conventional surgery, laparoscopic surgery and intravascular interventionism, using either embolizations with coils or with covered stents. The choice depends on the location and accessibility of the SAA and the general status of the patient.7 Classic open surgery with laparotomy is a method with proven effectiveness,1–5 although it is relatively traumatic and presents morbidity. Laparoscopy is an excellent, less aggressive alternative, but it requires an expert surgeon.8 Percutaneous endoluminal treatment has the disadvantages of difficult stent placement or embolization if the splenic artery is tortuous and the probability of recurrence or incomplete aneurysm exclusion (endoleak). We consider surgical treatment, either open or preferably laparoscopic, the best therapeutic option in patients with reasonable surgical risk. Patients with very high surgical risk or contraindication to surgery can benefit from intravascular percutaneous treatment, with excellent results as well as low morbidity and mortality.7
Associated splenectomy was considered the most common therapy in the past,6 but it should be avoided to preserve the hemato-immunological function of the spleen, although in the case of distal SAA it is usually necessary with the aneurysmectomy. In the case of SAA of the middle or proximal thirds, aneurysmectomy is preferred in association with revascularization whenever feasible, either by means of direct reimplantation of the splenic artery as in the present case or by using venous grafts or prostheses. In spite of the rich collateral circulation in the spleen, there have been case reports of splenic infarction and abscessification in the absence of revascularization and, given its feasibility, we believe it should be indicated whenever possible. In some cases, especially inflammatory SAA, partial pancreatectomy may be associated depending on the location.
In conclusion, we believe that treatment should be individualized and that conventional surgery continues to be the gold standard, but the current growth of intravascular techniques and their low associated morbidity7 may make this situation revert in the near future, even though it is the first step in the treatment of high-risk patients with favorable anatomy.
Please cite this article as: Rodríguez-Caulo EA, Araji O, Miranda N, Téllez JC, Velázquez C. Aneurisma fusiforme gigante de arteria esplénica. Cir Esp. 2014;92:215–216.