Delayed gastric emptying (DGE) is a relatively common complication after cephalic pancreaticoduodenectomy (CPD). Its origin is not very clear, and it is believed that its appearance is due to multiple factors (hormones, appearance of other complications, particularly pancreatic fistulas, and the surgical technique). Among the technical aspects associated with DGE, it has been proposed that the route of gastroenteric reconstruction (antecolic or retrocolic) could have an effect on its incidence.
Materials and methodsA systemic review was made of the literature, searching for articles that compared both reconstruction routes after CPD, finding only 11 articles: 4 randomized clinical trials, one prospective study, and 6 retrospective studies. A meta-analysis could not be performed on them, due to the large methodological differences between them.
ResultsIn the 4 randomized studies, 2 were in favor of the antecolic route, and 2 did not observe any differences between either of them. The antecolic route obtained a much lower DGE rate than the retrocolic one in the only prospective study. In 4 of the retrospective studies the antecolic route obtained a very low rate. The results of both routes were similar in another 2 retrospective studies, with the retrocolic route slightly better in one of them.
ConclusionsUsing the published literature, the gastric reconstruction route associated with less DGE after CPD cannot currently be determined.
El retraso del vaciamiento gástrico (RVG) es una complicación relativamente frecuente tras duodenopancreatectomía cefálica (DPC). Su etiología no está aclarada y se considera que múltiples factores están relacionados con su aparición (hormonales, aparición de otras complicaciones especialmente la fístula pancreática,y de técnica quirúrgica). Entre los aspectos técnicos relacionados con el RVG se ha postulado que la ruta de reconstrucción gastroentérica (antecólica o retrocólica) pudiera modificar la incidencia de RVG.
Material y métodosHemos realizado una revisión sistemática de la literatura de los artículos que comparan ambas rutas de reconstrucción tras DPC, encontrando solo 11 artículos: 4 ensayos clínicos aleatorizados, un estudio prospectivo y 6 estudios retrospectivos. Las grandes diferencias metodológicas entre ellos no nos han permitido realizar un metaanálisis.
ResultadosEn los 4 estudios aleatorizados, 2 son favorables a la ruta antecólica y 2 no observan diferencias entre ambas. En el único estudio prospectivo, la ruta antecólica obtiene una tasa de RVG muy inferior a la retrocólica. En los estudios retrospectivos, en 4 de ellos la ruta antecólica obtiene una tasa de RVG muy inferior. En otros 2 estudios retrospectivos, los resultados entre ambas rutas son similares, en uno de ellos levemente mejores en la ruta retrocólica.
ConclusionesLa literatura publicada no permite actualmente determinar que la ruta de reconstrucción gastroentérica se relacione con un menor RVG tras DPC.
Delayed gastric emptying (DGE) is a frequent complication after pancreaticoduodenectomy (PD). Until 2007, when the International Study Group of Pancreatic Surgery (ISGPS) developed a structured 3-level classification according to the severity of DGE, there was no internationally accepted definition for delayed gastric emptying and its incidence varied greatly in the different series published.1–8
Although it does not present the severity of other post-PD complications such as pancreatic fistula or hemorrhage, DGE causes great discomfort to patients and increases hospital stays and costs.2–4,6,9–13
The etiology of DGE is not clear and many theories have been postulated.3–6,9–15 Some technical aspects of PD have also been associated with different rates of DGE (PD with/without pylorus preservation, Billroth I vs Billroth II, associated Braun enteroenterostomy, route of the gastrojejunal anastomosis [antecolic vs retrocolic], etc.).1,10
After PD, the gastroenteric reconstruction anastomosis had classically been retrocolic, but in recent years certain groups have used the antecolic route because certain advantages have been observed, such as a possible decrease in DGE.13,16
We have performed a systematic review of the literature to evaluate whether either of the gastroenteric reconstruction routes (antecolic vs retrocolic) causes less DGE.
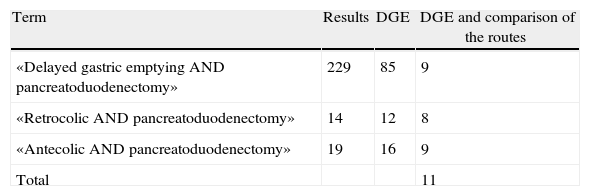
Materials and MethodsBibliographic Search; Data Analysis; Methodological Quality (Table 1)We performed a systematic search of the literature using the Pubmed database (January 1968–November 2012) in Spanish and English with different combinations of terms. The titles and abstracts of all the articles found were assessed. We selected those that referred to DGE and, out of these, those that compared the antecolic and retrocolic routes (Table 1).
In the search of the terms “antecolic pancreatoduodenectomy”, 19 articles were found, 16 of which reported DGE and 9 compared the 2 gastroenteric routes of reconstruction. In the search of the terms “retrocolic pancreatoduodenectomy”, 14 articles were found, 12 of which were dedicated to DGE and only 8 compared both routes. By using in the search the terms “delayed gastric emptying pancreatoduodenectomy” 229 articles were obtained, in 85 of which DGE was the main topic of the article. Out of these 85, only 9 articles dealt with gastroenteric reconstruction after PD and its relationship with DGE. We ruled out those articles that dealt with one of the 2 routes with no comparison with the other type. When the 3 searches were compared, there were only 11 articles that had not been repeated.
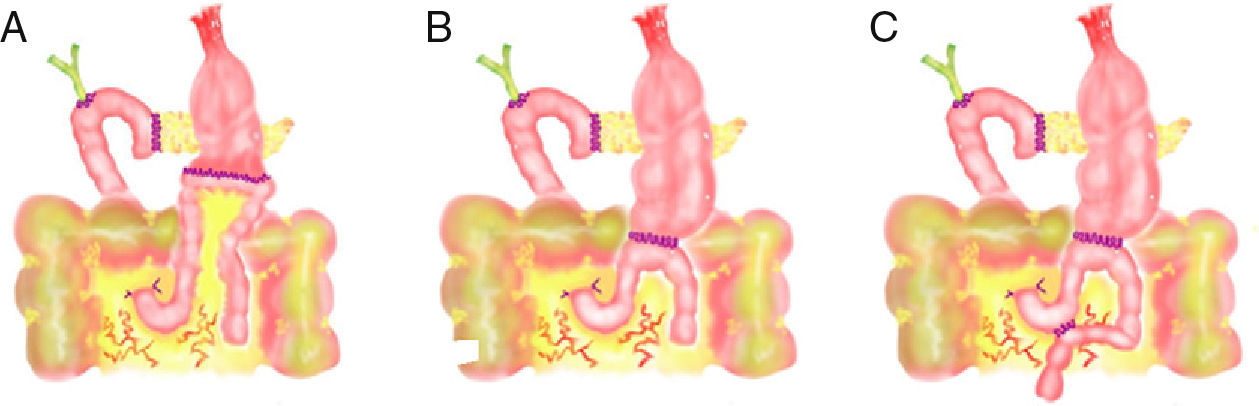
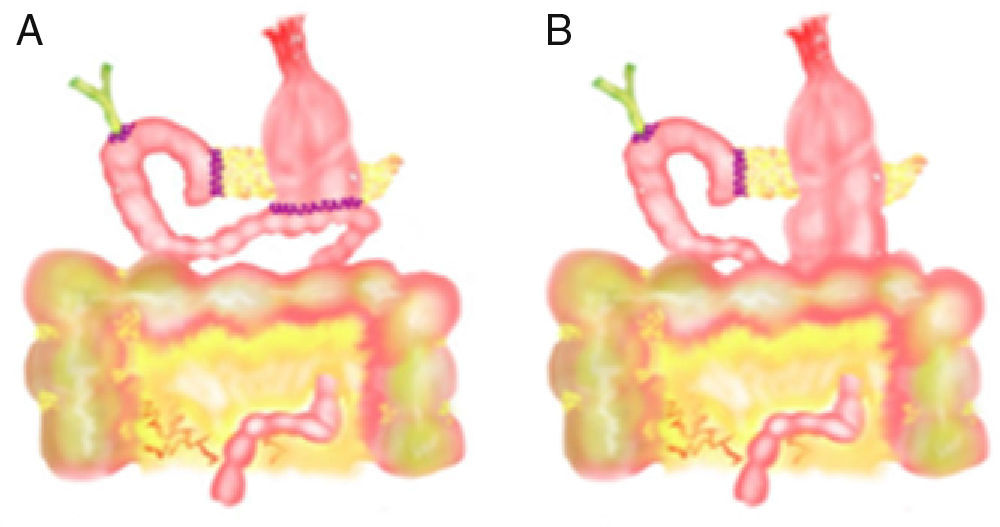
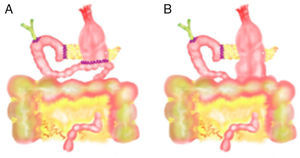
In the 11 articles, we studied the following variables: number of patients, study type (prospective, retrospective or randomized study), technical characteristics of PD, number of patients with antecolic (Fig. 1) and retrocolic (Fig. 2) methods, percentage of patients with PD with pylorus preservation, number of patients with DGE for each reconstruction type and number of patients with pancreatic fistula.
The 11 articles were: 4 randomized studies, a prospective study and 6 retrospective studies, on which we have based our review. We found no meta-analyses published on this subject.
In addition, to increase the amount of information provided we have used other articles related to DGE that we have selected from the mentioned search of the literature, even though they are not directly related with the comparison of reconstruction types.
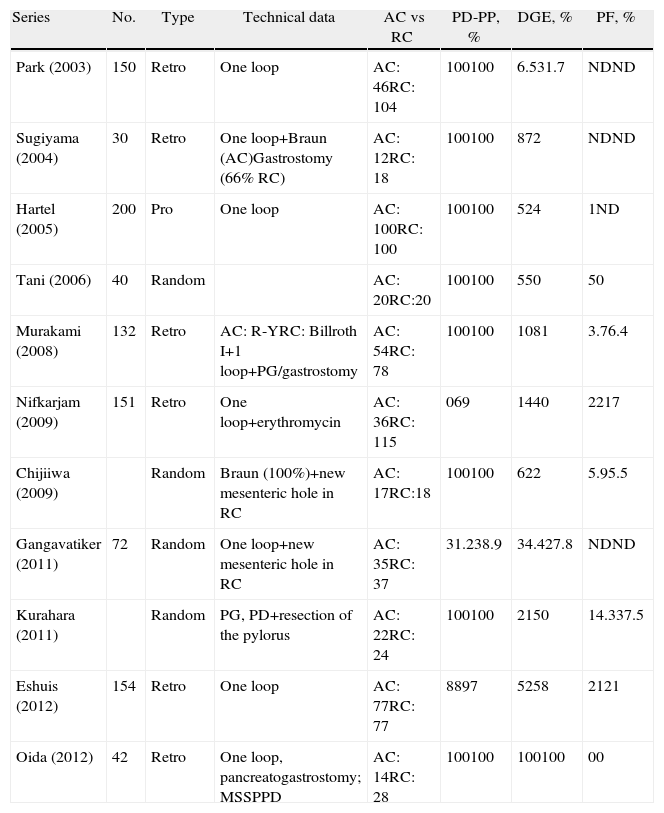
ResultsDue to the great differences between the series consulted, it was not feasible to combine all the results in a meta-analysis. The results would present multiple biases as the different gastric reconstruction methods, pancreatic anastomoses, postoperative diet regimes, prokinetic agents and antiemetics can affect DGE. Thus, we have chosen to summarize the articles studied in chronological order (Table 2).
Summary of the Published Series.
| Series | No. | Type | Technical data | AC vs RC | PD-PP, % | DGE, % | PF, % |
| Park (2003) | 150 | Retro | One loop | AC: 46RC: 104 | 100100 | 6.531.7 | NDND |
| Sugiyama (2004) | 30 | Retro | One loop+Braun (AC)Gastrostomy (66% RC) | AC: 12RC: 18 | 100100 | 872 | NDND |
| Hartel (2005) | 200 | Pro | One loop | AC: 100RC: 100 | 100100 | 524 | 1ND |
| Tani (2006) | 40 | Random | AC: 20RC:20 | 100100 | 550 | 50 | |
| Murakami (2008) | 132 | Retro | AC: R-YRC: Billroth I+1 loop+PG/gastrostomy | AC: 54RC: 78 | 100100 | 1081 | 3.76.4 |
| Nifkarjam (2009) | 151 | Retro | One loop+erythromycin | AC: 36RC: 115 | 069 | 1440 | 2217 |
| Chijiiwa (2009) | Random | Braun (100%)+new mesenteric hole in RC | AC: 17RC:18 | 100100 | 622 | 5.95.5 | |
| Gangavatiker (2011) | 72 | Random | One loop+new mesenteric hole in RC | AC: 35RC: 37 | 31.238.9 | 34.427.8 | NDND |
| Kurahara (2011) | Random | PG, PD+resection of the pylorus | AC: 22RC: 24 | 100100 | 2150 | 14.337.5 | |
| Eshuis (2012) | 154 | Retro | One loop | AC: 77RC: 77 | 8897 | 5258 | 2121 |
| Oida (2012) | 42 | Retro | One loop, pancreatogastrostomy; MSSPPD | AC: 14RC: 28 | 100100 | 100100 | 00 |
AC, antecolic; DGE, delayed gastric emptying; MSSPPD, modified subtotal stomachpreserving pancreaticoduodenectomy; PD-PP, pancreatoduodenectomy with pylorus preservation; PF, pancreatic fistula; PG, pancreatogastrostomy; Pro, prospective; Random, randomized; RC, retrocolic; Retro, retrospective.
Park et al. present a retrospective series of 150 PD. The overall DGE rate was 24%. The patients with retrocolic reconstruction presented more DGE (31.7% vs 6.5%), longer nasogastric drainage time and slower diet progression. The risk factors for DGE were the presence of preoperative cholangitis, the existence of intraabdominal complications and the retrocolic route of jejunal reconstruction.15
Sugiyama et al. present a retrospective series of 30 patients with PD and pylorus preservation (12 with antecolic anastomosis with Braun jejunojejunostomy vs 18 with retrocolic anastomosis). The rate of DGE was 8% when the anastomosis was antecolic and 72% in the retrocolic type. The patients with antecolic anastomosis presented fewer days of nasogastric suction, oral diet was introduced earlier and hospitalization was shorter.13
In a prospective, non-randomized study with a total of 200 patients (100 with antecolic and 100 with retrocolic anastomoses), Hartel et al. performed only pylorus-preserving PD. The patients with antecolic anastomosis had significantly shorter hospital stays, less intraoperative bleeding and fewer medical complications. The global rate of DGE in the series was 14.5%, but it was quite lower in the antecolic group (5% vs 24%). In the logistic regression analysis, the parameters associated with DGE were male sex and retrocolic reconstruction.12
Tani et al. carried out an RCT of 40 PD patients with pyloric preservation comparing the ante- and retrocolic routes (2 groups of 20). The overall incidence of DGE was 27.5%, but in the antecolic group it was 5% and in the retrocolic group it was 50%, with a statistically significant difference. The antecolic group presented, with a statistically significant difference, fewer days of postoperative SNG, less drained gastric volume, earlier tolerance to solid diet and shorter postoperative stay. There were no differences in the number of intraabdominal complications between both groups.9
Murakami et al., in their retrospective series of 132 patients, compared a Billroth 1-type retrocolic anastomosis with an antecolic gastrojejunal anastomosis. Both types were used in pylorus-preserving PD and pancreatogastrostomy. There was more blood loss and a greater number of complications in the retrocolic route. The incidence of DGE was higher in the retrocolic group vs the antecolic group (81% vs 10%). The reconstruction type, operating time and presence of postoperative complications were associated with DGE in the univariate analysis, but only the reconstruction type was associated in the multivariate analysis.11
Nifkarjam et al. presented a retrospective series of 151 PD (115 patients with classic retrocolic gastrojejunostomy and 36 with antecolic reconstruction and retrogastric omental patch). The group with antecolic reconstruction presented less DGE (14% vs 40%) and fewer hospital readmissions due to DGE (0% vs 17%). In the univariate analysis, the retrocolic anastomosis type was the only factor that was statistically associated with DGE. Male patients with cancer and classic PD have a non-significant higher tendency toward having less DGE. All patients received post-op erythromycin.6
Chijiiwa et al. carried out a randomized study with 35 patients (17 with antecolic and 18 with retrocolic reconstruction). On the 30th day post-op, the subjects ingested food marked with acetate 13C to determine the DGE. The postoperative DGE rate was 6% in the antecolic route and 22% in the retrocolic route, but the difference between the two routes was not statistically significant. There were no significant differences between the two routes in the studies with acetate 13C. One month after the PD, 80% of the patients had a gastric emptying similar to that before surgery.16
Gangavatiker et al. completed a randomized study that compared the two routes. Diabetic patients and those over the age of 70 were excluded due to their greater probability for DGE. Erythromycin was prescribed systematically. The overall incidence of DGE was 31%, with no differences according to the route used (34% in the antecolic group and 27.8% in the retrocolic group). Furthermore, the severity of DGE was not different when the two routes were compared. In the univariate analysis, age, use of octreotide and the presence of intraabdominal complications were risk factors for DGE; in the multivariate analysis, only age was a risk factor for DGE.2
Kurahara et al. published a randomized study with 46 patients: 24 with antecolic reconstruction and 22 with retrocolic reconstruction. The technique used was a PD with preserving subtotal gastrectomy, with pyloric ring resection only, and pancreatogastrostomy. The incidence of DGE was significantly higher in the retrocolic (50%) vs the antecolic (20.8%) group. In addition, the retrocolic group presented more severe DGE (more grades B and C). The retrocolic group required more days of NG tube, more days before proper tolerance of oral intake and longer hospital stays.17
Eshuis et al. retrospectively compared 2 groups of 77 patients with antecolic and retrocolic reconstruction. They observed no differences in DGE between the two groups, although in so-called “primary DGE” (not brought on by a secondary cause), the antecolic type presented a significantly lower rate of DGE (20% vs 36%).4
Oida et al. compared the antecolic and retrocolic routes after their own PD technique with pyloric resection and gastric preservation in 42 patients. All the patients presented some degree of DGE. The patients with retrocolic reconstruction resumed oral intake of solid foods earlier and none had grade C DGE.14
DiscussionIn patients with periampullary tumors, PD is the only treatment that offers the possibility of a cure and, when feasible, it is the treatment of choice.2,4,7,16 Mortality in PD has been drastically reduced in recent years, and in specialized centers the current rate is about 5%.1–5,7 The morbidity associated with this procedure, however, continues to be high, ranging from 30% to 60%.1–7,16,17 The most frequent complications are pancreatic fistula, postoperative hemorrhage and DGE.2,4,5,7,9,11
Previously, the incidence of DGE reported in the literature was very variable due to the lack of an internationally-accepted definition and the existence of several classifications.1,4,16 In 2007, the International Study Group of Pancreatic Surgery published a specific definition for DGE that consists of the inability to eat a normal diet 7 days post-PD or the prolonged use of a nasogastric tube or the need for reintroducing the NG tube, including 3 levels of severity (A, B and C).4,8,12 Despite this definition, the published incidence of DGE after PD is still variable in recent series.2,4,5,12
DGE produces discomfort in patients, prolongs hospital stays, increases costs and may even cause severe complications such as pneumonia or aspiration.2–4,6,9–13,15–17 The standard treatment for DGE is conservative and includes the administration of erythromycin and reintroduction of the nasogastric tube.6,9,11,12,15
The etiology of DGE has not been clarified, although it is thought to be multifactorial.2,4,6,9,12–14 The most widely accepted theories are changes in neurohormonal mechanisms after duodenojejunal resection (decreased motilin and cholecystokinin) and DGE caused by other intraabdominal complications (pancreatic fistula being the most common). Some authors call this type of DGE secondary.1,2,4,6,11,12 Other postulated etiologies are: postoperative pancreatitis, antropyloric ischemia, edema of the anastomosis, gastric denervation, pyloric spasm, diabetes mellitus, angulation or torsion of the gastrojejunal reconstruction, compromised vascular function of the jejunal loop, lymphadenectomy close to the celiac trunk due to possible damage on the vagal nerve branches, etc.1,3–6,9,11–14,16
Certain technical aspects of PD have also been related with DGE: the classic Whipple or pylorus preservation, Billroth I vs II, enterostomy, type of suture, jejunostomy and enteral nutrition, a new buttonhole in the mesentery, or route of gastroenteric reconstruction.18,19
Patients with antral resection after a classic Whipple procedure who underwent pylorus preservation seem to present similar DGE rates. Although initially some articles seemed to conclude that pyloric preservation was associated with higher DGE, this has not been later confirmed in other studies and systematic reviews.1,3,6,7,10–13,15,20–22 Goei et al. observed higher DGE in patients with Billroth's operation I (76%) vs Billroth II (32%) in a retrospective study in 2 centers.1 A Braun enteroenterostomy associated with antecolic reconstruction seems to perhaps lower DGE.5,23 A retrospective study has correlated suture type with DGE incidence, observing that it is lower in patients with mechanical anastomoses than in manual anastomoses, and among these it is lower in single-layer than in double-layer anastomoses.24 The placement of the retrocolic anastomosis in the inframesocolic space seems to diminish DGE.10 Contradictory information has been published about the use of enteral nutrition through a jejunostomy and the rate of DGE.25
There is no evidence of whether any of the possible types of gastroenteric reconstruction (antecolic or retrocolic) after PD reduces or prevents DGE.6 The supposed rate of DGE in the antecolic route is said to be 15% and 30% for retrocolic.16 Classically, after PD, gastrojejunal or duodenojejunal anastomoses were done by the retrocolic route, but in recent years the antecolic type has been becoming more popular.4 The theoretical advantages of antecolic gastrojejunal or duodenojejunal anastomoses are: greater distance from the pancreatic anastomosis, diminished possible venous congestion in the retromesenteric region of the afferent loop, minimized possible jejunal angulation or kinking, and the emptying by gravity is simpler and provides greater mobility of the stomach and jejunum.4,6,13
Although the literature about DGE is extensive, there are few articles that compare antecolic and retrocolic reconstruction in PD and the DGE results obtained with the two techniques. Our bibliographic search identified only 4 EA, one prospective study and 6 retrospective studies. The series comparing the two routes are presented in Table 1 in chronological order.
The series are difficult to compare because the multiple parameters that can influence DGE are different: (a) technical, such as the use of Roux-en-Y, Billroth I vs Billroth II reconstruction, separate window for the retrocolic method or not, Whipple or pyloric preservation, one or 2 loops, gastrostomy, enteroenterostomy (Braun) or exteriorization of pancreatic fluids; (b) DGE definition, classic vs International Study Group of Pancreatic Surgery; (c) dietary protocol (very different between western and oriental countries), use of NG tube, days of NG tube, fast-track protocols, systematic use of erythromycin and technique for reintroducing oral intake; and (d) existence of intraabdominal complications that could be related with DGE. In addition, in the studies analyzed, most patients underwent PD with pyloric preservation, so there is therefore practically no information as to whether there are differences in DGE depending on the route of gastroenteroanastomosis in patients with a classic Whipple procedure.
The information that we currently have available can be summarized as:
- 1.
Randomized studies: of the 4 randomized studies, 2 favor the antecolic route and another 2 observe no statistically significant differences between the two routes.2,9,16,17
- 2.
Prospective study: the antecolic route presented a DGE rate that is lower than the retrocolic approach.12
- 3.
Retrospective studies: in 4, the antecolic route obtained a rate of DGE that was quite lower. In another 2 retrospective studies, the results between the two routes were similar, and in one of them the results were slightly better in the retrocolic route.4,6,11,13–15
In conclusion, we currently cannot affirm that either of the 2 routes for reconstruction (antecolic vs retrocolic) is able to lower DGE rates, although the antecolic route does seem to be associated with a lower DGE. In order to determine which technique is optimal, a well-structured randomized study with a defined technique and common postoperative management would be necessary, while using the classification of the ISGPS for DGE. In addition, a very high number of patients would be required since the direct association between the presence of locoregional complications, which are very frequent after PD, and DGE could result in biased results.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ramia JM, De la Plaza R, Quiñones JE, Veguillas P, Adel F, García-Parreño J. Ruta de reconstrucción gastroentérica tras duodenopancreatectomía: antecólica versus retrocólica. Cir Esp. 2013;91:211–216.