Breast cancer is responsible for approximately 10 million cancer diagnoses in both sexes, and it is the leading cause of death in women worldwide.1 Lobular carcinoma of the breast has a greater capacity to metastasize than other subtypes, even at a clinically undetectable size.2 We present a case in which histopathological findings secondary to the resection of a peritoneal implant instigated the search for the primary breast tumor.
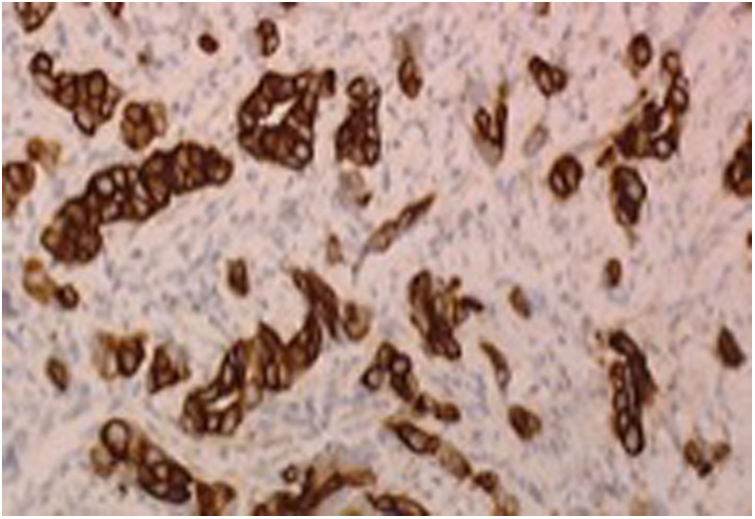
The patient is a 35-year-old woman, with no personal history of interest, who came to the emergency department with generalized abdominal pain and vomiting over the previous 72 h. Physical examination revealed abdominal distension with generalized pain upon palpation, with no other findings. Lab workup revealed a slight increase in acute-phase reactants (APR). Urgent abdominal computed tomography (CT) demonstrated significant dilation of the small bowel loops with a change in caliber in the region of the distal ileum. During urgent exploratory laparotomy, we found evidence of distal ileal stenosis caused by fibrous nodules that gave the impression of being tumor implants, finding no other lesions in the abdominal cavity. Right hemicolectomy was performed with jejunotransverse anastomosis. The postoperative progress was favorable, and that patient was discharged from hospital on the 7th postoperative day. The pathology results revealed the existence of multiple nodular formations that were miliary in appearance, compatible with poorly differentiated invasive lobular carcinoma of the breast. The immunophenotype was positive for cytokeratin 7 (Fig. 1) and negative for cytokeratin 20, c-kit (CD117), TTF1 and ALC (CD45). Positive estrogen receptors expressed in 100%; progesterone negative and HER2 negative.
After these findings, a complete breast study was carried out. During physical examination, a palpable breast nodule measuring 30 mm was identified in the upper outer quadrant of the left breast, with a clinically positive axilla. Protocolized imaging studies (mammography, breast and axillary ultrasound and magnetic resonance imaging) confirmed an infiltrating lobular carcinoma with immunohistochemical characteristics similar to the laparotomy findings. The extension study was negative. The patient was assessed by the tumor committee, which decided to perform a lumpectomy with axillary lymphadenectomy. The definitive pathology results identified an infiltrating lobular carcinoma measuring 20 mm with 100% estrogen receptor positivity, negative progesterone, Ki-67 > 14% and negative HER2. Axillary lymphadenectomy study found 16 affected nodes out of the 16 resected: stage pT1cN3a (16/16) M1. Given these results, the patient initiated treatment with paclitaxel, bevacizumab and megestrol acetate, then changing to bevacizumab alone after the fourth cycle due to poor tolerance. After one year of treatment and disease stability, bevacizumab was suspended, and quarterly goserelin and tamoxifen were administered.
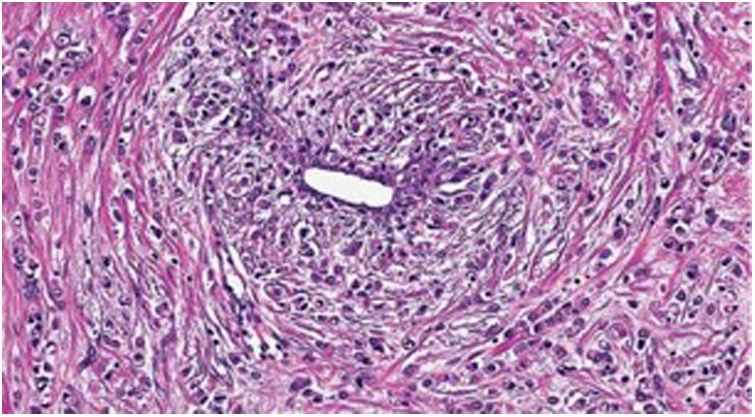
After 6 years of disease stability, the patient reported a newly emerging nodule adjacent to the breast scar. A complete bilateral breast study revealed a 15 mm nodule adjacent to the surgical scar of the left breast, with biopsy showing infiltrating lobular carcinoma (pleomorphic variant with signet ring cells), 100% positivity for hormone receptors (estrogen and progesterone) and negative HER2 (Fig. 2). Architectural distortion was also visible on magnetic resonance imaging scan of the contralateral breast, and biopsy results identified infiltrating lobular carcinoma with immunohistochemistry similar to the contralateral lesion. Right axilla was negative; extension study (body-CT and PET/CT) was negative. After the case was presented to the tumor committee, bilateral mastectomy was performed with right axillary SLNB (which was negative) and bilateral reconstruction with breast expanders. The definitive pathology results reported an infiltrating lobular carcinoma in the right breast measuring 0.9 cm with hormone receptors 100% for estrogen and 40% for progesterone, Ki-67 < 14%, HER2 negative. In the left breast, infiltrating lobular carcinoma measuring 1.6 cm was identified with 100% positivity for hormone receptors (estrogen and progesterone), Ki-67 > 14% and HER2 negative. The patient subsequently began adjuvant treatment with anthracyclines and taxanes, radiotherapy and hormone therapy. She is currently disease-free and pending definitive breast reconstruction (second stage of expander-prosthesis).
Solitary metastases in the gastrointestinal tract due to breast cancer are very rare.2 In 2005, McLemore et al.3 published a series of cases where 32% of the patients had metastases in the gastrointestinal tract, with no evidence of peritoneal carcinomatosis (i.e. resectable3), similar to the case presented.
Given the finding, single intestinal metastases should be resected if possible, as they improve the survival of patients compared to those managed with conservative treatment (hormone therapy) in cases of patients with a previous history of breast cancer.4
The survival of patients with stage IV breast cancer appears to be 12–24 months after starting treatment. However, there is a small group of stage IV patients in whom survivals of up to 20 years after diagnosis have been described.5 These patients are disease-free for a long period of time, are premenopausal, have a HER2-negative primary tumor and are oligometastatic.6 To date, the survival of the patient described in this case report has been 10 years, and she continues to be disease-free.
Please cite this article as: Gómez-Sánchez T, Ayllón Gámez S, Pacheco García JM. Obstrucción intestinal secundaria a metástasis de cáncer de mama no diagnosticado. Cir Esp. 2020;98:104–105.