Diaphragmatic plication is the most accepted treatment for symptomatic diaphragmatic hernia in adults. The fact that this pathology is infrequent and this procedure not been widespread means that this is an exceptional technique in our field.
To estimate its use in the literature, we carried out a review in English and Spanish, to which we added our series. We found only 6 series that contribute 59 video-assisted mini-thoractomy for diaphragmatic plications in adults, and none in Spanish. Our series will be the second largest with 18 cases.
Finally, we conducted a survey in all the Spanish Thoracic Surgery units in Spain: none reported more than 10 cases operated by thoracoscopy in the last 8 years (except our series) and most continue employing thoracotomy as the main approach.
We believe that many patients with symptomatic diaphragmatic hernia could benefit from the use of such techniques.
La plicatura diafragmática es el tratamiento más aceptado para la eventración diafragmática sintomática en adultos. La infrecuencia de esta dolencia y la escasa difusión de este procedimiento hacen que esta técnica sea excepcional en nuestro medio. Para estimar la difusión en la literatura, realizamos una revisión estructurada en lenguas inglesa y castellana a la que sumamos nuestra casuística: encontramos solo 6 series que aportan un total de 59 plicaturas diafragmáticas en adultos asistidas por toracoscopia. Ninguna en castellano. Nuestra serie sería la segunda mayor: 18 casos, con resultados satisfactorios similares a los publicados.
Finalmente efectuamos una encuesta a todos los servicios españoles de cirugía torácica: ninguno tiene más de 10 casos operados por toracoscopia en los últimos 8 años (a excepción del nuestro) y la mayoría continúa utilizando la toracotomía como abordaje.
En nuestra opinión muchos pacientes con eventración diafragmática sintomática podrían beneficiarse con la difusión de estas técnicas.
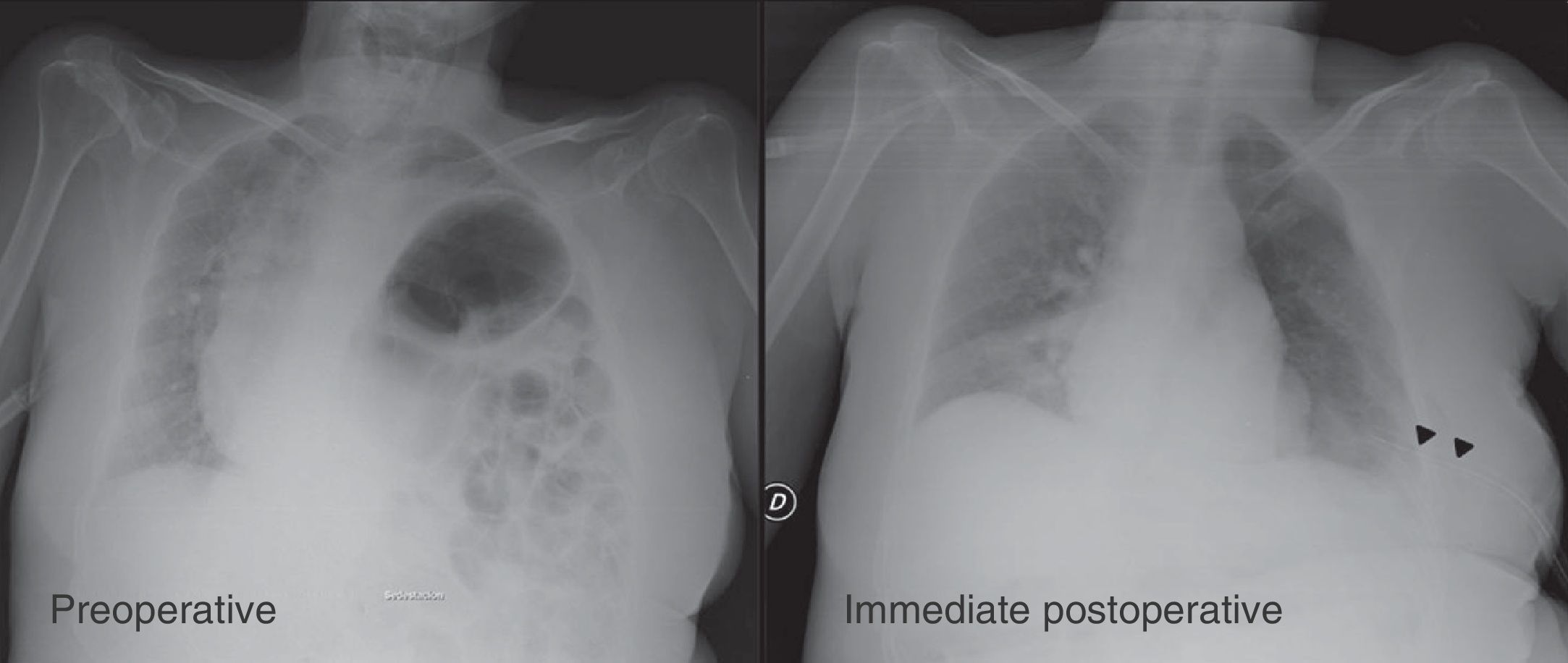
Diaphragmatic hernia (DH) is defined as the abnormal and permanent lifting of part or all of the diaphragm without defects in continuity (Fig. 1).1–3 Depending on the origin, it may be congenital or acquired (the latter is also called diaphragmatic or phrenic palsy).
The posterior–anterior X-ray image for preoperative and immediate postoperative diaphragmatic plication (60-year-old patient with a history of polio, tetraparesis, and left symptomatic diaphragmatic hernia). Note the mediastinal shift, and the compression of both lungs and the opposite hemidiaphragm due to hernia of the left hemidiaphragm. The arrows indicate postoperative pleural drainage.
Although uncommon, it is more prevalent in the pediatric population, where it causes acute symptoms that can turn into severe respiratory failure.4–6 By contrast, few cases in adults have shown symptoms (progressive dyspnea, orthopnea, recurrent pneumonia, palpitations or dyspepsia).4,7–10
The true incidence of this disease is difficult to estimate and often underestimated, due to the existence of asymptomatic or symptomatic cases that have not been treated surgically.1,4,7,11 The most accepted surgical treatment for symptomatic cases is to perform folds in the diaphragm to achieve its descent and appropriate tension, a technique known as diaphragmatic plication (DP) (Fig. 1).
Decades ago, good functional results of this procedure were overshadowed by the consequences of the approach by thoracotomy or laparotomy, which led to this surgery gradually falling into disuse.1,7 With the advent of endoscopic techniques, these methods gradually regained their acceptance and indication.1,7 At present, although there are few publications and few cases in the literature, DP with minimally invasive techniques is considered the treatment of choice; it is safe and effective for correcting clinical and spirometric defects secondary to DH.1,8,12 However, many surgeons are unaware of this unusual procedure; some even continue using thoracotomy (as performed for over half a century), without incorporating the practical benefits of minimally invasive surgery.13,14 These latter observations, also mentioned by other authors, seem to fit the reality in Spain.
Objectives- 1.
To identify, in English and Spanish scientific literature, publications concerning the video-thoracoscopy-assisted DP, highlighting those in Spanish groups.
- 2.
To assess the degree of dissemination and use of DP by video-assisted minithoracotomy by health personnel, mainly at national and local level.
This work consists of a structured narrative review and a national survey on DP in adults.
Initially, we conducted a review of the literature on video-assisted thoracoscopy DP in adults, consulting 11 databases (08/11/2012); our cases (18 cases) were also added. We attempted to refine the search, excluding papers focusing on pediatric patients and those in languages other than English or Spanish. No limits were set for year of publication. The following search engines were used:
Medline:
- –
*Diaphragm surgery [Majr] and crossed with diaphragmatic plicat*. The search was limited to anyone older than 13 years of age (20 papers were obtained).
- –
Diaphragm* surgery [MeSH] and crossed with diaphragmatic plicat*. The search was limited to anyone older than 13 years of age (29 papers were obtained).
- –
Respiratory paralysis [MeSH] OR diaphragmatic eventration [MeSH] AND diaphragmatic plicat*. The search was limited to anyone older than 13 years of age. (40 papers were obtained).
EMBASE:
- –
diaphragm* plicat* AND adult* NOT child* OR infant* OR newborn* OR pediatr* (75 papers were obtained).
IBECS (Spanish Bibliographic Index on Health Sciences):
- –
Plicat* diafragm*. The search was limited to anyone older than 13 years of age (0 papers were obtained).
IME (Spanish Medical Index):
- –
Plication AND diafragm* (4 papers were obtained).
Cochrane:
- –
Plication diafragm*. The search was limited to anyone older than 13 years of age (0 papers were obtained).
Trip Database:
- –
Diaphragm* AND plicat* [anywhere]. The search was limited to anyone older than 13 years of age (44 papers were obtained).
- –
SciELO (Scientific Electronic Library Online):
- –
Plicat* diafragm*. [Method: integrated]. The search was limited to anyone older than 13 years of age (3 records were obtained).
VHL (Virtual Health Library):
- –
Plicat* diafragm*. The search was limited by selecting: human, adult, middle-aged and elderly (14 papers were obtained).
Up to date:
- –
Diaphragm* plicat* AND adult* NOT child* OR infant* OR newborn* OR pediatr*.
WOK (web of knowledge):
- –
Diaphragm* plicat* AND adult* NOT child* OR infant* OR newborn* OR pediatr* Refined by: Research Areas: SURGERY (53 papers were obtained).
Google Scholar:
- –
Diaphragm plicature plication. Without the words: pediat* – child* – infant* – nin* (20 papers were obtained).
- –
Diafragm* plicat*. Without the words: pediat* – child* – infant* – nin* (19 papers were obtained).
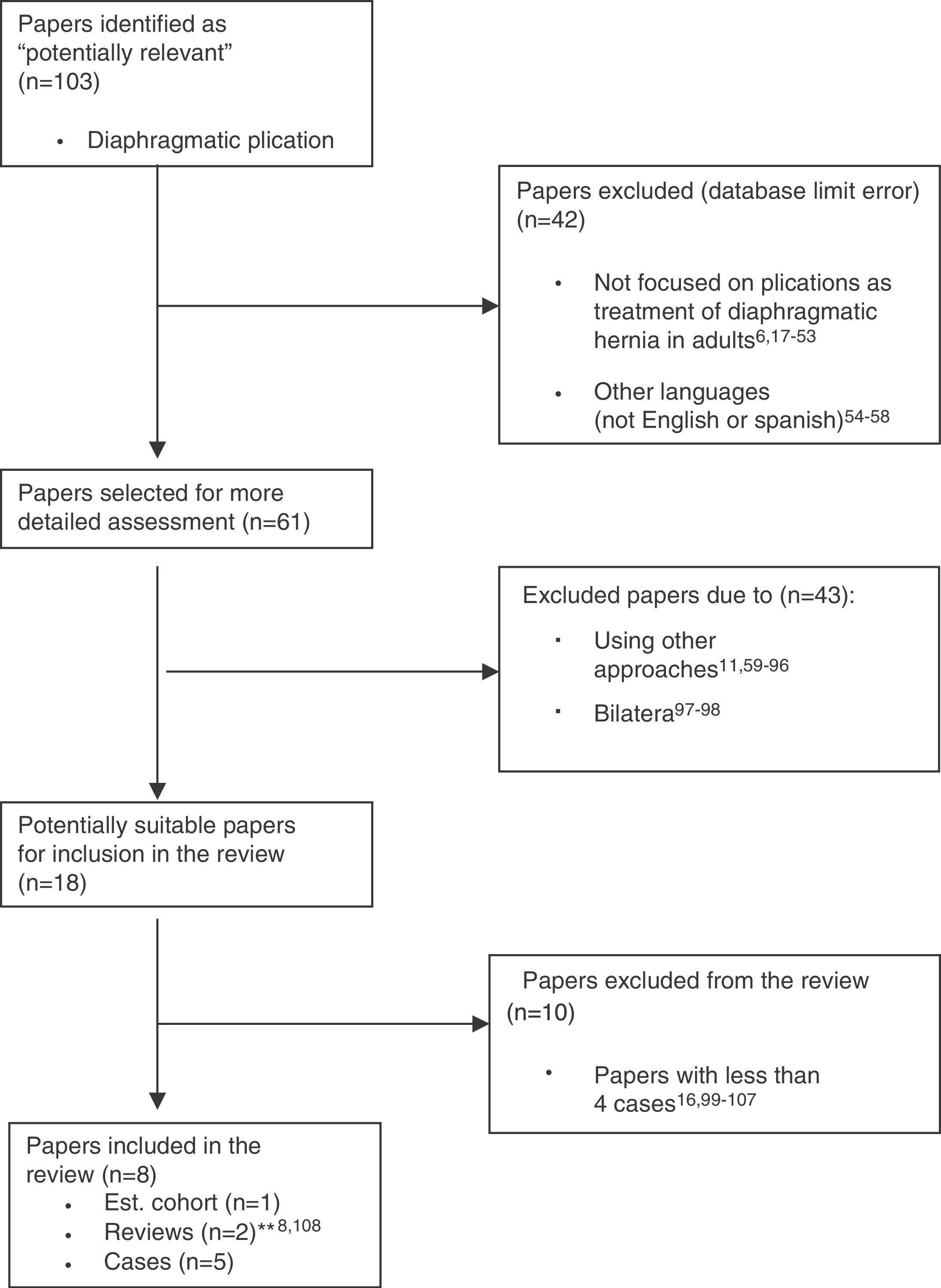
By following the recommendations suggested by QUOROM,15 all papers obtained from the various databases were reviewed, and repeats removed, to form a set entitled: “Potentially Relevant Papers.” Subsequently, we excluded those not in English or Spanish, those dealing exclusively with pediatric populations (database filter failures), and those not focused on DP as a treatment for hernia or paralysis of the diaphragm in adults. All the others were used to form the set entitled: “Selected Papers for Further Review.” From this group, we separated all papers focusing on DP performed by a non-thoracoscopic-assisted approach with minimal invasive surgical techniques or treating bilateral diaphragmatic hernias or paralysis to form the set entitled: “Papers Potentially Suitable for Inclusion.” Finally, we excluded from the review those publications with less than 4 clinical cases (Fig. 2).
Flow 17–107 diagram of the selection of papers in the literature review: “unilateral diaphragmatic plication in adults with minimally invasive thoracoscopy-assisted techniques.” Based on the “QUOROM” scheme for meta-analyses and systematic reviews of clinical trials.15,a Cited revisions do not provide the author's own cases.
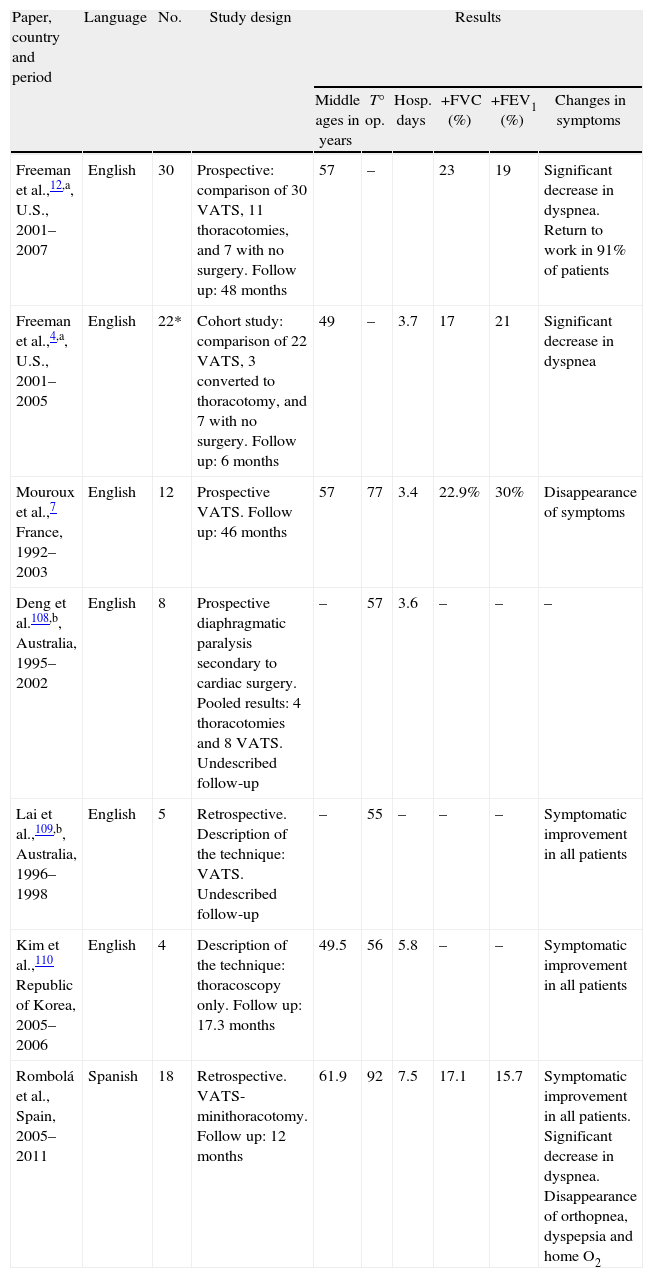
The “Included in the Review” papers were grouped according to the type of publication (Table 1), highlighting the level of evidence according to the U.S. Agency for Health Research and Quality.
Description of Main Perioperative, Spirometry and Symptom Variables in the Published Papers for Diaphragmatic Plication With Minimally Invasive Thoracoscopy-Assisted Techniques for the Treatment of Diaphragmatic Hernia in Adults.
| Paper, country and period | Language | No. | Study design | Results | |||||
| Middle ages in years | T° op. | Hosp. days | +FVC (%) | +FEV1 (%) | Changes in symptoms | ||||
| Freeman et al.,12,a, U.S., 2001–2007 | English | 30 | Prospective: comparison of 30 VATS, 11 thoracotomies, and 7 with no surgery. Follow up: 48 months | 57 | – | 23 | 19 | Significant decrease in dyspnea. Return to work in 91% of patients | |
| Freeman et al.,4,a, U.S., 2001–2005 | English | 22* | Cohort study: comparison of 22 VATS, 3 converted to thoracotomy, and 7 with no surgery. Follow up: 6 months | 49 | – | 3.7 | 17 | 21 | Significant decrease in dyspnea |
| Mouroux et al.,7 France, 1992–2003 | English | 12 | Prospective VATS. Follow up: 46 months | 57 | 77 | 3.4 | 22.9% | 30% | Disappearance of symptoms |
| Deng et al.108,b, Australia, 1995–2002 | English | 8 | Prospective diaphragmatic paralysis secondary to cardiac surgery. Pooled results: 4 thoracotomies and 8 VATS. Undescribed follow-up | – | 57 | 3.6 | – | – | – |
| Lai et al.,109,b, Australia, 1996–1998 | English | 5 | Retrospective. Description of the technique: VATS. Undescribed follow-up | – | 55 | – | – | – | Symptomatic improvement in all patients |
| Kim et al.,110 Republic of Korea, 2005–2006 | English | 4 | Description of the technique: thoracoscopy only. Follow up: 17.3 months | 49.5 | 56 | 5.8 | – | – | Symptomatic improvement in all patients |
| Rombolá et al., Spain, 2005–2011 | Spanish | 18 | Retrospective. VATS-minithoracotomy. Follow up: 12 months | 61.9 | 92 | 7.5 | 17.1 | 15.7 | Symptomatic improvement in all patients. Significant decrease in dyspnea. Disappearance of orthopnea, dyspepsia and home O2 |
–: provides no information.
Hosp. days: days of hospitalization. +FEV1: average increase in the relative value of forced expiratory volume in 1s; +FVC: average increase in the relative value of forced vital capacity; No.: number of patients in the series; Home O2: home oxygen therapy requirements; T° Op.: average surgery time.
a,b Publications from the same hospital.
Subsequently, in all publications, we collected the epidemiological variables assessed in our study: age and time from diagnosis to assessment by thoracic surgery; perioperative: duration of surgery and days of hospital stay; clinical: comparison of dyspnea, orthopnea, dyspepsia and respiratory oxygen requirements for preoperatively, postoperatively and spirometric variables: comparison of functional residual volume (FVC) and forced expiratory volume in the first second (FEV1) of our series. We compared these variables using a table with publications from other authors on techniques similar to ours. All our patients underwent surgery by DP with the technique described by Mouroux with minimal modifications1,7,16: through an incision smaller than 4cm in the lateral region of the affected hemithorax and using thoracoscopic control to perform 4 continuous invaginating sutures of the diaphragm from their costal insertions to the mediastinum, achieving adequate diaphragm reduction and tension.
Finally, we conducted a brief survey of all thoracic surgery departments in Spain, aiming to find the approximate DP experience accumulated by the different sites in the last 8 years. The following questions were addressed:
- –
What experience does your center have in treating symptomatic diaphragmatic hernias in adults over the last 8 years? Indicate the number and the technique used. Respondents were asked to select one of the following options: (a) none; (b) less than 5 cases; (c) between 5 and 10 cases; (d) between 10 and 20 cases and (e) more than 20 cases.
- –
Why do you think that these surgical treatments are indicated so infrequently? State your opinion about the indication for DP as treatment for DH. Respondents were asked to select one of the following options: (a) it is an uncommon condition and rarely symptomatic; (b) surgery is not appropriate treatment; (c) due to the poor results of surgery; (d) lack of knowledge of the medical community for surgical treatment and results. Few cases referred to the thoracic surgeon; (e) high rate of comorbidity and poor respiratory function tests of affected patients; and (f) other reasons.
Answers were collected over 3 months (May, June and July 2012).
ResultsThe literature review yielded the following results:
- –
Medline: 89 papers
- –
EMBASE: 50 papers
- –
IBECS: 0 papers
- –
IME: 4 papers
- –
Cochrane: 0 papers
- –
Trip Database: 44 papers
- –
SciELO: 3 papers
- –
VHL: 14 papers
- –
Up To Date: 2 papers
- –
WOK: 43 papers
- –
Google Scholar: 39 papers
After removing duplicate papers in the various searches, we obtained 103 “Potentially Relevant Papers” that were progressively excluded, based on proposed criteria (Fig. 2.); 6 papers were left yielding series greater than 4 cases, with a total of 59 patients (Table 1). No publications were found in Spanish or from Spanish centers.
Table 1 shows the publication type, the number of cases in each series, and the main pre and postoperative variables. The same table includes results relevant to our study. We did not find any randomized controlled trials or meta-analyses. All publications correspond to a series of cases with a IV level of evidence.
In our cases, the mean time from the radiological diagnosis of symptomatic DH and consultation to thoracic surgery was 59.27 months, with a standard deviation of 82.59 months, and a range of 6–301 months.
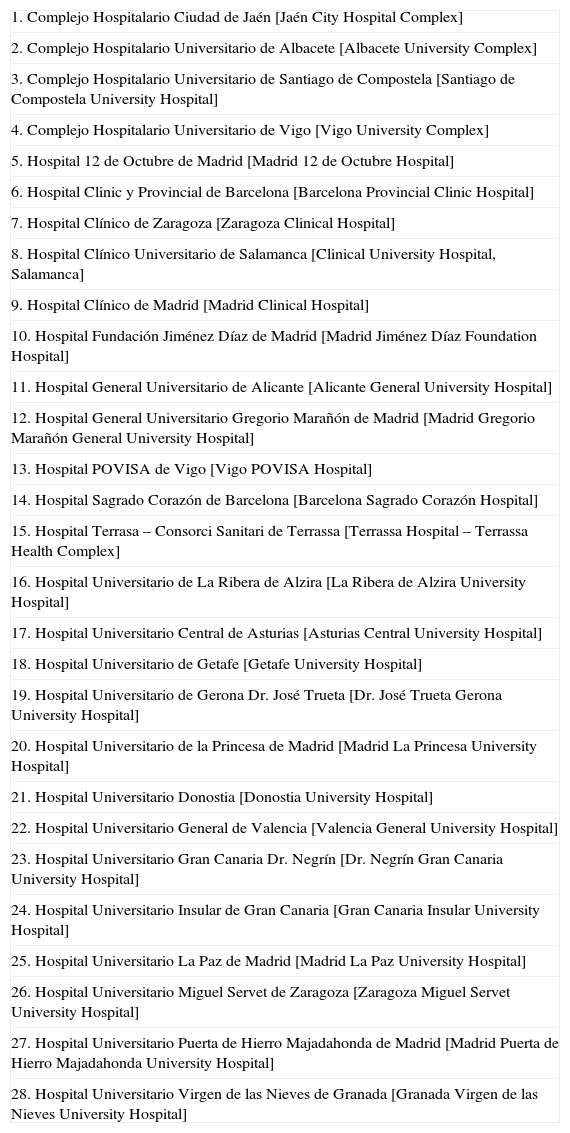
Of the 52 Spanish thoracic surgery centers, 29 (56%) answered the survey (Table 2); of these answers, we concluded that 5 centers (17.24%) have no experience in surgical treatment of DH; 11 (37.93%) have had experience with minimally invasive thoracoscopy-assisted techniques at least once, and 23 (79.3%) had at least one case treated by thoracotomy. Only 7 centers reported having performed more than 5 DPs in the last 8 years, and only our center treated more than 10 cases with minimally invasive thoracoscopic-assisted surgery. No centers have answered having experience with other types of medical or surgical treatments for this condition.
Overview of Spanish Hospital Sites That Answered the Survey.
| 1. Complejo Hospitalario Ciudad de Jaén [Jaén City Hospital Complex] |
| 2. Complejo Hospitalario Universitario de Albacete [Albacete University Complex] |
| 3. Complejo Hospitalario Universitario de Santiago de Compostela [Santiago de Compostela University Hospital] |
| 4. Complejo Hospitalario Universitario de Vigo [Vigo University Complex] |
| 5. Hospital 12 de Octubre de Madrid [Madrid 12 de Octubre Hospital] |
| 6. Hospital Clinic y Provincial de Barcelona [Barcelona Provincial Clinic Hospital] |
| 7. Hospital Clínico de Zaragoza [Zaragoza Clinical Hospital] |
| 8. Hospital Clínico Universitario de Salamanca [Clinical University Hospital, Salamanca] |
| 9. Hospital Clínico de Madrid [Madrid Clinical Hospital] |
| 10. Hospital Fundación Jiménez Díaz de Madrid [Madrid Jiménez Díaz Foundation Hospital] |
| 11. Hospital General Universitario de Alicante [Alicante General University Hospital] |
| 12. Hospital General Universitario Gregorio Marañón de Madrid [Madrid Gregorio Marañón General University Hospital] |
| 13. Hospital POVISA de Vigo [Vigo POVISA Hospital] |
| 14. Hospital Sagrado Corazón de Barcelona [Barcelona Sagrado Corazón Hospital] |
| 15. Hospital Terrasa – Consorci Sanitari de Terrassa [Terrassa Hospital – Terrassa Health Complex] |
| 16. Hospital Universitario de La Ribera de Alzira [La Ribera de Alzira University Hospital] |
| 17. Hospital Universitario Central de Asturias [Asturias Central University Hospital] |
| 18. Hospital Universitario de Getafe [Getafe University Hospital] |
| 19. Hospital Universitario de Gerona Dr. José Trueta [Dr. José Trueta Gerona University Hospital] |
| 20. Hospital Universitario de la Princesa de Madrid [Madrid La Princesa University Hospital] |
| 21. Hospital Universitario Donostia [Donostia University Hospital] |
| 22. Hospital Universitario General de Valencia [Valencia General University Hospital] |
| 23. Hospital Universitario Gran Canaria Dr. Negrín [Dr. Negrín Gran Canaria University Hospital] |
| 24. Hospital Universitario Insular de Gran Canaria [Gran Canaria Insular University Hospital] |
| 25. Hospital Universitario La Paz de Madrid [Madrid La Paz University Hospital] |
| 26. Hospital Universitario Miguel Servet de Zaragoza [Zaragoza Miguel Servet University Hospital] |
| 27. Hospital Universitario Puerta de Hierro Majadahonda de Madrid [Madrid Puerta de Hierro Majadahonda University Hospital] |
| 28. Hospital Universitario Virgen de las Nieves de Granada [Granada Virgen de las Nieves University Hospital] |
Most respondents felt that this intervention is unusual because of the rarity of the condition and symptoms in adults (55.17%), and also lack of knowledge of the medical community of surgical treatment and outcomes (58.62%). Answers were not exclusive.
DiscussionThe confusion between DH and diaphragmatic hernias, their rarity and the large amount of synonyms used in the literature (hernia, paralysis, diaphragmatic elevation or relaxation, diaphragmatic failure, Petit's disease, neurogenic muscular aplasia of the diaphragm, megaphrenia, mega-diaphragm and diaphragmatic atrophy) can cause controversy1,7,9,111 and create difficulties for spreading awareness of this disease.
Hemidiaphragm plication by paralysis or hernia is rarely performed in adults; it is more accepted in the pediatric population.4
While there are few publications and small cases of DP in adults, all show satisfactory results and minor complications, which appear to be reduced with minimally invasive techniques.8,12
In our review of the literature, we have not found any clinical trial or meta-analysis related to this issue. The publication of Freeman et al.12 is a cohort study comparing DH patients who did not undergo surgery (7 cases), with another group of patients undergoing DP by thoracotomy (11 cases) and VATS (30 cases). Due to the limited cases and design, it cannot be considered as level of evidence IIb. All other publications provide cases with level of evidence IV.
In a literature search similar to the one we conducted, Gazala et al. achieved results practically identical to ours8; of 126 publications found, only 13 were considered relevant. The latter study included all DP performed by thoracotomy (n: 111 patients) or VATS-thoracoscopy (n: 54 patients). All were observational studies. Only one cohort study was identified,4 and the others consisted of case series and clinical cases. The most voluminous series was that of Freeman et al.,12 with 41 DP cases (30 by VATS-thoracoscopy, and 11 by thoracotomy). After their review, Gazala et al. concluded that thoracotomy DP or thoracoscopy DP appear to be effective in improving respiratory function and symptoms in patients with DH; although, the results lack comprehensive analytical studies, therefore, they must be treated with caution, and they emphasize the need for quality studies focused mainly on results and long-term quality of life for patients who have undergone surgery.8
Comparing the changes of DH patients with no surgery to those who underwent surgery for DP, Freeman et al. highlight frequent hospitalizations for respiratory symptoms and work disabilities in the non-surgery patient group.8,12
However, despite good published results on the surgical treatment of this disease, it is remarkable how much the local medical community lacks awareness of these techniques; this is reflected in our findings over prolonged time from diagnosis to the referral to thoracic surgery (5 years on average, with an approximate range of 6 months to 23 years). Most of our patients had received other ineffective or palliative treatments: bronchodilators, physiotherapy or home oxygen therapy, along with the health and economic costs that this generates. In several cases, referral to thoracic surgery consultation was prompted by communications on DP in regional centers we made in recent years to increase awareness of this effective treatment.
Freeman et al. describe a similar situation, and highlight some causes which act as barriers to referral to surgical treatment of patients with DH: not attributing symptoms to diaphragmatic paralysis; doubting the potential benefits of plication; the idea of requiring a thoracotomy and thereby any consequences; shortage of quality literature in this regard; the rarity of symptomatic cases in adults, and the lack of familiarity of the procedure among surgeons.4
The survey on Spanish thoracic surgery departments reflects the limited experience with this technique in our country. Most respondents attributed this limited experience to the rarity of the disease in adults and poor dissemination of surgical treatment in the medical community. Surprisingly, most surgeries were performed by thoracotomy, even in sites with extensive experience in VATS lobectomy. Of the 29 centers that answered, only 11 performed a DP with minimally invasive techniques at least once.
Our review of literature on thoracoscopy-assisted DP in adults highlights the small number of publications and patients reported in English literature. We failed to find any case series in Spanish with more than 4 published cases.
Of the 6 publications that we consider relevant (providing more than 4 cases), 2 correspond to the same main author: Freeman, and he is referring to the same series with progressive increase in 2006 and 2009.4,12 Two other publications correspond to the same center: Deng et al.108 and Lai et al.109 of the department of cardiothoracic surgery at Westmead Hospital (Sydney, Australia).
Therefore, there are only 4 centers that have published this technique in English, with a grand total of 59 patients.
Our series, with 18 cases, would be the second largest in terms of number of patients who underwent surgery.
Beyond the known rarity of symptomatic cases in adults, we assume that the few existing publications show little interest in this condition, and very little dissemination and acceptance of thoracoscopic surgery in adults, both for international and domestic healthcare.
Our experience led us to the conviction that many patients suffering the effects of DH may benefit from the dissemination of these techniques.
ConclusionsThere are very few reports of DP-assisted thoracoscopy. When the literature was reviewed, we only found 6 series which provide a total of 59 thoracoscopy-assisted DP in adults. None in Spanish. All have few cases with levels of evidence of IV. Our series would be the second largest: 18 satisfactory cases and results (similar to those of the other publications.)
The survey of Spanish thoracic surgery departments shows that in the past 8 years, none has treated more than 10 cases with thoracoscopy-assisted surgery (except ours). Most continue to use the thoracotomy approach, and blame the rarity of the disease and the lack of dissemination of these techniques as being responsible for the lack of referrals to surgical treatment.
We believe that many patients suffering the effects of DH may benefit from these techniques; therefore, these publications (even with few cases) can contribute to adequate dissemination of this treatment among the medical community.
Conflict of InterestThe authors declare having no conflict of interest.
The authors would like to thank Ms. María Isabel Rodríguez Vera, our hospital's librarian, for her assistance in literature searches.
Please cite this article as: Rombolá CA, Genovés Crespo M, Tárraga López PJ, García Jiménez MD, Honguero Martínez AF, León Atance P, et al. Tratamiento de la eventración diafragmática en adultos mediante plicatura diafragmática asistida por videotoracoscopia. ¿Es una técnica difundida en nuestro medio? Revisión de la literatura, resultados de una encuesta nacional. Cir Esp. 2014;92:453–462.