Amyloidosis is a generic term that refers to a group of diseases characterized by extracellular deposits of amyloid material. The variety of symptoms caused by amyloidosis makes the diagnosis of the disease difficult and delayed. Gastrointestinal involvement is common, but the appearance of massive hemorrhage is rare and difficult to diagnose and treat. The deposit of amyloid material in the digestive tract is basically located in the mucosa and submucosa, as well as in the muscularis propria and blood vessel walls, which can cause gastrointestinal symptoms to be very heterogenous.
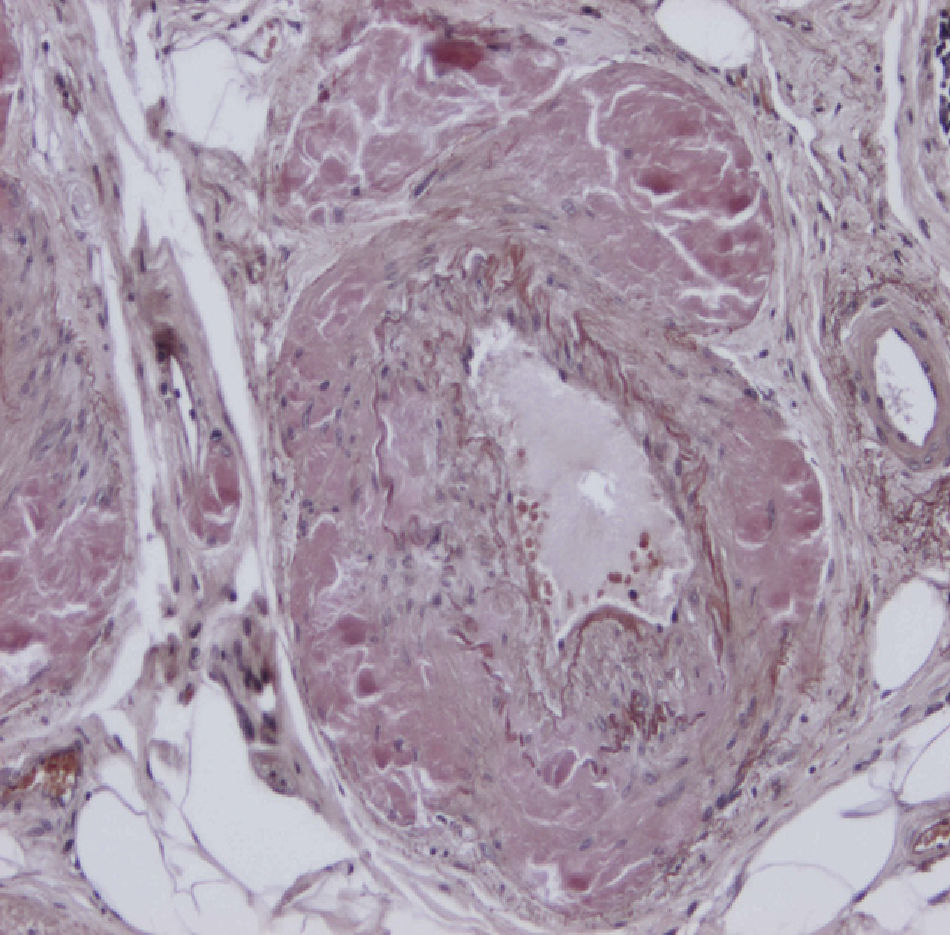
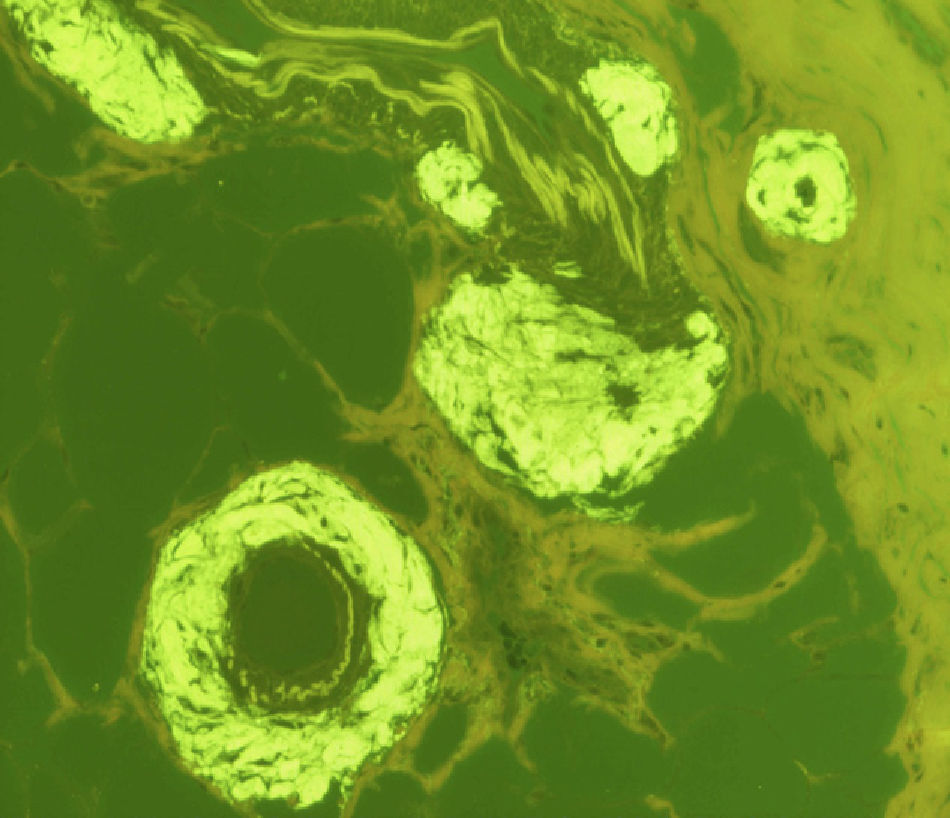
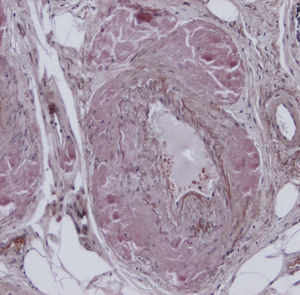
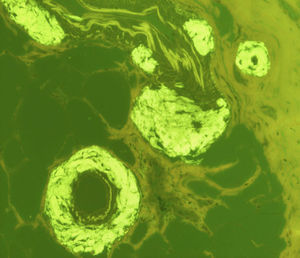
We present a 75-year-old patient with no prior medical history who was admitted to our hospital due to bloody stools over the course of the previous 2 days, with no other associated symptoms. The patient was shown to be very anemic, requiring massive transfusion and urgent endoscopy, which revealed evidence of bleeding in the proximal jejunum, although the origin was not able to be located with CT angiography or arteriography. Exploratory laparotomy demonstrated a 20-cm jejunal segment that was fibrotic in consistency and purple in color. The intestinal loop was opened, where active capillary bleeding was observed in the congested jejunal mucosa; 40cm of the jejunum was removed, and a manual end-to-end anastomosis was performed. The pathology study with Congo red and thioflavin staining of the surgical specimen provided the diagnosis of amyloidosis of the jejunum (Figs. 1 and 2).
The patient presented no extraintestinal manifestations associated with amyloidosis or any other symptoms of secondary amyloidosis. Blood analyses ruled out macroglobulinemia and rheumatoid factor, and the quantification of immunoglobulin was negative. Bone marrow aspiration ruled out the presence of multiple myeloma. The amyloidosis study was completed with a proteinuria study, and the presence of kappa and lambda light chains was ruled out.
Amyloidosis is defined as a group of diseases whose main characteristic is extracellular amyloid material deposits. Amyloidosis is divided into 6 groups: primary, secondary, hemodialysis-related, hereditary, senile and local or organ-specific.1,2
In systemic amyloidosis, intestinal involvement is frequent and can occur in 60%–90% of cases, although gastrointestinal involvement alone is an exceptional finding. In published cases, the small bowel is the most frequently affected region. This involvement can be diffuse or, less commonly, focal. There have been few cases reported in the medical literature of focal amyloidomas of the duodenum and jejunum without extraintestinal manifestations.1,3
Focal amyloidomas are infiltrations of the entire thickness of the intestinal wall. This involves the destruction of the mucosa, deep infiltration of the muscularis propria and narrowing of the blood vessel lumen, typically presenting as multiple polypoid lesions or pseudotumors of the small intestine, causing a great disparity in symptoms.4
The most common signs are diarrhea and malabsorption syndrome. The vascular fragility caused by amyloid deposits in the blood vessel walls can lead to episodes of gastrointestinal bleeding. Another theory holds that progressive intestinal ischemia due to vascular compromise would cause necrotic ulcerations with consequent bleeding. There have also been case reports of intestinal motility disorders with dysphagia, pseudoobstruction, perforation and intestinal infarction.5,6
Patterns found in barium-contrast radiological studies (such as computed tomography) in amyloidosis of the gastrointestinal tract are not specific. The suspicious signs on endoscopy are fine granularity of the small bowel together with erosions or polypoid protrusions. On biopsy, amyloid deposits are observed in the blood vessel walls and in the muscularis mucosae, showing green birefringence with polarized light after staining with Congo red.7,8
Given the lack of specificity together with its subclinical nature, gastrointestinal amyloidosis is usually diagnosed in advanced stages. It is commonly diagnosed during intestinal motility disorder studies or in the presence of an intestinal malabsorption syndrome, which involve gastrointestinal endoscopy and biopsies with pathology confirmation. The definitive treatment of focal gastrointestinal amyloidosis would be surgical resection of the affected segment.9,10
In short, focal amyloidosis of the bowel is a rare pathology that is difficult to diagnose due to variable symptoms. Surgery is indicated in cases of obstruction and hemorrhage, which leads to cure as it is a localized disease found only in the resected bowel segment.
Please cite this article as: Garay M, Bollo J, Balague C, Targarona E, Trias M. Hemorragia digestiva como primer síntoma de una amiloidosis yeyunal focal. Cir Esp. 2014;92:696–698.