Vascular leiomyosarcomas (VLMS) are uncommon1–5 and represent less than 2% of all sarcomas.2 They are usually seen in low-pressure vascular systems such as the vena cava. The least common locations are the veins of the lower extremities or the arterial system (pulmonary artery or periphery). In spite of being rare, it presents high rates of local recurrence and distant metastasis.6 Surgical resection is the treatment of choice and achieves acceptable long-term survival rates.1–3 We present the surgical treatment of a patient who presented liver metastasis of a saphenous vein leiomyosarcoma.
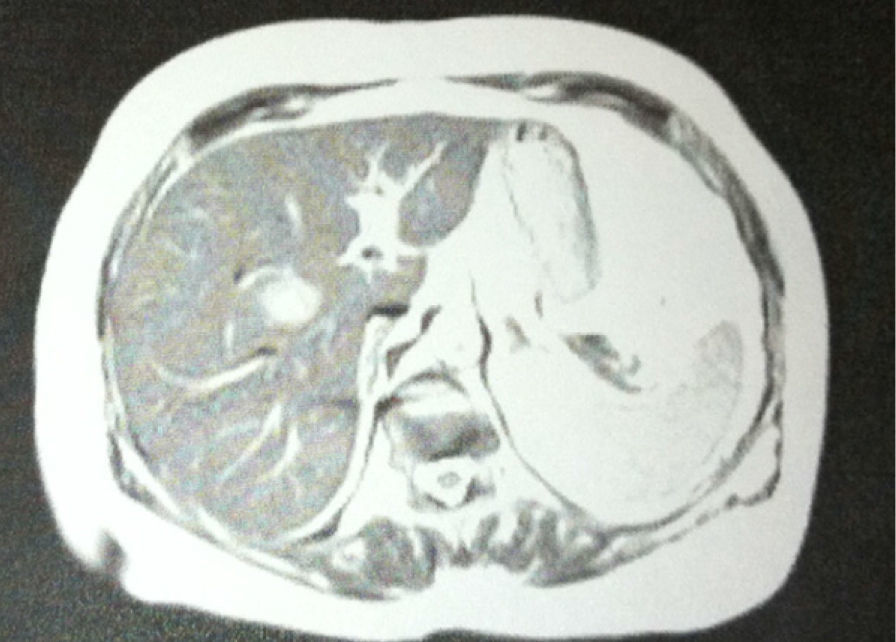
The patient is a 70-year-old woman who was surgically treated in January 2009 for a grade II leiomyosarcoma measuring 10cm in the right inguinal region. The tumor was removed and vascular resection performed, followed by adjuvant radiotherapy at a dosage of 66Gy in 40 sessions. In June 2010, a space-occupying lesion (SOL) was discovered in the liver that was consistent with metastasis. Abdominal computed tomography (CT) revealed a hepatic SOL that was approximately 15mm in the right liver lobe in close proximity to the portal bifurcation. Magnetic resonance (Fig. 1) showed an SOL measuring 26×28×23mm in segment VIII (hyperintense in sequences T2 and hypointense in sequences T1, with early peripheral enhancement and rapid central wash-out in the post-contrast study) and positron-emission tomography (PET) showed evidence of a hypermetabolic lesion measuring 3.2cm located in segment VIII (SUVmax: 6.6) (Fig. 2). With a diagnosis of metastasis of VLMS, she was sent to our hospital for scheduled surgery. During the procedure, a 3.5cm lesion was found resting on the portal bifurcation and proximal to the middle suprahepatic vein, and a right hepatectomy was performed. The pathology diagnosis was leiomyosarcoma metastasis with free margins. During post-op, the patient presented transient mild liver failure, which resolved with conservative treatment. She was discharged on the 8th day post-op.
Leiomyosarcomas are aggressive neoplasms with a very poor prognosis compared with other soft tissue sarcomas. The vascular origin has been identified as an adverse prognostic factor that reduces both disease-free survival as well as overall patient survival. In addition, they present a high potential for metastasis, probably because of their easy dissemination through the blood, the biological aggressiveness of these tumors, and their delayed diagnosis.4 The mean survival of patients with liver metastases of soft tissue sarcomas that go untreated is about 14 months, while the 5-year survival is 27%–35% after surgery.7,8 Out of the 27 cases of leiomyosarcoma of the saphenous vein described in the literature, including ours, 33% presented distant metastasis. Pulmonary involvement is the most frequent (22%) since the normal venous pathway drains through the inferior vena cava to the lung. Approximately 11% have been found in the liver (3 cases).
As for the diagnosis of these lesions, the efficacy of PET has yet to be defined, although it has shown promising results in other soft-tissue sarcomas. PET and PET-CT could be especially effective for evaluating patients with previous surgical treatment in order to search for local recurrences or metastases.9 In spite of the different therapeutic options that are currently available to us for the treatment of metastatic disease of other origins, in the case of VLMS metastases, neither systemic chemotherapy nor chemoembolization or radiofrequency has improved overall survival or disease-free survival.7,8 Only surgical resection has presented acceptable long-term survival rates at around 35% after 5 years.7,8
The liver is the organ that is most frequently affected by soft tissue sarcoma recurrence, with reports ranging from 59.4% to 93%.7,8 Nevertheless, recurrence rates clearly decrease in cases of R0 resections (21%), as seen in the series by Marudanayagam.7
These data support the argument that surgery should be considered the “gold standard” for initial treatment of hepatic/liver metastases as well as intrahepatic recurrences. Furthermore, perioperative mortality in these cases is lower than 5% in units specialized in hepatobiliopancreatic surgery.7
Please cite this article as: Prieto-Puga Arjona T, Sánchez Pérez B, Suárez Muñoz MÁ, Fernández Aguilar JL, Santoyo Santoyo J. Hepatectomía por metástasis de leiomiosarcoma de vena safena. Cir Esp. 2014;92:217–218.