When we receive a polytraumatized patient at our emergency service, we must assure permeability of the airway, spontaneous breathing, cardiovascular stability, neurologic situation and perform a complete physical examination. For the correct haemodynamic management of these patients we commonly need to place one or more central venous catheters, which may be located at jugular, femoral or subclavian veins.1 The femoral venous catheterization is an easy technique, especially for emergent situations, uncooperative patients or who present breathing difficulties. Complication rates of central venous catheters vary from 15 to 33%, being the most frequent ones: catheter malposition, arterial puncture, haemorrhage, haemothorax and pneumothorax, deep vein thrombosis, infections, and arteriovenous fistula.2 It is important, as well, the measurement of intraabdominal pressure (IAP) to discard the presence of intraabdominal hypertension (IAH, defined as an IAP ≥ 12mmHg), and try to avoid the development of a compartment abdominal syndrome, which would be defined as a sustained IAP higher than 20mmHg associated with new organ dysfunction.3 Some publications support that IAH duration is an independent predictor of 60-day mortality in critically ill patients, so every effort to reduce the IAP as soon as possible should be done.4 When managing trauma patients, it is required to know the whole medical history and the circumstances in which injuries have occurred. In the context of an abdominal trauma, the imaging test of choice is an intravenous contrast enhanced computed tomography (CT) as long as the patient is hemodynamically stable,5 since it constitutes a non-invasive technique with a great sensibility and specificity.
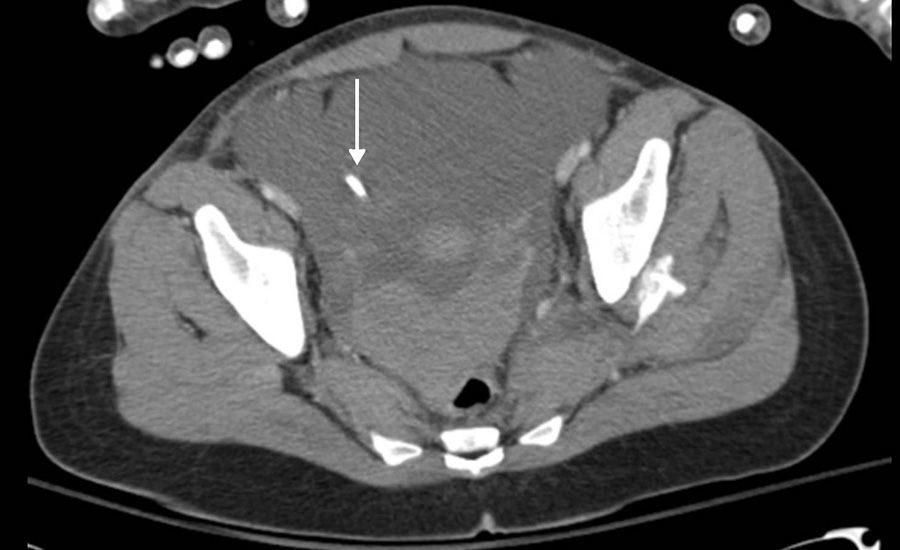
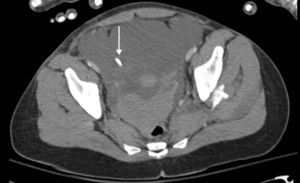
A 23 year-old woman, with no clinical history of interest, suffered a polytrauma secondary to a road traffic accident. In her reference hospital, 2 central venous catheters (right subclavian and femoral) were placed for haemodynamic monitoring and transfusion of 6 packed red blood cells. Once she was stabilized, a body CT was performed, revealing bilateral pleural effusion, fracture of the left acetabulum with posterior dislocation of the femoral head, liver laceration of 9×7cm in the right hepatic lobe (grade IV of the AAST liver injury scale), and intraperitoneal free fluid compatible with hemoperitoneum. The patient was transferred to our centre, which is a regional reference for hepatic surgery, presenting important abdominal distention, signs of peritoneal irritation, and an IAP of 35mmHg. A new body CT was requested, which showed the previously known injuries and a greater amount of hemoperitoneum, without visualizing active contrast extravasation [Fig. 1]. Cross-section images and tridimensional reconstruction from CT demonstrated the presence of the femoral venous catheter in a free intraperitoneal location, without contacting with femoral artery or vein [Fig. 2]. In the intensive care unit, we proceeded to aspirate through the femoral catheter, obtaining several litres of hematic content, which resulted in lowering the IAP and disappearance of the IAH status. Given our patient's haemodynamic stability and the lack of active source of bleeding, we decided a conservative attitude, with satisfactory evolution.
Central venous catheters (CVC) are used both in emergency as in scheduled situations, its location is usually aided by the use of ultrasounds, circumstance which may be absent during the management of a shocked patient. Although CVC insertion is a common procedure, it is not exempt of presenting complications. After contacting with the primary hospital where the femoral catheter was placed, they used Seldinger technique without employing ultrasound. They aspirated dark blood, so it was assumed that the central line was correctly located along the femoral vein, whilst they were actually obtaining intraperitoneal free blood which was coming from liver laceration. Although femoral venous catheterization looks to be a safe procedure during initial trauma resuscitation even in the absence of ultrasound, malposition of this catheter may carry severe complications, such as the one our patient suffered.6 In regard to hepatic trauma management, a non-operative management (NOM) should be performed in hemodynamically stable patients, without penetrating abdominal wounds, and in the absence of an active source of bleeding or other abdominal injuries in CT.7 Failure rates, following this approach, range from 10% to 20%.8 Anyway, nowadays, lots of hepatic vascular lesions may be initially managed with interventional radiologic procedures, what allows avoiding a major surgical procedure.9 Free intraperitoneal location of a femoral venous catheter is an outstanding complication which has barely been described in literature.10 In this case, transfusion of packed red blood cells through this catheter contributed to increase the amount of hemoperitoneum and to develop IAH in our patient. Tridimensional reconstruction from CT was essential to visualize the presence of the femoral venous catheter within the peritoneal cavity and to ensure the origin of the hemoperitoneum, what avoided a major surgery procedure.
Please cite this article as: Bailón-Cuadrado M, Barrera-Rebollo A, Sarmentero-Prieto JC, Rodríguez-López M, Blanco-Álvarez JI. Hemoperitoneo y síndrome compartimental abdominal por catéter venoso femoral intraperitoneal. Cir Esp. 2016;94:487–488.