Schwannomas are benign neurogenic tumors derived from the Schwann cells that produce myelin sheaths around axons. These types of tumors are found in the peripheral or cranial nerves and are very rare in the digestive tract or in the retroperitoneal region.1 Only 10 cases have been published in the literature about lymph node schwannomas, which are extremely rare, located in different anatomical regions.2–7
We present a case of suprarenal lymph node schwannoma. The patient is a 42-year-old woman with an asymptomatic retroperitoneal mass that was found during a study for arterial hypertension, with no other medical history of interest. After suprarenal hormone profiling, which was normal, imaging tests were done. Abdominal computed tomography (CT) with contrast demonstrated a heterogeneous mass with decreased uptake in the right suprarenal area that was approximately 5cm in diameter with hyper-intense edges as well as some subcentimeter adjacent lymphadenopathies (Fig. 1). We also observed 2 hyper-intense liver lesions with solid characteristics located in each liver lobe, the largest measuring 1.5cm in diameter. In order to study these liver lesions in greater detail, abdominal MRI was ordered, which cataloged the lesions as angiomas. With the diagnosis of non-functioning right suprarenal mass, laparoscopic adrenalectomy was performed for diagnosis and treatment. The postoperative period was free of complications, and the patient was discharged 48h after surgery.
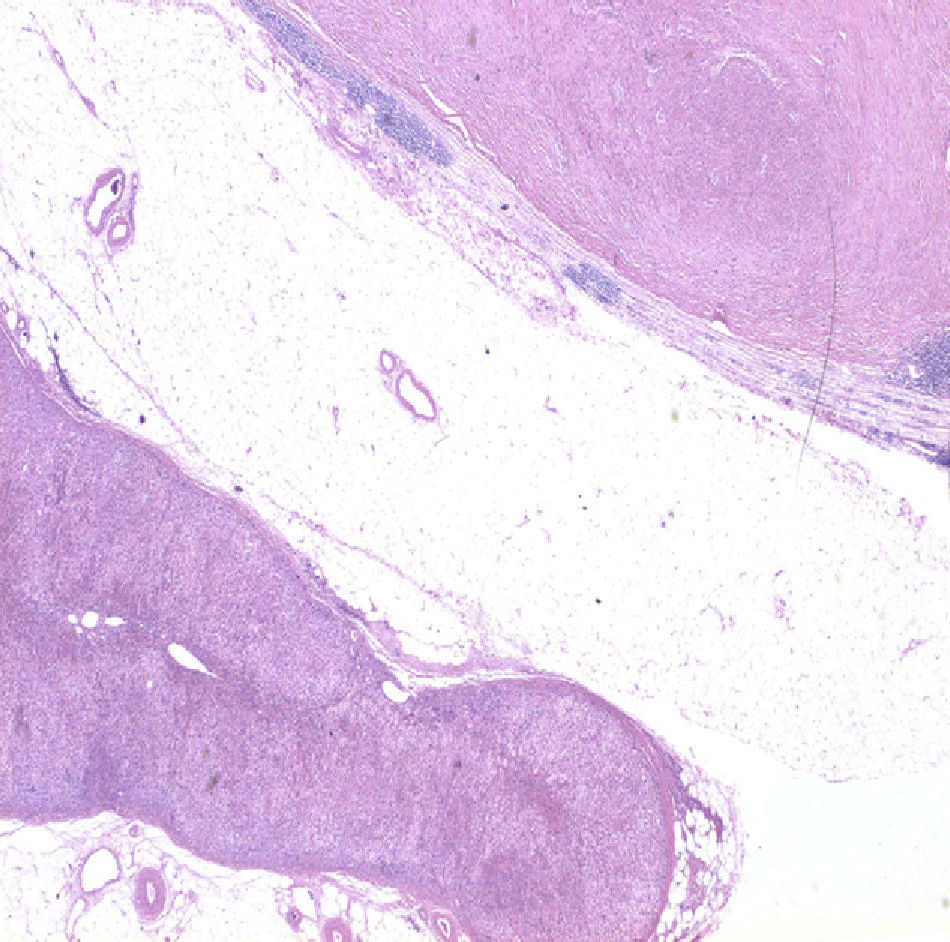
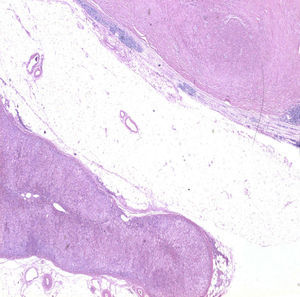
The surgical specimen from the adrenalectomy measured 8cm×5cm×4.5cm and included the suprarenal gland, with no significant histologic alterations, and a solid nodular lesion measuring 37mm. This was closely adhered and it turned out to be a lymph node infiltrated by a mesenchymal proliferation with histologic characteristics and positive S100 immunophenotype (Fig. 2). The histologic diagnosis was suprarenal lymph node schwannoma type Antoni A.
Schwannomas are benign tumors that originate from well-differentiated Schwann neoplastic cells. They are usually encapsulated, well-defined, clear and brilliant in appearance when observed macroscopically.3 They have a benign clinical behavior, with progressive growth and no local or systemic invasion; they are usually asymptomatic, so diagnosis is incidental in most cases. Schwannomas are rarely malignant and, if this does occur, they are usually associated with von Recklinghausen syndrome or some other type of neurofibromatosis.1 Microscopically, schwannomas are divided into 2 subtypes: Antoni A, which is hypercellular with limited stroma and presenting Verocay bodies (small groups of fibers surrounded by nuclear palisades); and Antoni B, which presents limited cellularity and a larger amount of stroma, considered a degenerated form of the Antoni A type. Immunohistology studies play an essential role in the diagnosis and in this type of tumors they are positive for S100 (family of low-molecular weight proteins present in the cells derived from the neural crest) and vimentin (protein found in the cytoskeleton of mesenchymal cells).2,3,8
As for the treatment of suprarenal tumors, surgery is indicated in functioning tumors, in masses with radiological suspicion for malignancy (regardless of size) and in tumors larger than 4cm, as in our case. Size is the most important criterion for the indication for surgery in non-functioning tumors. Laparoscopic removal is the technique of choice due to its limited postoperative morbidity and the existence of adequate planes outlining the mass.1,4,9,10
In our case, the lymph node location of the schwannoma was not able to be identified before the histopathology study since, on the imaging techniques as well as macroscopically after the removal of the specimen, it formed part of a mass that was integrated with the suprarenal gland.
In conclusion, suprarenal lymph node schwannomas are uncommon neoplasms, although they should be taken into consideration in the differential diagnosis of retroperitoneal masses.
Please cite this article as: Hernández Domínguez S, Mugüerza Huguet JM, Díez Alonso MM, González Estecha A. Schwanoma intranodal de localización suprarrenal. Cir Esp. 2014;92:695–696.
This article is original and was presented as a poster at the Meeting of the National Association of Spanish Surgeons held in November, 2011 in Pamplona (Navarra, Spain).