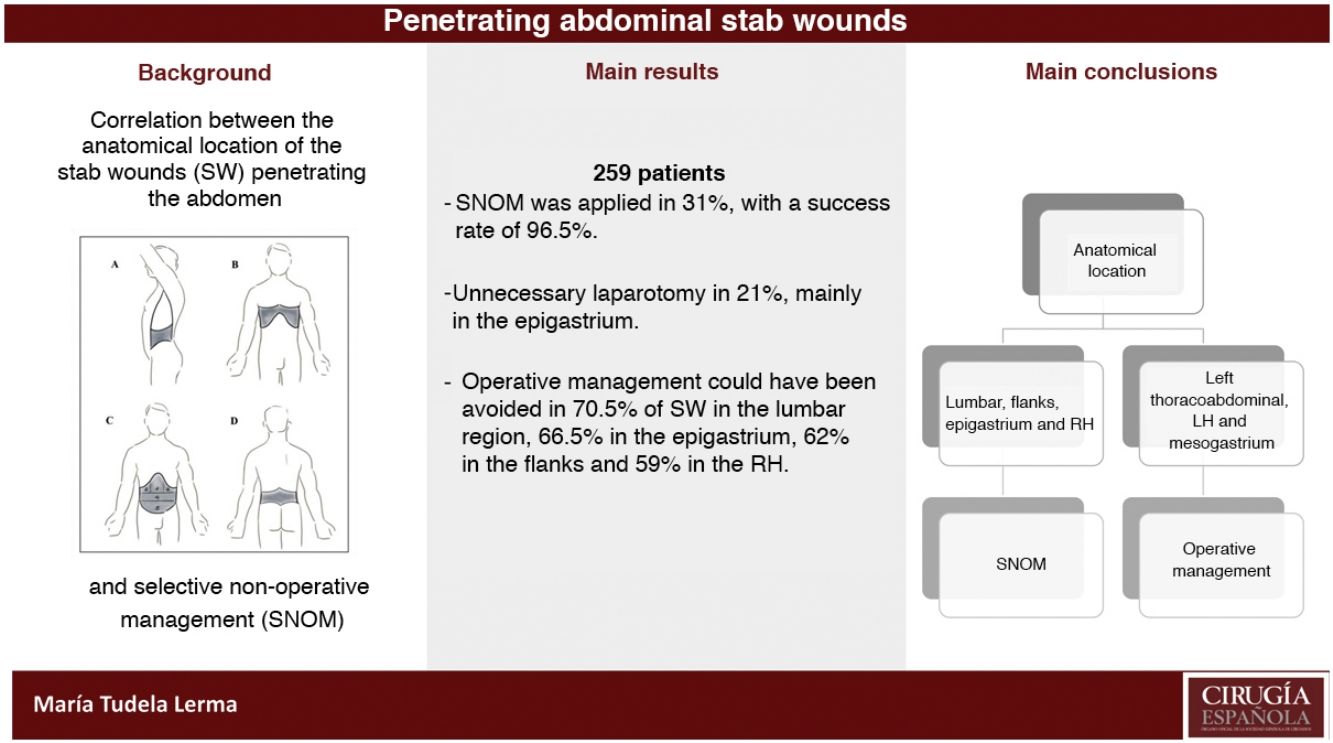
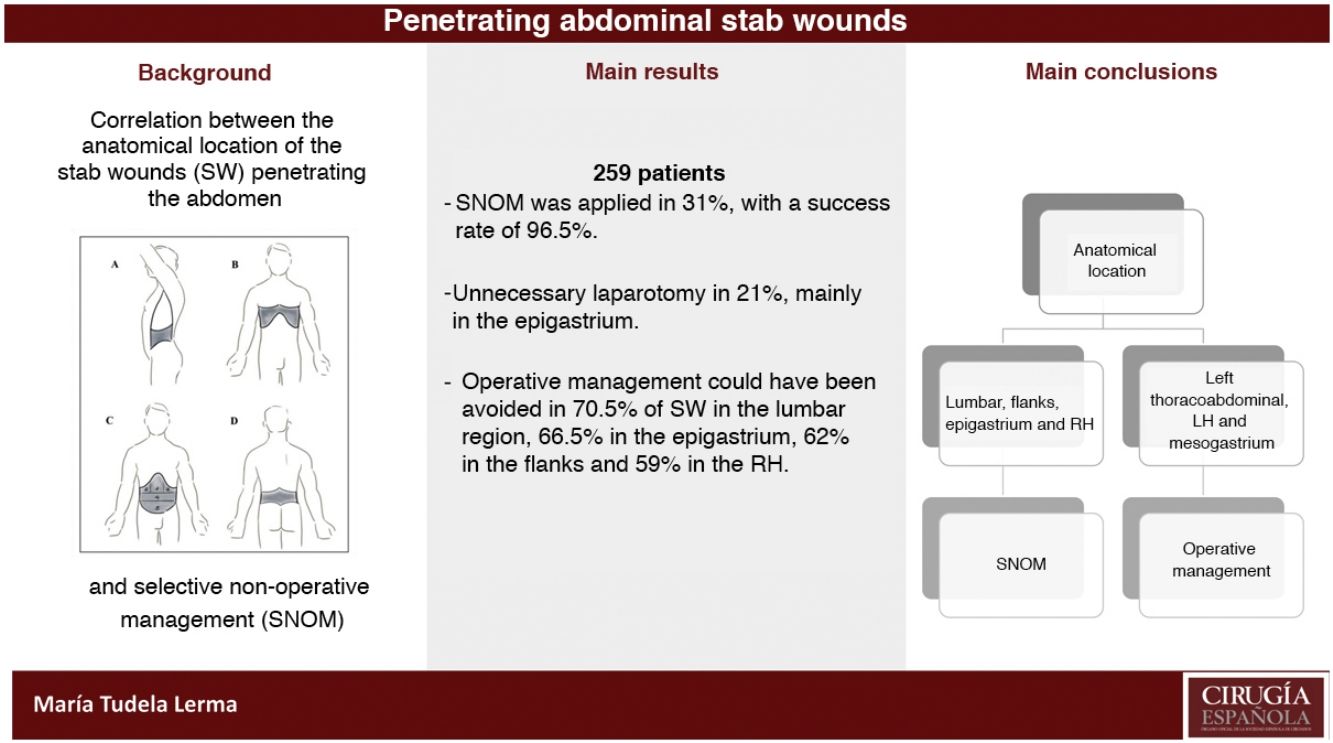
The relationship between the anatomical location of penetrating abdominal stab wounds (SW) and the rate of selective non-operative management (SNOM) based on that location is scarcely reflected in the specialized literature. Our main objective has been to assess this rate based on the anatomical location, and our results.
MethodsRetrospective review of a prospective registry of abdominal trauma from April 1993 to June 2020. The two study groups considered were the Operative Management (OM), and the SNOM, including in this one the use of diagnostic laparoscopy. Penetrating SWs in the abdomen were classified according to anatomical location.
ResultsWe identified 259 patients who fulfilled the inclusion criteria. SNOM was applied in 31% of the patients with a success rate of 96%, and it was more frequent in the lumbar, flank, and thoraco-abdominal regions; within the anterior abdomen it was more applicable in the RH, followed by the LH and epigastrium, respectively. An unnecessary laparotomy was done in 21% of patients, with the highest number in the epigastrium. Taking into account the unnecessary laparotomies and the rates of successful SNOM, 70.5% of lumbar, 66.5% of epigastric, 62% of flank, and 59% of RH penetrating SW could have been managed without a laparotomy.
ConclusionsSNOM of penetrating SW in the abdomen has been safer and more applicable in those located in the lumbar, flank, epigastric, and RH regions.
La localización anatómica de las heridas por arma blanca (HAB) penetrantes en abdomen y su relación con el manejo selectivo no operatorio (MSNO) tiene escaso reflejo en la literatura especializada. Nuestro objetivo principal ha sido valorar la tasa de MSNO en función de esa localización anatómica, y sus resultados.
MétodosRevisión retrospectiva del registro prospectivo de trauma abdominal desde abril de 1993 hasta junio de 2020. Los dos grupos a estudio fueron manejo operatorio (MO), y MSNO, incluyendo en este último grupo el uso de laparoscopias exploradora como método diagnóstico. Se clasificaron las HAB penetrantes en abdomen en función de su localización anatómica.
ResultadosIdentificamos 259 pacientes que cumplían los criterios de inclusión. El MSNO se aplicó en el 31% de los pacientes con una tasa de éxito del 96,5%. En las HAB de las regiones lumbares, flancos, y tóraco-abdominales fue donde se optó más frecuentemente por este manejo; y en el abdomen anterior fue más aplicable en hipocondrio derecho (HD), seguido del hipocondrio izquierdo (HI) y epigastrio. Se realizó una laparotomía innecesaria en el 21%, con la cifra más alta en epigastrio. Teniendo en cuenta los porcentajes de MSNO y laparotomías evitables en cada región, el 70,5% de las HAB lumbares, el 66,5% de las epigástricas, 62% de flancos y el 59% de HD se podrían haber manejado con éxito sin laparotomía.
ConclusionesEl MSNO de las HAB penetrantes en abdomen ha resultado más seguro y aplicable en las localizadas en las regiones lumbares, flancos, epigastrio e HD.
In recent years, selective non-operative management (SNOM) has become a widely accepted practice for the treatment of stab wounds (SW) penetrating the abdomen.1,2 This approach has been shown to be effective in reducing the rate of avoidable laparotomies, without increasing morbidity or mortality,3–5 as well as reducing the average hospital stay and associated costs.6
The correlation between the anatomical location of the SW and SNOM rates based on that location has received little attention in the medical literature other than the finding that only 50%–75% of all anterior abdominal wounds penetrate the peritoneal cavity and, of these, 50%–75% cause an injury that will require operative management (OM). For this reason, a relevant percentage of stable and asymptomatic patients can benefit from SNOM. On the other hand, assuming that they are injuries caused by a low transmission of kinetic energy, the possibility of visceral injuries will be determined by the position of the victim (generally standing) and the length and characteristics of the weapon, among other possible factors.
For this study, our main objective was to assess the success rate of SNOM for penetrating SW in the abdomen based on the anatomical location. In addition, we have analyzed our rate of unnecessary laparotomies in an extensive series of patients, also based on anatomical location, as well as the potential SNOM rate in light of these unnecessary laparotomies and successful cases of SNOM.
MethodsWe conducted an observational cohort study following the STROBE Statement7 and analyzing all abdominal SW included in our prospective trauma registry between April 1993 and June 2020. The study included patients ≥18 years of age with peritoneal penetration that had been confirmed by one or several of the following methods: local wound exploration under local anesthesia, laparotomy, laparoscopy (LPS) or abdominal CT without triple contrast. In obese, intoxicated and/or combative patients in whom local exploration of the wound was impracticable or incomplete, as well as certain cases of penetration of the fascia with uncertain penetration of the peritoneum, LPS was performed preferentially. Injuries were defined as ‘multiple SW’ when more than one penetrating wound was identified in the cavity.
The therapeutic approaches to penetrating abdominal SW were classified into 2 categories: operative management (OM), and selective non-operative management (SNOM). All laparotomies, LPS converted to laparotomy, and therapeutic LPS were considered OM. To calculate the avoidable OM rate, we analyzed those patients who underwent negative or non-therapeutic laparotomy. The remaining patients, who had been managed with active clinical observation, angioembolization or exploratory (non-therapeutic) LPS, were included in the SNOM group. The most frequent indication for exploratory LPS was to exclude peritoneal penetration, hollow viscus injury, or diaphragmatic injury in cases with trauma to the thoracoabdominal region. Therapeutic LPS included the application of adhesive substances and hemostatic agents, sutures of hollow viscus injuries and diverting colostomies, among other procedures. The absolute contraindication for LPS was hemodynamic instability. Relative contraindications included third-trimester pregnancies, multiple previous laparotomies, chronic cardiorespiratory disease, and lumbar SW. SNOM failure was defined as the need for urgent or deferred surgery in a patient previously subjected to SNOM, either due to an inadvertent lesion during the exploratory LPS, or due to poor progress during clinical observation or after interventional procedures.
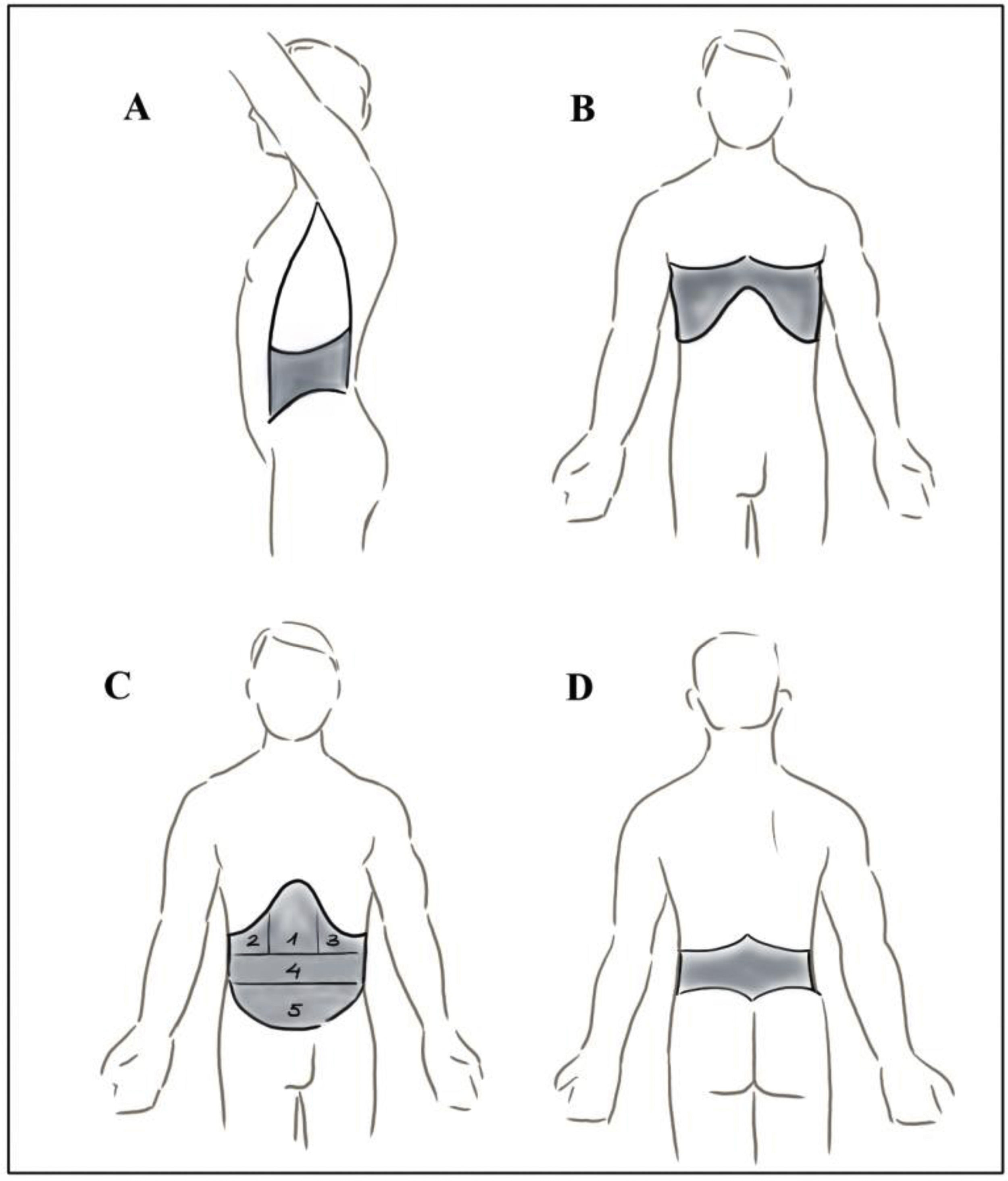
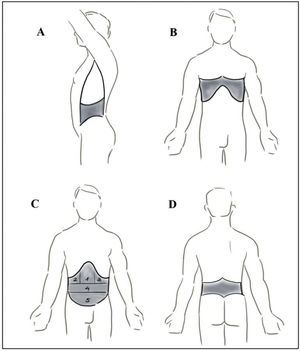
From a clinical point of view, we have classified the penetrating abdominal SW according to their anatomical location (Fig. 1): anterior abdomen (from the costal margins to the pubis and inguinal ligaments, between the anterior axillary lines); the flanks (between the anterior and posterior axillary lines, costal margin and iliac crest); posterior or lumbar abdomen (between the posterior costal margins, iliac crests, and posterior axillary lines); and right and left thoracoabdominal region (from the nipple line to the costal margins in front, and the tips of the scapulae and costal margins behind). In turn, in the anterior abdomen, 5 anatomical locations were considered: epigastrium, right hypochondrium (RH), left hypochondrium (LH), mesogastrium, and hypogastrium. The reason for considering these 5 locations in the anterior abdomen stems from the fact that, especially in the early years, SW located in the mesogastrium and hypogastrium were referred to in this way in our registry; furthermore, these are locations with, a priori, a greater need for surgical intervention due to the frequency of intestinal injuries. Finally, the patients who presented multiple wounds were classified considering the anatomical location of the wound that presumably caused the main injury; however, a separate category was created for that subgroup.
We have evaluated the severity of the patients using the Injury Severity Score (ISS) and the Revised Trauma Score (RTS). Within the ISS, we have established 4 severity ranges: 1−15 (mild-moderate), 16−24 (serious), 25−39 (very high risk) and 40−75 (uncertain survival). Within the RTS, despite being a quantitative variable and given that the vast majority of patients in both groups had a score of 12, we have established two categories: ≤11 and 12, making it a qualitative variable.
For the statistical analysis, the SPSS 20.0 program for MacOS was used. The association between qualitative variables was evaluated with the chi-squared test or Fisher’s exact test. For the comparison of quantitative variables with a normal distribution, the Student’s t test was used for independent samples. In the event that the variable did not fit this distribution, the non-parametric Mann–Whitney U test was used. Statistical significance was based on a P-value <.05.
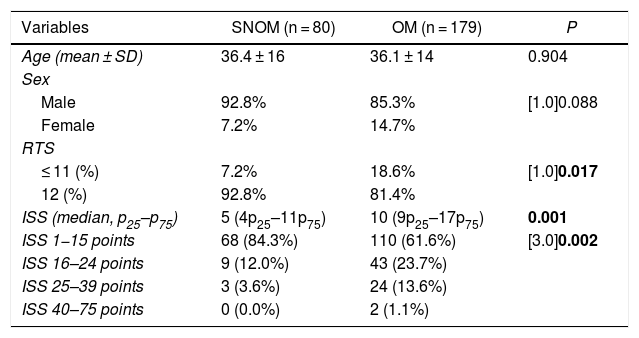
ResultsWe identified 259 patients who met the inclusion criteria. Table 1 describes demographic data and differences in the severity scores between the OM and SNOM groups, with statistically significant differences. Subdividing the ISS into 4 categories confirmed the greater anatomical severity of patients undergoing OM.
Demographic data and severity scores in both groups.
| Variables | SNOM (n = 80) | OM (n = 179) | P |
|---|---|---|---|
| Age (mean ± SD) | 36.4 ± 16 | 36.1 ± 14 | 0.904 |
| Sex | |||
| Male | 92.8% | 85.3% | [1.0]0.088 |
| Female | 7.2% | 14.7% | |
| RTS | |||
| ≤ 11 (%) | 7.2% | 18.6% | [1.0]0.017 |
| 12 (%) | 92.8% | 81.4% | |
| ISS (median, p25–p75) | 5 (4p25–11p75) | 10 (9p25–17p75) | 0.001 |
| ISS 1−15 points | 68 (84.3%) | 110 (61.6%) | [3.0]0.002 |
| ISS 16–24 points | 9 (12.0%) | 43 (23.7%) | |
| ISS 25–39 points | 3 (3.6%) | 24 (13.6%) | |
| ISS 40–75 points | 0 (0.0%) | 2 (1.1%) |
SD: standard deviation; OM: operative management; SNOM: selective non-operative management; RTS: Revised Trauma Score; ISS: Injury Severity Score. 1−15: mild-moderate. 16−24: severe. 25−39: very high life risk. 40−75: survival uncertain.
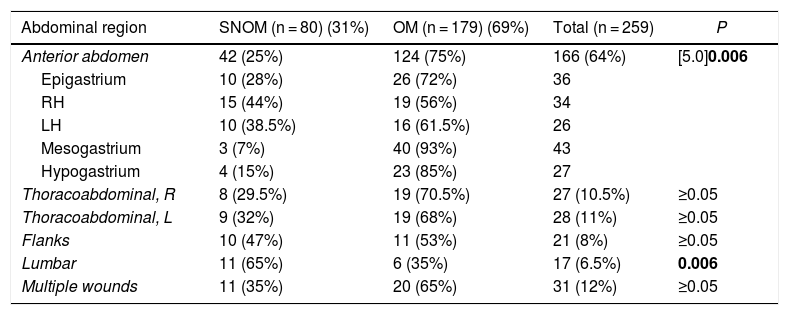
Table 2 shows the percentages of OM and SNOM depending on the anatomical location of the abdominal SW. The SNOM was applied to 31% of the patients and was more frequent in the flanks and lumbar region, with statistically significant differences being observed in the latter region compared to OM. We operated on 75% of the patients with penetrating SW in the anterior abdomen, which showed statistically significant differences versus SNOM. In this region, SNOM was more used in the RH, followed by the LH and epigastrium, but no statistically significant differences were found. Approximately 1 in 3 patients with multiple thoracoabdominal SW were managed with SNOM.
Percentages of OM and SNOM depending on the anatomical location of abdominal SW.
| Abdominal region | SNOM (n = 80) (31%) | OM (n = 179) (69%) | Total (n = 259) | P |
|---|---|---|---|---|
| Anterior abdomen | 42 (25%) | 124 (75%) | 166 (64%) | [5.0]0.006 |
| Epigastrium | 10 (28%) | 26 (72%) | 36 | |
| RH | 15 (44%) | 19 (56%) | 34 | |
| LH | 10 (38.5%) | 16 (61.5%) | 26 | |
| Mesogastrium | 3 (7%) | 40 (93%) | 43 | |
| Hypogastrium | 4 (15%) | 23 (85%) | 27 | |
| Thoracoabdominal, R | 8 (29.5%) | 19 (70.5%) | 27 (10.5%) | ≥0.05 |
| Thoracoabdominal, L | 9 (32%) | 19 (68%) | 28 (11%) | ≥0.05 |
| Flanks | 10 (47%) | 11 (53%) | 21 (8%) | ≥0.05 |
| Lumbar | 11 (65%) | 6 (35%) | 17 (6.5%) | 0.006 |
| Multiple wounds | 11 (35%) | 20 (65%) | 31 (12%) | ≥0.05 |
SW: stab wounds; RH: right hypochondrium; LH: left hypochondrium; OM: operative management; SNOM: selective non-operative management.
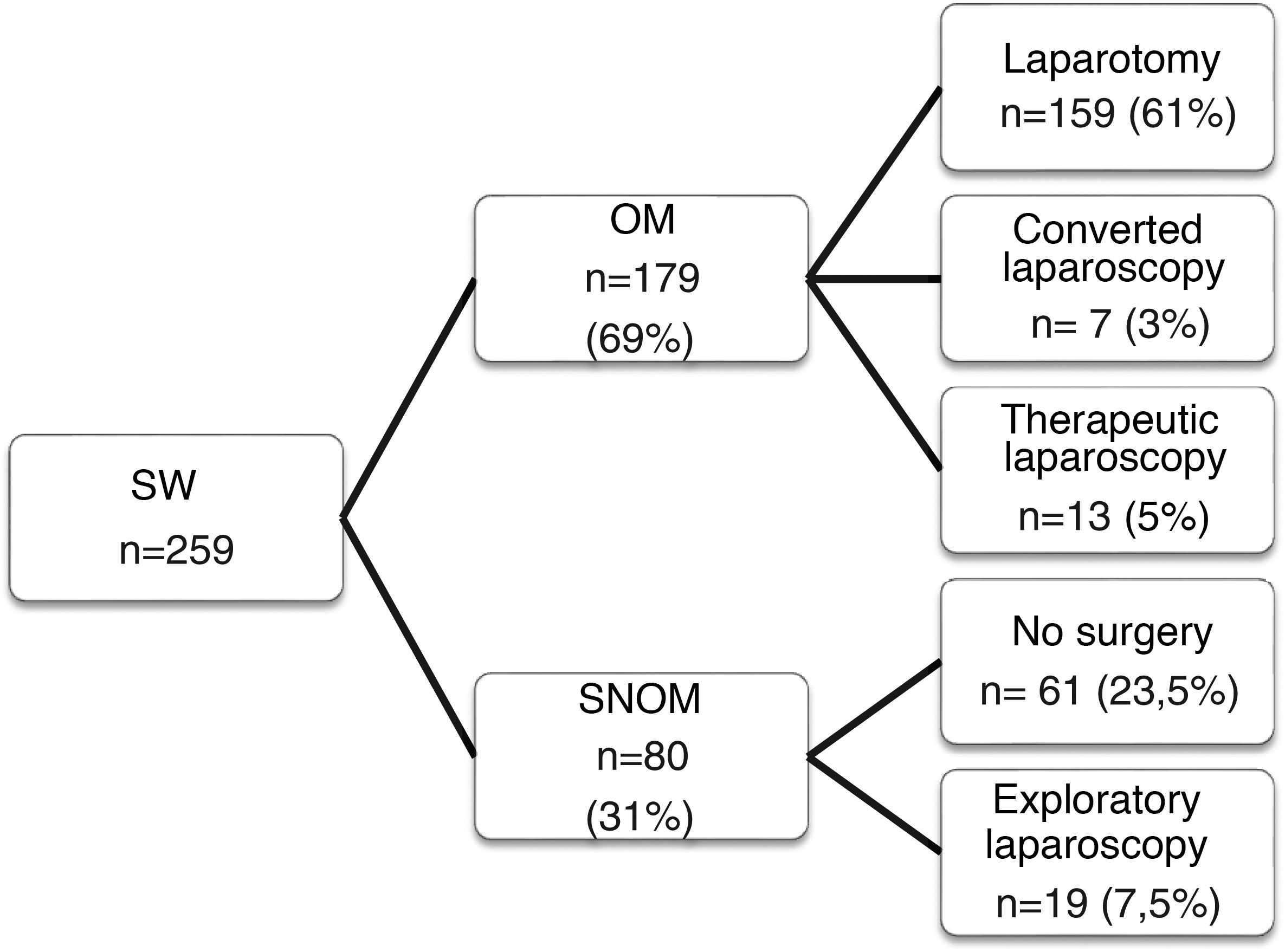
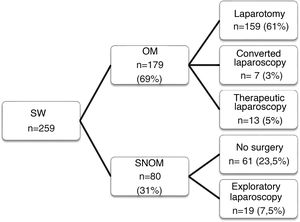
Fig. 2 summarizes the distribution of patients according to the type of management received, showing that almost one-third were managed with SNOM. Within this group, arteriography was performed in 14 patients, 9 (11%) of whom underwent angioembolization due to active bleeding: 4 due to renal lacerations, one adrenal injury, 2 iliolumbar hemorrhage, one circumflex artery bleed, and one liver laceration. In total, 19 exploratory LPS were performed, all of them with no associated morbidity. The success rate of SNOM was 96%. Among the 80 patients managed with this approach, only 3 cases (3.5%) later required urgent or deferred surgery. Two were due to undetected injuries to the small intestine and colon during in the exploratory LPS of a left thoracoabdominal and mesogastric wound, and the third due to failure of conservative management of a grade III splenic laceration in a patient with an LH wound. All 3 underwent laparotomy, with no additional complications or mortality.
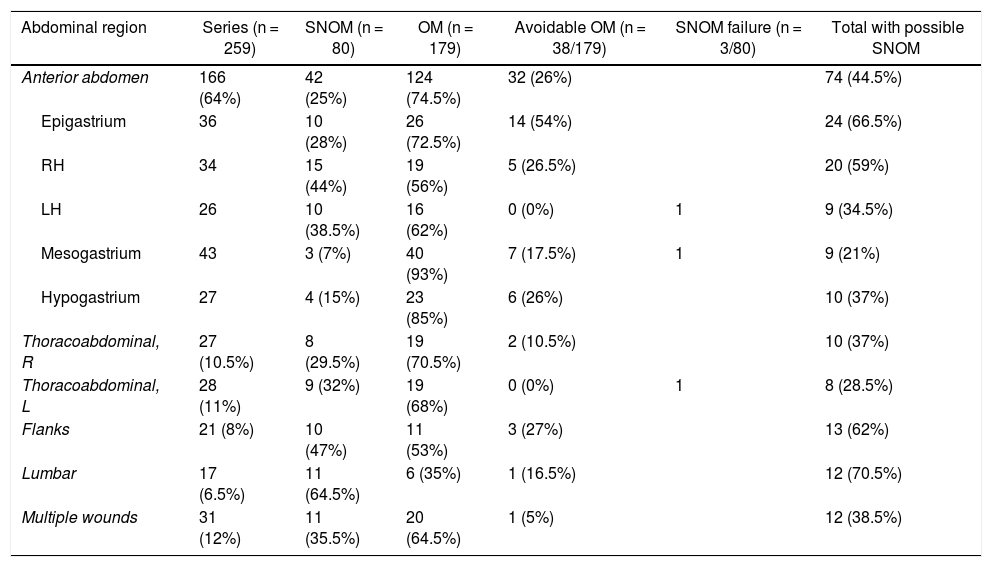
Table 3 reflects the rates of negative, avoidable or non-therapeutic laparotomies depending on the location, this overall percentage being 21% (38/179). In the anterior abdomen, there was a high number of avoidable laparotomies in the epigastrium (54%), followed by the RH (26.5%) and hypogastrium (26%). Likewise, approximately one out of every 4 laparotomies due to SW in the flanks could have been avoided. This OM was less avoidable in thoracoabdominal SW as well as the LH and mesogastrium. The associated morbidity entailed 2 wound infections, 2 eviscerations, and 2 prolonged ileus.
Potential SNOM, according to anatomical location.
| Abdominal region | Series (n = 259) | SNOM (n = 80) | OM (n = 179) | Avoidable OM (n = 38/179) | SNOM failure (n = 3/80) | Total with possible SNOM |
|---|---|---|---|---|---|---|
| Anterior abdomen | 166 (64%) | 42 (25%) | 124 (74.5%) | 32 (26%) | 74 (44.5%) | |
| Epigastrium | 36 | 10 (28%) | 26 (72.5%) | 14 (54%) | 24 (66.5%) | |
| RH | 34 | 15 (44%) | 19 (56%) | 5 (26.5%) | 20 (59%) | |
| LH | 26 | 10 (38.5%) | 16 (62%) | 0 (0%) | 1 | 9 (34.5%) |
| Mesogastrium | 43 | 3 (7%) | 40 (93%) | 7 (17.5%) | 1 | 9 (21%) |
| Hypogastrium | 27 | 4 (15%) | 23 (85%) | 6 (26%) | 10 (37%) | |
| Thoracoabdominal, R | 27 (10.5%) | 8 (29.5%) | 19 (70.5%) | 2 (10.5%) | 10 (37%) | |
| Thoracoabdominal, L | 28 (11%) | 9 (32%) | 19 (68%) | 0 (0%) | 1 | 8 (28.5%) |
| Flanks | 21 (8%) | 10 (47%) | 11 (53%) | 3 (27%) | 13 (62%) | |
| Lumbar | 17 (6.5%) | 11 (64.5%) | 6 (35%) | 1 (16.5%) | 12 (70.5%) | |
| Multiple wounds | 31 (12%) | 11 (35.5%) | 20 (64.5%) | 1 (5%) | 12 (38.5%) |
RH: right hypochondrium; LH: left hypochondrium; SNOM: selective non-operative management; OM: operative management.
For each anatomical location, if we analyze the patients with satisfactory SNOM versus patients who underwent avoidable laparotomies (Table 3), the SW in which SNOM would have been safest are the lumbar injuries, followed by those in the epigastrium, flanks and RH.
Five patients presented evisceration of the small intestine, and all underwent laparotomy, which was justified in 4 (80%); 20 patients had a protruding omentum, only 9 of which (45%) had lesions secondary to surgery. In 2, exploratory LPS was performed, and the rest underwent laparotomy.
DiscussionThe use of selective non-operative management of SW penetrating the abdomen has been well established,8–10 although we have found no studies correlating SNOM rates with the different anatomical regions of the abdomen.11 Throughout the 1990s, new diagnostic-therapeutic approaches were introduced based on emerging technologies, such as LPS, CT and, to a lesser extent, ultrasound and angioembolization. The debate has continued to focus on the balance between invasion, use of resources, and timely repair of major injuries.12 Our 96% success rate for SNOM confirms this, even though exploratory LPS and angioembolization have been included in this SNOM rate. In our experience, angioembolization is a very useful therapeutic tool, and it was used in 11% of our patients with SNOM. Exploratory LPS has progressively found its place in the SNOM of penetrating abdominal SW in stable patients with no signs of peritoneal injuries,13,14 and there are groups that routinely recommend it in these patients to assess the possible violation of the peritoneum and potential injuries.15,16 In our review, we have considered exploratory (non-therapeutic) LPS within the SNOM group in a way similar to blunt trauma, especially to the liver, where deferred LPS is considered by some to be a fundamental component of SNOM, despite requiring general anesthesia.15,17 The main drawback of exploratory LPS is undetected lesions, although a very significant decrease in their incidence has been reported in the last decade, from 13% to 0.12%.16 Some publications have reported a significant increase in mortality associated with delayed diagnosis and treatment due injuries not detected during SNOM,18 something that we have not observed in our series, where we only had 3 SNOM failures (3.5%) that required deferred urgent surgery.
Certain potential anatomical locations for SNOM, such as thoracoabdominal SW, present particularities that support routine evaluation by LPS (or thoracoscopy), especially on the left side.19 The low diagnostic performance of CT to exclude diaphragm injuries, and the frequency of associated injuries when the diaphragm is injured, make the use of minimally invasive surgery recommendable since generally around 25% of asymptomatic patients with thoracoabdominal SW have perforation of the diaphragm.20,21 In the right thoracoabdominal region, the diaphragm is ‘protected’ by the liver, and in most cases SNOM is possible, although it may include angioembolization of liver injuries that are actively bleeding, which provides a high success rate and low rate of complications.
Penetrating SW in the lumbar region have a lower probability of significant injuries. CT, without the need for triple contrast, is considered the gold standard for its evaluation,22 and SNOM is considered a prudent and safe approach in most cases.23 In our series, 64.7% of penetrating lumbar SW were treated with SNOM, a percentage that could increase to 70.5% because one non-therapeutic laparotomy was also performed.
Multiple SW have a higher risk of intra-abdominal injury, and the internationally accepted ‘clinical follow-up’ protocol may not be appropriate in the treatment of this subgroup of patients.24 In our series, SNOM was performed in 35% of these patients, and there were no failures; in fact, there was only one avoidable laparotomy, which leads us to believe that SNOM is a feasible option in this scenario in well-selected patients.
Our 21% rate of avoidable laparotomies is consistent with published data,25 and most were performed on wounds located in the flanks, epigastrium, RH, and hypogastrium, so the potential use of SNOM would be very high, as shown in Table 3.
Regarding the controversy over the possibility of SNOM for evisceration of the omentum or viscera in SW of the anterior abdomen, a majority of authors consider visceral evisceration an indication for laparotomy or LPS, since most patients will have some type of associated injury.25,26 A minority, however, defends selective observation in these cases.27 All our patients with bowel evisceration underwent laparotomy, which was justified in 80%. The presence of associated injuries is much lower in evisceration of the omentum, and routine laparotomy also has detractors and defenders, although in recent years the use of SNOM seems to prevail in selected cases; only 45% (9/20) of our patients with evisceration of the omentum had lesions requiring surgery.
The mild-to-moderate severity of most of our patients is reflected in the severity scores, and likewise the greater need for OM in the more severe patients.
The limitations of this study include its retrospective nature and the long time period analyzed, with modified management algorithms based on new technologies, as well as different management criteria based on the large number of surgeons involved. In addition, in the small group of patients with multiple SW, the interpretation of the location of the main wound was subjective in several cases, as it was not well described in the operative report.
In conclusion, selective non-operative management of penetrating abdominal stab wounds is perfectly justified from the epidemiological and clinical point of view. In our experience, it has been safer and applicable in injuries located in the lumbar regions, flanks, epigastrium and RH. In light of the rates of avoidable laparotomy according to anatomical location, OM has been less avoidable in wounds of the left thoracoabdominal region, LH, and mesogastrium.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Tudela Lerma M, Turégano Fuentes F, Pérez Díaz MD, Rey Valcárcel C, Martín Román L, Ruiz Moreno C, et al. Relación entre la localización anatómica y el manejo selectivo no operatorio de las heridas por arma blanca penetrantes en abdomen. Cir Esp. 2022;100:67–73.