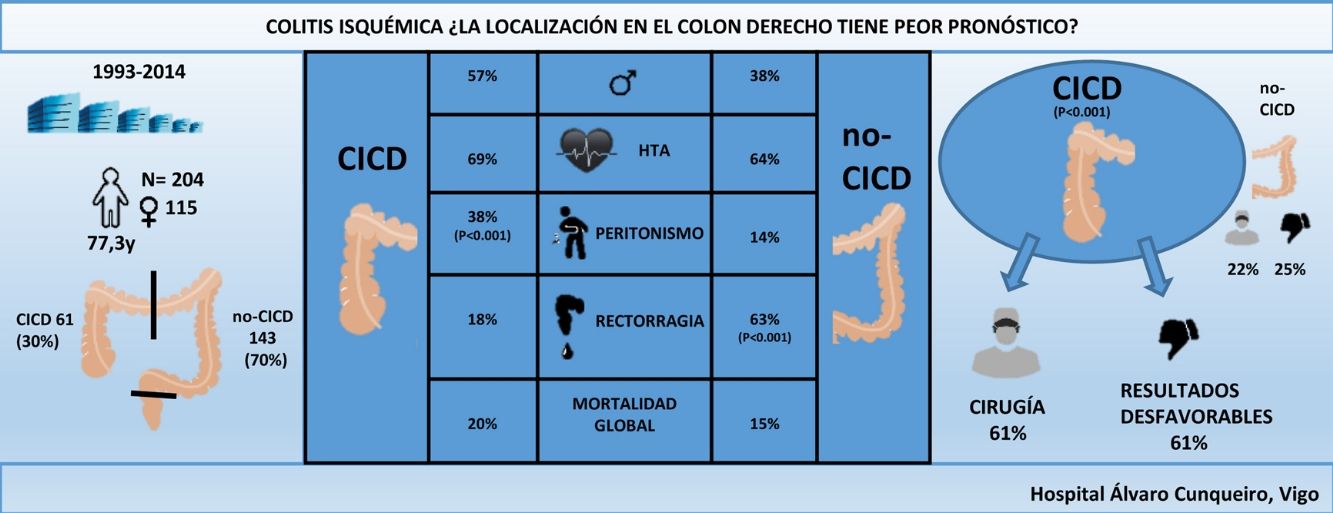
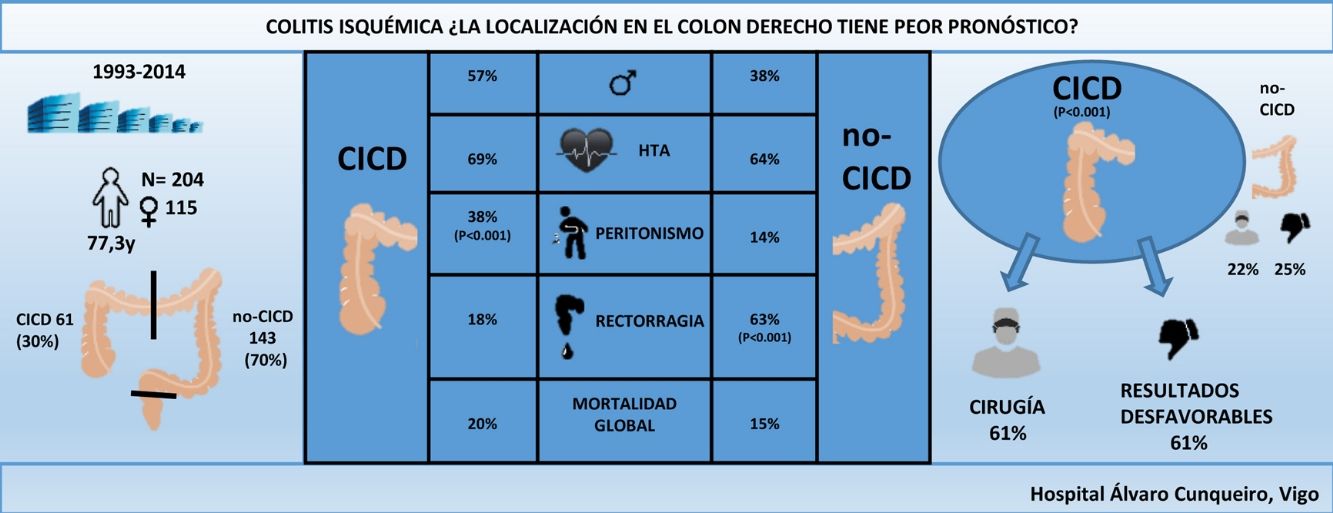
Most patients with ischemic colitis have a favourable evolution; nevertheless, the location in the right colon has been associated with a worse prognosis. The purpose of this study is to compare the clinical presentation and results of right colon ischemic colitis (CICD) with ischemic colitis of other colonic segments (non-CIDC).
MethodsRetrospective, observational study of patients admitted to our hospital with ischemic colitis between 1993 and 2014, identified through a computerized search of ICD9 codes. They were divided into 2 groups: CICD and non-CICD. Comorbidities, clinical presentation, need for surgery, and mortality were compared. Multivariate analysis was performed using logistic regression adjusting for age and sex. Statistical significance was established at a value of P < 0.05.
ResultsA total of 204 patients were identified, 61 (30%) with CICD; 61% of CICD patients required surgery compared to 22% of non-CICD patients (P < 0.001). Differences in post-surgical mortality (32% vs 55%) and overall mortality (20% vs 15%) were not statistically significant. CICD patients had more commonly unfavourable outcomes than non-CICD patients (61% vs 25%, P < 0.001). The odds ratio (OR) for surgery was 5.28 and 4.47 for unfavourable outcomes for patients with CICD.
ConclusionsCICD patients have a worse prognosis than non-CICD patients, 5 times more likely to need surgery and 4 times more likely to have unfavourable outcomes.
La mayoría de los pacientes con colitis isquémica tienen una evolución favorable; sin embargo, se ha relacionado la localización en el colon derecho con un peor pronóstico. El propósito de este estudio es comparar la presentación clínica y los resultados de la colitis isquémica del colon derecho (CICD) con la colitis isquémica de otros segmentos del colon (no CICD).
MétodosEstudio retrospectivo, observacional de los pacientes ingresados en nuestro hospital con colitis isquémica entre 1993 y 2014, identificados mediante búsqueda computarizada de los códigos de ICD-9. Se dividieron en 2 grupos: CICD y no CICD. Se compararon las comorbilidades, presentación clínica, necesidad de cirugía y mortalidad. El análisis multivariado se realizó mediante regresión logística ajustando por edad y sexo. La significación estadística se estableció en un valor de p < 0,05.
ResultadosFueron identificados 204 pacientes, 61 (30%) con CICD. El 61% de los pacientes con CICD necesitaron cirugía en comparación con el 22% de los pacientes no CICD (p < 0,001). La mortalidad posquirúrgica (32 vs. 55%) y la global (20 vs. 15%) no fueron estadísticamente significativas entre los 2 grupos. Los pacientes con CICD tuvieron resultados desfavorables más comúnmente que los no CICD (61 vs. 25%; p < 0,001). La odds ratio (OR) para cirugía fue de 5,28 y de 4,47 para resultados desfavorables para pacientes con CICD.
ConclusionesLos pacientes con CICD tienen peor pronóstico que los pacientes con no CICD, 5 veces más probabilidades de necesitar cirugía y 4 veces más de presentar resultados desfavorables.
Ischemic colitis (IC), which is the result of vascular insufficiency of the colon, is the most common form of gastrointestinal ischemia, occurring most frequently in females and between the 6th and 8th decades of life1,2. Any segment of the colon can be affected, but the left colon is the predominant location, found in 75%–80% of patients3,4. The evolution of the disease depends on the severity of its presentation and, therefore, knowledge of certain prognostic factors is important when deciding on the best therapeutic strategy for each patient5. Some authors have not been able to establish a relationship between the severity of IC and its anatomical location5,6, but a higher incidence of comorbidities has been documented in IC of the right colon, such as coronary artery disease, atrial fibrillation, chronic kidney failure (CKF) or hemodialysis requirements, which may contribute to a greater severity of the disease in these patients7–9. Very few studies have compared the results between patients with right IC (RIC) and non-RIC10 subjects, and our purpose was to analyze the clinical findings and therapeutic results between these 2 groups.
MethodsWe conducted a retrospective, observational study of patients admitted to our hospital between 1993 and 2014 with the diagnosis of IC, as identified by a database search of the codes of the International Statistical Classification of Diseases and Related Health Problems (ICD-9): 557.0 (acute ischemic colitis, ulcerative colitis, fulminant ulcerative colitis), 557.1 (chronic ischemic colitis due to mesenteric artery insufficiency), and 557.9 (ischemic colitis).
We established 2 groups of patients for study. RIC was defined as that affecting the cecum, ascending colon or hepatic flexure and the proximal third of the transverse colon. Involvement of the distal 2/3 of the transverse colon, splenic flexure, descending colon, and sigmoid colon was considered non-RIC. In this way, patients diagnosed with pancolitis, multisegmental colitis or rectal involvement were excluded. This study did not analyze patients with benign or malignant intestinal obstruction, associated colorectal cancer, inflammatory bowel disease, intestinal ischemia associated with occlusion of the inferior mesenteric artery, IC secondary to abdominal trauma, patients during the immediate postoperative period after cardiovascular surgery (aortoiliac reconstruction, cardiopulmonary bypass or aortic aneurysm surgery), or patients with no histopathological identification of the disease.
Under this premise, 202 out of the 411 registered patients were excluded. Another 5 patients were also excluded due to the lack of certain data pertinent to the analysis. Therefore, a total of 204 patients remained for analysis.
The following variables were collected in all patients:
- -
Clinical history: age, sex, duration of symptoms until hospital admission; existence of comorbidities, including arterial hypertension (HTN), diabetes mellitus, chronic obstructive pulmonary disease (COPD), arrhythmia, CRF, heart failure, ischemic heart disease, arteriosclerosis, dyslipidemia, constipation, cerebrovascular accident, hemodialysis, and number of associated diseases.
- -
Symptoms at admission: abdominal pain, localized abdominal pain, diffuse abdominal pain, rectal bleeding, peritonism, vomiting, localized pain and rectal bleeding, diffuse abdominal pain and rectal bleeding, American Society of Anesthesiologists (ASA) score.
‘Mortality’ refers to mortality that occurred within 30 days of diagnosis, after surgical treatment or during the hospital stay if it was longer than 30 days. ‘Postoperative mortality’ is that which after occurred surgical treatment of the condition, and ‘global mortality’ is postoperative deaths that occurred during conservative treatment.
The results have been classified as favorable (satisfactory response to conservative treatment) and unfavorable (requiring surgery, or death due to failure of conservative treatment).
Statistical analysisThe 2 study groups were compared in terms of comorbidities, clinical and physical data, need for surgery, and mortality.
Dichotomous variables are expressed as percentage and number of patients, and continuous variables as mean and standard deviation (SD). Bivariate comparisons of the continuous variables were made using the Student’s t test, while bivariate comparisons of dichotomous variables were made using the chi-squared or Fisher’s exact test, as appropriate. The multivariate analysis was performed using logistic regression, adjusted for age and sex. Statistical significance was established at a P value <.05. All analyses were performed with the IBM SPSS Statistics® program, version 25.
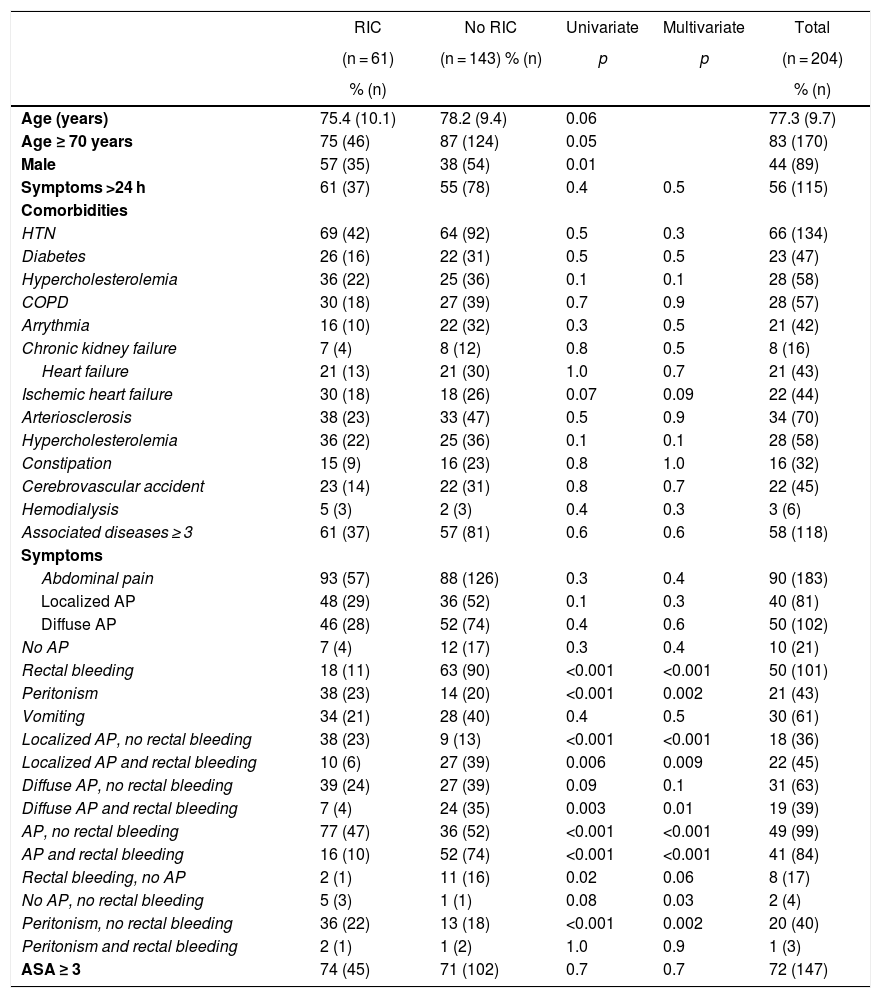
ResultsA total of 204 patients were identified (115 women and 89 men), with a mean age of 77.3 ± 9.7 years. Table 1 shows the characteristics of the presentation of the disease according to the location. Most of the patients (83%) were ≥70 years of age, and their symptoms had been developing for more than 24 h in 56% of the cases. The most frequently associated disease was HTN (66%), and 58% of the patients had ≥3 comorbidities. No statistically significant differences were found between the existing comorbidities in the 2 study groups.
RIC vs non-RIC: comorbidities and symptoms.
| RIC | No RIC | Univariate | Multivariate | Total | |
|---|---|---|---|---|---|
| (n = 61) | (n = 143) % (n) | p | p | (n = 204) | |
| % (n) | % (n) | ||||
| Age (years) | 75.4 (10.1) | 78.2 (9.4) | 0.06 | 77.3 (9.7) | |
| Age ≥ 70 years | 75 (46) | 87 (124) | 0.05 | 83 (170) | |
| Male | 57 (35) | 38 (54) | 0.01 | 44 (89) | |
| Symptoms >24 h | 61 (37) | 55 (78) | 0.4 | 0.5 | 56 (115) |
| Comorbidities | |||||
| HTN | 69 (42) | 64 (92) | 0.5 | 0.3 | 66 (134) |
| Diabetes | 26 (16) | 22 (31) | 0.5 | 0.5 | 23 (47) |
| Hypercholesterolemia | 36 (22) | 25 (36) | 0.1 | 0.1 | 28 (58) |
| COPD | 30 (18) | 27 (39) | 0.7 | 0.9 | 28 (57) |
| Arrythmia | 16 (10) | 22 (32) | 0.3 | 0.5 | 21 (42) |
| Chronic kidney failure | 7 (4) | 8 (12) | 0.8 | 0.5 | 8 (16) |
| Heart failure | 21 (13) | 21 (30) | 1.0 | 0.7 | 21 (43) |
| Ischemic heart failure | 30 (18) | 18 (26) | 0.07 | 0.09 | 22 (44) |
| Arteriosclerosis | 38 (23) | 33 (47) | 0.5 | 0.9 | 34 (70) |
| Hypercholesterolemia | 36 (22) | 25 (36) | 0.1 | 0.1 | 28 (58) |
| Constipation | 15 (9) | 16 (23) | 0.8 | 1.0 | 16 (32) |
| Cerebrovascular accident | 23 (14) | 22 (31) | 0.8 | 0.7 | 22 (45) |
| Hemodialysis | 5 (3) | 2 (3) | 0.4 | 0.3 | 3 (6) |
| Associated diseases ≥ 3 | 61 (37) | 57 (81) | 0.6 | 0.6 | 58 (118) |
| Symptoms | |||||
| Abdominal pain | 93 (57) | 88 (126) | 0.3 | 0.4 | 90 (183) |
| Localized AP | 48 (29) | 36 (52) | 0.1 | 0.3 | 40 (81) |
| Diffuse AP | 46 (28) | 52 (74) | 0.4 | 0.6 | 50 (102) |
| No AP | 7 (4) | 12 (17) | 0.3 | 0.4 | 10 (21) |
| Rectal bleeding | 18 (11) | 63 (90) | <0.001 | <0.001 | 50 (101) |
| Peritonism | 38 (23) | 14 (20) | <0.001 | 0.002 | 21 (43) |
| Vomiting | 34 (21) | 28 (40) | 0.4 | 0.5 | 30 (61) |
| Localized AP, no rectal bleeding | 38 (23) | 9 (13) | <0.001 | <0.001 | 18 (36) |
| Localized AP and rectal bleeding | 10 (6) | 27 (39) | 0.006 | 0.009 | 22 (45) |
| Diffuse AP, no rectal bleeding | 39 (24) | 27 (39) | 0.09 | 0.1 | 31 (63) |
| Diffuse AP and rectal bleeding | 7 (4) | 24 (35) | 0.003 | 0.01 | 19 (39) |
| AP, no rectal bleeding | 77 (47) | 36 (52) | <0.001 | <0.001 | 49 (99) |
| AP and rectal bleeding | 16 (10) | 52 (74) | <0.001 | <0.001 | 41 (84) |
| Rectal bleeding, no AP | 2 (1) | 11 (16) | 0.02 | 0.06 | 8 (17) |
| No AP, no rectal bleeding | 5 (3) | 1 (1) | 0.08 | 0.03 | 2 (4) |
| Peritonism, no rectal bleeding | 36 (22) | 13 (18) | <0.001 | 0.002 | 20 (40) |
| Peritonism and rectal bleeding | 2 (1) | 1 (2) | 1.0 | 0.9 | 1 (3) |
| ASA ≥ 3 | 74 (45) | 71 (102) | 0.7 | 0.7 | 72 (147) |
The dichotomic variables are expressed as percentage (number of patients) and the continuous variables as mean (DE). The bivariate comparisons of the continuous variables were done with the Student’s t test, while the bivariate comparisons of dichotomic variables were done with the chi-squared test or Fisher’s exact test, as needed. The multivariate analysis was calculated by means of logistic regression, adjusting for age and sex.
RIC: isolated right ischemic colitis; AP: abdominal pain; COPD: chronic obstructive pulmonary disease; HTN: hypertension; non-RIC: no isolated right ischemic colitis.
The most predominant symptom was abdominal pain (90%), which was diffuse in 50% of the cases. Meanwhile, 50% of the patients reported rectal bleeding, 29.9% vomiting, and 21.1% presented peritonism.
Sixty-one (30%) patients were diagnosed with RIC, which was more frequent in men (57% vs 38%; P = .01). Out of the 101 patients who reported rectal bleeding, 18% were diagnosed with RIC, and 63% were non-RIC (P < .001). Peritonism was more frequent in patients with RIC (38% vs 14%; P < .001). Patients with RIC more frequently presented abdominal pain and peritonism without rectal bleeding (P < .001). A higher percentage of non-RIC patients initially presented without abdominal pain, but with rectal bleeding (2% vs 11%; P < .05). Lastly, 20% of the patients presented peritonism without rectal bleeding, 36% from the RIC group (P < 0.001).
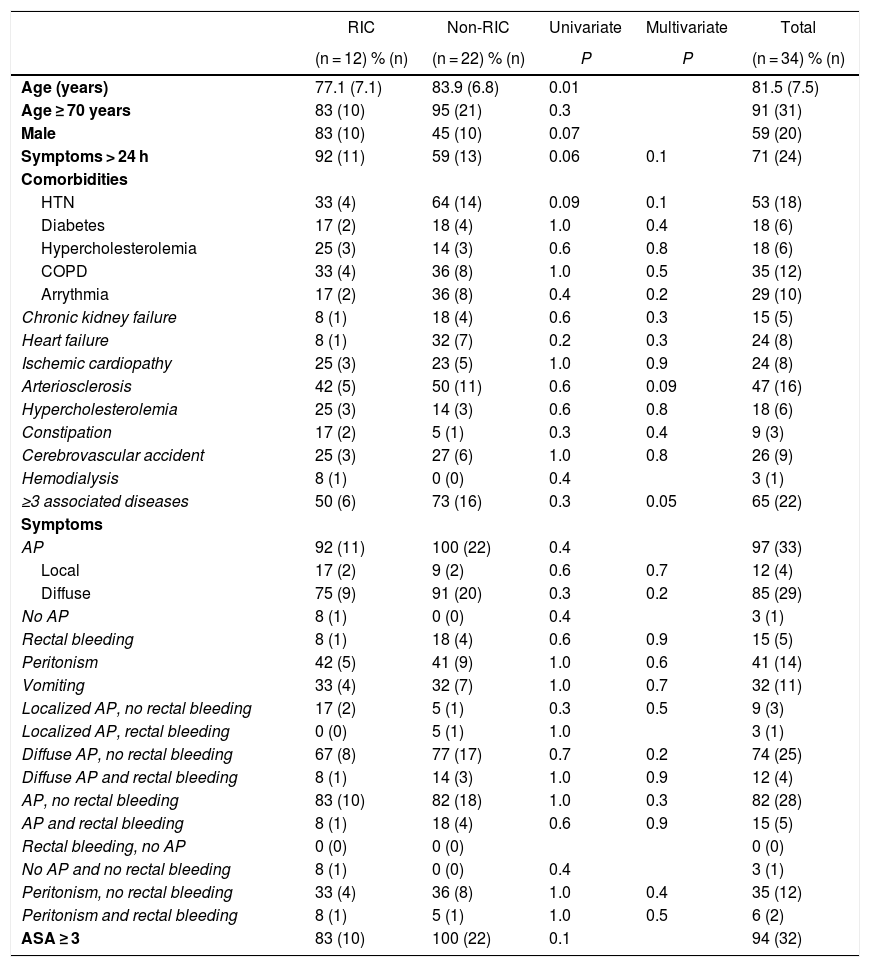
Overall mortality was 34 patients (17%), specifically 12 (20%) and 22 (15%) in the RIC and non-RIC groups, respectively. The comparative analysis of the comorbidities and presentation of the disease of the deceased patients in the 2 groups did not demonstrate the existence of significant variables associated with mortality (Table 2).
Comorbidities and symptoms in patient deaths with RIC vs non-RIC.
| RIC | Non-RIC | Univariate | Multivariate | Total | |
|---|---|---|---|---|---|
| (n = 12) % (n) | (n = 22) % (n) | P | P | (n = 34) % (n) | |
| Age (years) | 77.1 (7.1) | 83.9 (6.8) | 0.01 | 81.5 (7.5) | |
| Age ≥ 70 years | 83 (10) | 95 (21) | 0.3 | 91 (31) | |
| Male | 83 (10) | 45 (10) | 0.07 | 59 (20) | |
| Symptoms > 24 h | 92 (11) | 59 (13) | 0.06 | 0.1 | 71 (24) |
| Comorbidities | |||||
| HTN | 33 (4) | 64 (14) | 0.09 | 0.1 | 53 (18) |
| Diabetes | 17 (2) | 18 (4) | 1.0 | 0.4 | 18 (6) |
| Hypercholesterolemia | 25 (3) | 14 (3) | 0.6 | 0.8 | 18 (6) |
| COPD | 33 (4) | 36 (8) | 1.0 | 0.5 | 35 (12) |
| Arrythmia | 17 (2) | 36 (8) | 0.4 | 0.2 | 29 (10) |
| Chronic kidney failure | 8 (1) | 18 (4) | 0.6 | 0.3 | 15 (5) |
| Heart failure | 8 (1) | 32 (7) | 0.2 | 0.3 | 24 (8) |
| Ischemic cardiopathy | 25 (3) | 23 (5) | 1.0 | 0.9 | 24 (8) |
| Arteriosclerosis | 42 (5) | 50 (11) | 0.6 | 0.09 | 47 (16) |
| Hypercholesterolemia | 25 (3) | 14 (3) | 0.6 | 0.8 | 18 (6) |
| Constipation | 17 (2) | 5 (1) | 0.3 | 0.4 | 9 (3) |
| Cerebrovascular accident | 25 (3) | 27 (6) | 1.0 | 0.8 | 26 (9) |
| Hemodialysis | 8 (1) | 0 (0) | 0.4 | 3 (1) | |
| ≥3 associated diseases | 50 (6) | 73 (16) | 0.3 | 0.05 | 65 (22) |
| Symptoms | |||||
| AP | 92 (11) | 100 (22) | 0.4 | 97 (33) | |
| Local | 17 (2) | 9 (2) | 0.6 | 0.7 | 12 (4) |
| Diffuse | 75 (9) | 91 (20) | 0.3 | 0.2 | 85 (29) |
| No AP | 8 (1) | 0 (0) | 0.4 | 3 (1) | |
| Rectal bleeding | 8 (1) | 18 (4) | 0.6 | 0.9 | 15 (5) |
| Peritonism | 42 (5) | 41 (9) | 1.0 | 0.6 | 41 (14) |
| Vomiting | 33 (4) | 32 (7) | 1.0 | 0.7 | 32 (11) |
| Localized AP, no rectal bleeding | 17 (2) | 5 (1) | 0.3 | 0.5 | 9 (3) |
| Localized AP, rectal bleeding | 0 (0) | 5 (1) | 1.0 | 3 (1) | |
| Diffuse AP, no rectal bleeding | 67 (8) | 77 (17) | 0.7 | 0.2 | 74 (25) |
| Diffuse AP and rectal bleeding | 8 (1) | 14 (3) | 1.0 | 0.9 | 12 (4) |
| AP, no rectal bleeding | 83 (10) | 82 (18) | 1.0 | 0.3 | 82 (28) |
| AP and rectal bleeding | 8 (1) | 18 (4) | 0.6 | 0.9 | 15 (5) |
| Rectal bleeding, no AP | 0 (0) | 0 (0) | 0 (0) | ||
| No AP and no rectal bleeding | 8 (1) | 0 (0) | 0.4 | 3 (1) | |
| Peritonism, no rectal bleeding | 33 (4) | 36 (8) | 1.0 | 0.4 | 35 (12) |
| Peritonism and rectal bleeding | 8 (1) | 5 (1) | 1.0 | 0.5 | 6 (2) |
| ASA ≥ 3 | 83 (10) | 100 (22) | 0.1 | 94 (32) |
Dichotomous variables are expressed as a percentage (number of patients) and continuous variables as mean (SD). Bivariate comparisons of continuous variables were performed with the Student’s t test, while bivariate comparisons of dichotomous variables were made using the chi-squared test or Fisher’s exact test, as appropriate. The multivariate analysis was calculated using logistic regression, adjusting for age and sex.
RIC: isolated right ischemic colitis; AP: abdominal pain; COPD: chronic obstructive pulmonary disease; HTN: hypertension; non-RIC: no isolated ischemic colitis.
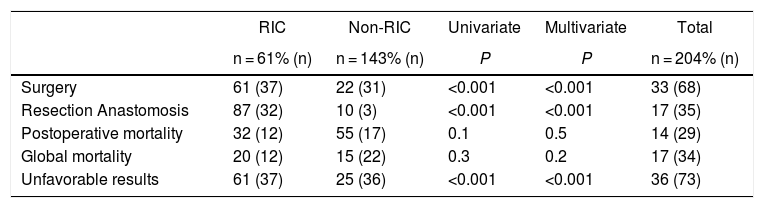
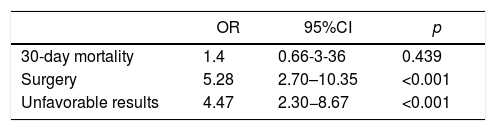
Patients with RIC required surgery in a higher percentage than non-RIC patients (61% vs 22%; P < .001), and resection with primary anastomosis was the most frequently used technique (87 vs 10; P < .001). Proportionally, postoperative mortality was higher in non-RIC patients (32% vs 55%) while overall mortality was higher in RIC patients (20% vs 15%), neither of which reached statistical significance. A total of 107 non-RIC patients (75%) presented favorable results. The unfavorable results were significantly higher in patients with RIC (61% vs 25%; P < .001) (Tables 3 and 4).
Results: RIC vs non-RIC.
| RIC | Non-RIC | Univariate | Multivariate | Total | |
|---|---|---|---|---|---|
| n = 61% (n) | n = 143% (n) | P | P | n = 204% (n) | |
| Surgery | 61 (37) | 22 (31) | <0.001 | <0.001 | 33 (68) |
| Resection Anastomosis | 87 (32) | 10 (3) | <0.001 | <0.001 | 17 (35) |
| Postoperative mortality | 32 (12) | 55 (17) | 0.1 | 0.5 | 14 (29) |
| Global mortality | 20 (12) | 15 (22) | 0.3 | 0.2 | 17 (34) |
| Unfavorable results | 61 (37) | 25 (36) | <0.001 | <0.001 | 36 (73) |
RIC: isolated right ischemic colitis; non-RIC: no isolated ischemic colitis.
Unfavorable results: RIC vs non-RIC.
| OR | 95%CI | p | |
|---|---|---|---|
| 30-day mortality | 1.4 | 0.66-3-36 | 0.439 |
| Surgery | 5.28 | 2.70–10.35 | <0.001 |
| Unfavorable results | 4.47 | 2.30−8.67 | <0.001 |
The multivariate analysis was performed by logistic regression, adjusting for age and sex.
RIC: isolated right ischemic colitis; 95%CI: 95% confidence interval; non-RIC: no isolated right ischemic colitis; OR: odds ratio.
The clinical presentation of IC is highly variable, ranging from moderate forms, which progress favorably with conservative treatment, to severe forms, which require surgery or lead to the death of the patient5,8.
Our study confirms that IC is more frequent in females, in patients aged ≥70 years with ≥3 associated diseases, and that the most common comorbidity is HTN8,11. Between the 2 groups analyzed, there were no differences in the age of presentation of the disease or in the duration of symptoms until diagnosis; RIC was more prevalent in men (57% vs 38%; P<.05). Associated comorbidities and disease severity differ according to the segment of the colon affected, and the location in the right colon may be the most significant predictor of severity7,12.
There is a prevalence of RIC in patients with CKD, especially in those treated with hemodialysis8. Hemodialysis favors a decrease in mesenteric flow due to a decrease in cardiac output, causing hypotension and vasoconstriction of the vasa rectus of the right colon, and limiting marginal circulation13. In some series7 CKF is associated with a frequency 3 times higher than RIC, and involvement of the right colon was present in 82% of patients on dialysis9, which can increase the risk of adverse effects by up to 8.5 times13. Other authors10 have not found a statistically significant difference in the incidence of CKF and hemodialysis between patients with RIC and those without RIC.
While our disease location pattern considers ischemic lesions located between the cecum and the proximal third of the transverse colon involvement of the right colon, other authors have based its distribution pattern on the most proximal site of the disease, regardless of the distal extension. Hence, in some studies, the incidence of IC between the cecum and the hepatic flexure is actually 9.9% while, when adding this location to other segments, it is 25%7. In other series, 65% are actually isolated IC of the right colon, and the remaining 35% are lesions that affect the transverse colon, left colon, and even pancolitis in addition to the right colon9. In the study by Chang et al.8, 24% of the patients analyzed had been diagnosed with CKF, and 100% of these had received hemodialysis. Only 8% of our patients had CKF, and 5% of the patients with RIC had been dialyzed, so we cannot confirm that dialysis is a predisposing factor for a higher incidence of the disease in the right colon. This difference in the prevalence between hemodialysis and RIC could be explained by the different way of classifying the lesions in the right colon and the fact that there were fewer hemodialysis patients in our study.
Associated diseases, such as coronary artery disease and atrial fibrillation, have been reported to be 2 times more common in patients with RIC than in other locations7. For other authors8, comorbidities such as hypertension, atrial fibrillation, coronary artery disease, heart failure, and diabetes mellitus are not related to the location of IC. In our study, patients with RIC had ≥3 associated diseases than non-RIC patients and had a higher prevalence of HTN, diabetes mellitus, COPD, coronary artery disease, and arteriosclerosis, although these results were not statistically significant.
In 78%–87% and 58%–84% of patients with IC, the most common symptoms are abdominal pain and rectal bleeding, respectively14,15, but the clinical presentation differs between patients with and without RIC10. 50% of our patients manifested rectal bleeding, and 90% presented localized or diffuse abdominal pain (in similar percentages), regardless of the location of the disease.
In our series, 77% of the patients with RIC had acute abdominal pain, no rectal bleeding2,4,10,12,16, and the incidence of peritonism was significantly higher than in non-RIC patients, perhaps as an expression of transmural colonic lesion5.
Patients with RIC have worse outcomes than patients with IC in other locations or when other segments are affected simultaneously2,9,10. In the multicenter study of the work-group for the study of IC in Spain, Montoro et al.16 showed that unfavorable results are more frequent in RIC than in non-RIC patients (41% vs 10%; P < .001). An overall mortality rate has been reported in patients with RIC that is approximately 2 times higher than in non-RIC patients and a 5 times higher rate in patients requiring surgery (55% vs 11%; P < .001), but a very similar postoperative mortality rate10.
Although 61% of patients in our study with RIC required surgery (which is almost 3 times more frequently than non-RIC patients), postoperative and overall mortality were not statistically significant, indicating that the higher mortality rate in this group can be explained by the natural evolutionary process of the disease10. Unfavorable results, defined by the need for surgery and mortality with conservative treatment, were significantly more frequent in the RIC group (61% vs 25%; P < .001). The overall mortality in our series was 17%. Meanwhile no correlation was found between the results and comorbidities or the clinical presentation of the disease.
Adjusted for age and sex, the odds ratio for 30-day mortality was 1.4 for patients with RIC, which demonstrates that there is no association between the location of the isolated disease in the right colon and mortality. The odds ratio for surgery and unfavorable outcomes was 5.3 and 4.5 for RIC patients versus non-RIC patients, respectively. This supports the hypothesis that RIC patients have a worse prognosis. However, more studies and more evidence will be needed to determine whether patients with RIC should be managed differently than non-RIC patients17.
This study has some limitations, including those inherent to a retrospective observational study: all the patients analyzed had IC and were hospitalized, which may generate a bias compared to the general population we treat and the patients who, even being diagnosed with probable IC, follow an outpatient regimen. On the other hand, some variables that are used for the evaluation of the disease (analytical, radiological or endoscopic data) have not been recorded; therefore, we must not rule out that there may be unanalyzed factors that could influence our results.
This study has not demonstrated an association between RIC and patient comorbidities. It most commonly presents with localized abdominal pain and peritonism, with no rectal bleeding. We can confirm that the isolated location of the disease in the right colon is a highly predictive factor for a worse prognosis compared to the location of IC in other segments, since patients with RIC are 5 and 4 times more likely to have to be treated surgically and have unfavorable results, respectively, than non-RIC patients.
FundingThis study has received no specific funding from public, commercial or non-profit organizations.
Conflict of interestsVincenzo Vigorita has no conflict of interests to declare.
Marta Paniagua García-Señoráns has no conflict of interests to declare.
Gianluca Pellino has no conflict of interests to declare.
Paula Troncoso Pereira has no conflict of interests to declare.
Alberto de San Ildefonso Pereira has no conflict of interests to declare.
Enrique Moncada Iribarren has no conflict of interests to declare.
Raquel Sánchez Santos has no conflict of interests to declare.
Jose Enrique Casal Núñez has no conflict of interests to declare.
Please cite this article as: Vigorita V, García-Señoráns MP, Pellino G, Troncoso Pereira P, de San Ildefonso Pereira A, Moncada Iribarren E, et al. Colitis isquémica. ¿La localización en el colon derecho tiene peor pronóstico? Cir Esp. 2022;100:74–80.