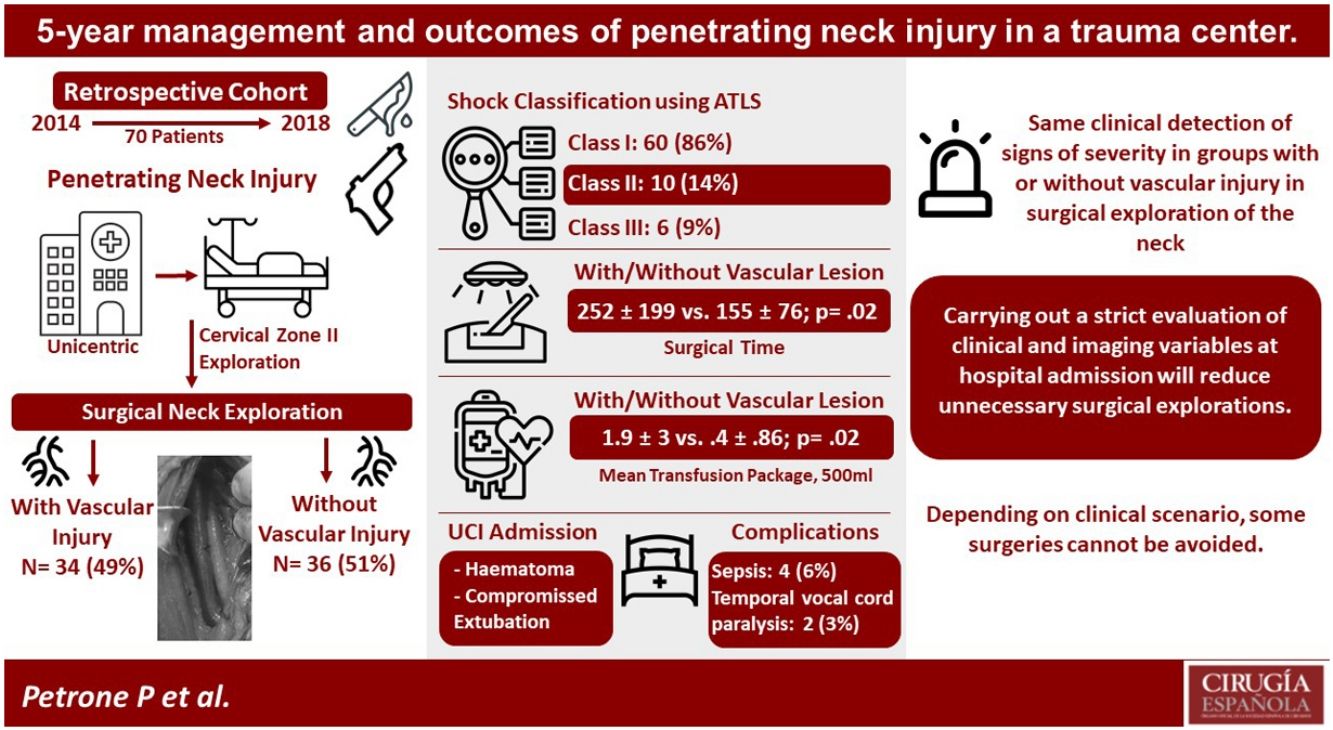
Penetrating neck injuries represent 5–10% of all traumatic injuries, these bring with them a high rate of morbidity and mortality due to vital structures that could be injured in this area. The aim of this study was to determine the epidemiological and clinical characteristics of penetrating neck injuries.
MethodsThis was a retrospective, unicentric and descriptive study that included all patients who underwent neck exploration surgery.
ResultsA total of 70 neck exploration cases were reviewed, 34 (49%) didn’t had any injury. Thirty (43%) had at least one hard sign, 42 (60%) patients showed at least one soft sign. Statistical analysis showed only surgical time (252±199.5 vs. 155±76.4; p=0.020) and transfusions (1.87±3 vs. 0.4±0.856; p=0.013) were statistically significant. We report a mortality of 2 (3%) patients.
ConclusionsOur prevalence of neck surgical exploration without vascular injury was slightly higher (49% vs. 40%) than literature. We highlight the importance of not performing neck explorations in all patients who present a penetrating injury. We did not obtain differences between groups for hard signs and soft signs. We were not able to identify whether or not there would be an injury based on clinical characteristics. Imaging studies should be performed to avoid unnecessary neck explorations; however, depending on the clinical scenario some surgery cannot be avoided.
Las lesiones penetrantes de cuello representan entre el 5-10% de todas las lesiones traumáticas, estas traen consigo una alta tasa de morbimortalidad por estructuras vitales que podrían lesionarse en esta área. El propósito de este estudio fue determinar las características epidemiológicas y clínicas del trauma penetrante de cuello.
MétodosEstudio retrospectivo, unicéntrico y descriptivo que incluyó a todos los pacientes sometidos a cirugía de exploración de cuello.
ResultadosSe revisaron un total de 70 casos de exploración de cuello, 34 pacientes (49%) no presentaron ninguna lesión. Treinta pacientes (43%) tenían al menos un signo duro, 42 pacientes (60%) mostraron al menos un signo blando. El análisis estadístico mostró que solo el tiempo quirúrgico (252±199,5 vs. 155±76,4; p=0,020) y las transfusiones (1,87±3 vs, 0,4±0,856; p=0,013) fueron estadísticamente significativas. Reportamos la mortalidad de 2 pacientes (3%).
ConclusionesNuestra prevalencia de exploración quirúrgica de cuello sin lesión vascular fue ligeramente superior (49 vs. 40%) que la literatura. Destacamos la importancia de no realizar exploraciones de cuello en todos los pacientes que presentan una lesión penetrante. No obtuvimos diferencias entre grupos para signos duros y signos blandos. No pudimos identificar si hubiera o no una lesión en función de las características clínicas. Se deben realizar estudios de imagen para evitar exploraciones innecesarias del cuello; sin embargo, dependiendo del escenario clínico, no se pueden evitar algunas cirugías.
Penetrating neck injuries (PNI) represent 5–10% of all traumatic injuries, these bring with them a high rate of morbidity and mortality due to vital structures that could be injured in this area.1
The neck is divided into 3 anatomical areas: I (upper edge of the collarbone to the lower edge of the cricoid cartilage), II (lower edge of the cricoid cartilage to the angle of the jaw) and III (angle the jaw to the skull base).2,3 Any injury that passes the platysma between the lower edge of the mandible and the skull base, and the top edge of the clavicle and the seventh cervical vertebra is defined as a PNI.
A PNI can damage the upper airway (trachea and larynx), the upper digestive tract (hypopharynx and cervical esophagus), the vascular system (carotid, jugular, subclavian, and vertebral vessels), organs (thyroid, parathyroid and salivary), the skeletal system (spine, base of skull, clavicle, sternum and jaw), and the nervous system (spinal cord and nerve plexus).4
PNIs caused by gunshot wounds (GSW) account for 50%, stab wounds (SW) 10–20%, shotgun wounds 4% and by other weapons 12%.5 The classic “hard” signs of arterial injury are pulsatile bleeding, expanding hematoma, a carotid “thrill”, an audible murmur. Soft signs include peripheral nerve deficit, history of hemorrhage at scene, a reduced but palpable pulse or an injury in proximity to a major artery.6 Surgical exploration is used for PNI care; however, this management is associated with a high incidence of surgery without an internal injury in 16–75% of cases.7–9
The aim of this study was to determine the clinical and management outcomes of PNIs. A secondary objective was to compare those with and without confirmed associated injury.
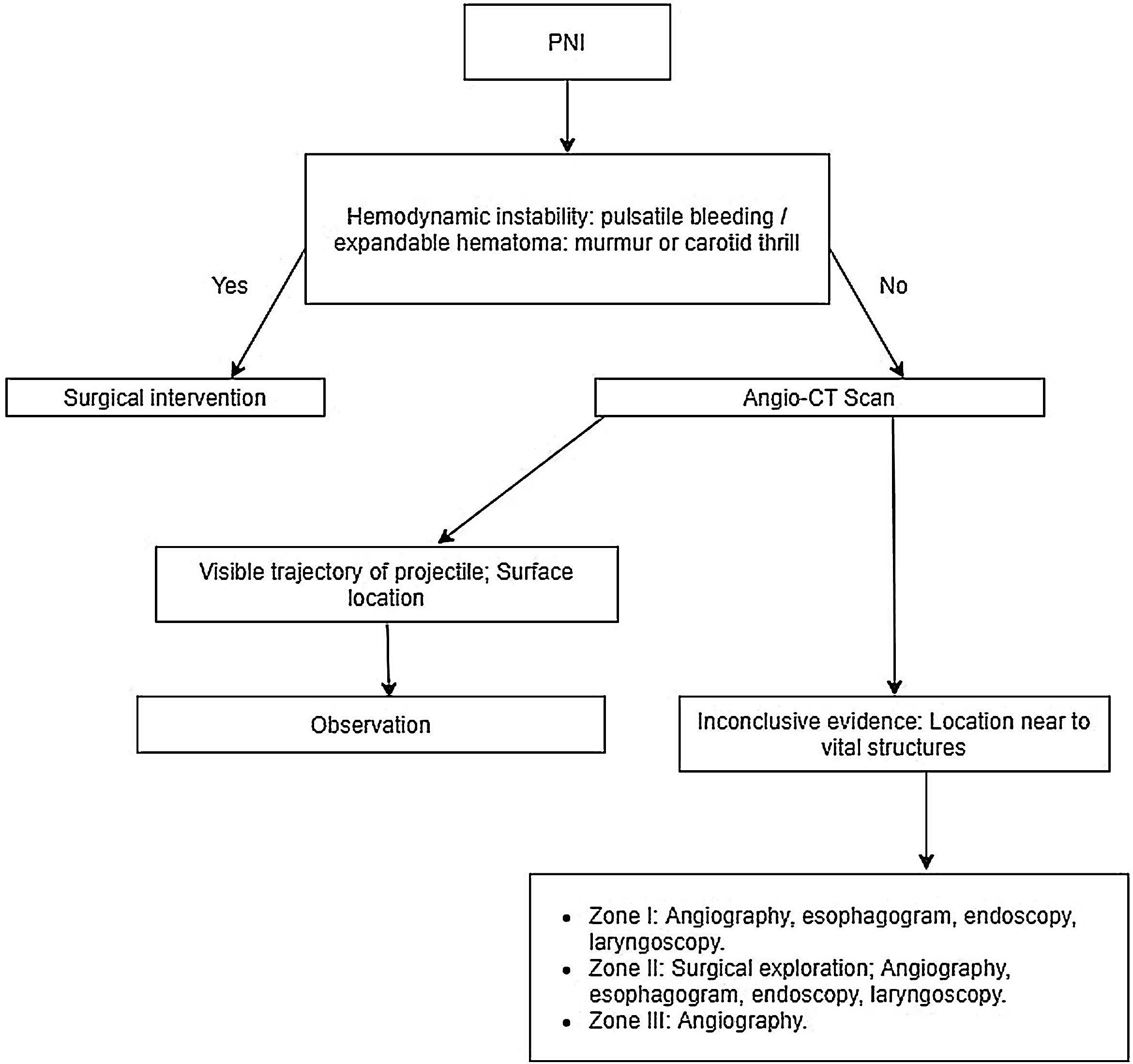
Material and methodsThis was a retrospective, unicentric and descriptive study that was carried out between 2014 and 2018 at the Emergency Department of the University Hospital of Universidad Autónoma de Nuevo Leon (UANL). It included all patients who underwent neck exploration surgery obtained from the Statistics Department. This study was approved by the ethics committee of the Faculty of Medicine of UANL. Exclusion criteria were the absence of a clinical record or under 18 years of age. The criteria used for neck exploration were: Penetrating injury in zone II, presence of hard signs, hemodynamic instability, compromised airway or CT confirmed injury (Fig. 1).
Penetrating neck injury diagnostic and treatment algorithm. PNI; penetrating neck injury. CT; computer tomography.1
Penetrating injury in zone II is between lower edge of the cricoid cartilage and the angle of the jaw. Our study used the Clavien-Dindo classification for surgical complications.10 Multiple clinical, epidemiological, and surgical variables as age, sex, hospitalization days, type of injury, outcomes, transfusions, complications, etc. were reviewed. Injury severity score (ISS) standardizes severity of traumatic injury based on worst injury of body systems. Hemodynamic shock classification was based on the Advanced Trauma Life Support (ATLS) guidelines, defining class I as <15% of approximate blood loss, 15–30% (Mild) as class II, 31–40% (Moderate) as class III and >40% as class IV.
Emergency room to operation room (ER-OR) time was defined as the time between patient arrival to emergency room until surgical start time. Hard signs (indicates immediate surgery) of neck injury means presence of shock, pulsatile bleeding of expanding hematoma, audible bruit of palpable thrill, airway compromise, wound bubbling and subcutaneous emphysema,11 soft signs (indicates serial examination) mean presence of history of arterial bleeding at scene, proximity of penetrating wound or blunt trauma to major artery, diminished unilateral distal pulse and small nonpulsatile hematoma.12
Statistical analysisContinuous variables are described with their mean value (standard deviation, SD). Categorical variables are presented as n (%). The mean (SD) was compared with the Mann–Whitney U test or Student's t-test depending on its normal distribution and homogeneity in the variance; the Kormorov–Smirnoff test was used to define the normal distribution of continuous variables. Categorical variables were compared with the chi-square test or Fisher's exact test. A p-value≤0.05 was considered statistically significant. The statistical analysis was developed with the SPSS 22.0 program (IBM Corporation, Armonk, NY, USA).
ResultsA total of 70 neck exploration (Fig. 2) cases were reviewed with a mean age was 33 (± 10.4) years. 66 (94%) male and 4 females (6%) were included in the study. Mean hospitalization time was 5 days, with only 6 (9%) patients staying more than 2 weeks. 40 (57%) patients were injured by GSW and 30 (43%) by SW. All patients had a Glasgow Coma Score of 15 upon arrival to the emergency room (ER). Extra-cervical injuries were observed in 12 (17%) patients.
On admission, 60 (86%) patients had class I hemorrhagic shock, 10 (14%) had class II, and 6 (9%) class III. 30 (43%) had at least one hard sign. All patients with class III shock had hard signs. Only 42 (60%) patients showed at least one soft sign. All patients were classified as grade IIIb or greater (n=70) by the Clavien-Dindo classification for intervention under general anesthesia, or greater. Eight (11%) patients were classified as grade IV for life threatening complication requiring ICU management. Two (3%) patients were on grade V after surgery (death of patient).
The total injured structures found were 12 (35%) internal jugular vein (IJV), 16 (47%) external jugular vein, 2(5.8%) carotid arteries and 4(11.7%) tracheal with IJV injuries. From this PNI injury group, details of the injured structured by type of injury can be found in Table 2. Intrahospital complications were sepsis 4 (6%) and temporal vocal cord paralysis 2 (3%). Temporal vocal cord paralysis was present in penetrating neck surgical exploration without injury and 2 (3%) dead patients showed associated sepsis.
Statistical analysis of neck explorations with and without injury.
| Total (n=70) | With injury n=34 (49%) (%) | Without injury n=36 (51%) (%) | p | |
|---|---|---|---|---|
| Mean age, years | 33 (± 10.4) | 34 (± 12.8) | 32 (± 8.2) | 0.770 |
| Sex | 0.062 | |||
| Male | 66 (94%) | 30 (88%) | 36 (100%) | |
| Type of injury | 0.241 | |||
| GSW | 40 (57%) | 16 (47%) | 24 (67%) | |
| SW | 30 (4%) | 18 (53%) | 12 (33%) | |
| Hospitalization, days | 5 (± 5.3) | 5 (± 3.4) | 5 (± 6.59) | 0.192 |
| Extra-cervical injuries | 12 (17%) | 8 (24%) | 4 (11%) | 0.258 |
| Hemodynamically unstable | 14 (20%) | 8 (22%) | 6 (16%) | 0.349 |
| Glasgow score of 15, points | 70 (100%) | 34 (100%) | 36 (100%) | 1.00 |
| ISS, mean | 21 (± 6.3) | 22 (± 6.1) | 20 (± 6.6) | 0.130 |
| Hard signs, (+)a | 30 (43%) | 16 (41%) | 14 (38%) | 0.375 |
| Soft signs, (+)a | 42 (60%) | 20 (58%) | 22 (61%) | 0.859 |
| ER-OR time, min | 120 (± 103.8) | 106 (± 71.6) | 133 (± 125.2) | 0.427 |
| Surgical time, min | 199 (± 151.4) | 252 (± 199.5) | 155 (± 76.4) | 0.020 |
| PRBCs, meanb | 1.5 (± 2.2) | 1.87 (± 3) | .4 (± .856) | 0.013 |
| Bleeding, mL | 292.4 (± 325.7) | 371 (± 412.4) | 226 (± 222.6) | 0.209 |
| Intensive care unit | 8 (11%) | 5 (15%) | 3 (8%) | 0.369 |
| Complications | 6 (9%) | 4 (11%) | 2 (5%) | 0.734 |
| Postsurgical mortality | 2 (3%) | 2 (3%) | 0 | 0.296 |
PRBCs, 500mL. Data are presented as mean (Standard Deviation) or n (%). Sepsis and temporal vocal cord paralysis are considered as postoperative complications. GSW: gunshot wound; SW: stab wound; ISS: injury severity score; ER: emergency room; OR: operation room; PRBCs, packed red blood cells. p. Statistical significance p≤0.05.
Injured neck structures.
| SW (n=30) | GSW (n=40) | |
|---|---|---|
| Internal jugular vein | 6 (20%) | 10 (25%) |
| External jugular vein | 12 (40%) | 2 (5%) |
| Carotid artery | 0 | 2 (5%) |
| Tracheal injury | 2 (6.7%) | 2 (5%) |
| Total | 20 (66.7%) | 16 (40%) |
This is the total of reported injuries; the 2 tracheal injury patients also had another vascular injury. SW: stab wound. GSW: gun-shot wound.
The mean time between the ER and OR was 120 (± 103.8) minutes. Patients with class II or III shock had shorter transfer times, with a mean of 68min, and 129min for class I. The mean operating time was 199 (± 151.4) min with a mean blood loss of 292.4 (± 325.7) mL; only 12 (27%) had a blood loss of more than 500mL. More than 6 blood transfusions were required in only 6 (8.6%) patients. Eight (11%) patients were admitted to the intensive care unit postoperatively for suffering hematoma or upper airway inflammation or edema that can compromise extubation evaluated by anesthesiology. Two (3%) deaths were reported in a patient with SW but this was associated to hospital-acquired pneumonia.
A statistical analysis comparing patients who underwent surgery and those with and without a neck injury was performed (Table 1). In this analysis, only surgical time (252±199.5 vs. 155±76.4; p=0.020) and transfusions (1.87±3 vs. 0.4±0.856; p=0.013) were statistically significant. There were no statistically significant differences between the SW, GSW groups and hard and soft signs.
DiscussionAs for our primary objective, prevalence of neck surgical exploration without vascular injury was slightly higher (49% vs. 40%) than literature.13 We highlight the importance of not performing neck explorations in all patients who present a penetrating injury. We considered that hospital emergency personnel should perform physical examination and imaging studies before considering use of a surgical neck exploration due to penetrating trauma.
In regards of the ER-OR time, we found a high average for the injured group (106±71.6 vs. 133±125.2min). According to protocol, if patients didn’t show an immediate life threatening clinical information, complete preoperative management was ensured, which could’ve prolonged these times. We found that vascular injury in the SW group are slightly more common (66% vs. 40%) because in the GSW cases if these lesions are present the likelihood of surviving is low.
For our secondary objective when comparing injury vs. no-injury PNI group we found that surgical times and transfusions were the only variables statistically significant among these groups. We did not obtain differences between groups for hard signs and soft signs. In the literature, these help to define the therapeutic plan of the patient with penetrating neck trauma, which suggests that in this study the assessment of these signs could be complicated by surgeons, so they opted in most cases in performing exploratory neck surgery despite the probable lack of hard signs. We did not find evidence on the understanding during hospital practice of hard and soft signs to prevent unnecessary surgical procedures.
Imaging studies are preferred while there are no absolute signs of emergency to avoid unnecessary procedures as several studies have proven the effectiveness of CT angiography to eliminate non-therapeutic neck surgical procedures14–16 since it has been shown to be a fast, safe and effective method to evaluate patients with penetrating neck trauma.17,18
There is evidence in the literature that indicates a greater surgical sensitivity to vascular and muscular injuries due to penetrating neck trauma than just using CT scan,19 this difference is greater when talking about airways injuries (6.7% for CT angiography vs. 40%; for Surgery; p=0.002) and esophageal/pharyngeal lesion (10% for CT angiography vs. 30% for surgery; p=0.013). Furthermore, due to CT scan is a non-invasive study, in the absence of hard signs, less radical options should be explored if possible, for the benefit of the patient.
Conservative or selective non-operative management (SNOM) is considered safe, in the case of the airway, repair and tracheotomy is reserved only for major destructive lesions.20 Isolated injuries with undisplaced fractures of the laryngotracheal skeleton, and lacerations of the trachea under one third of its circumference, may be offered conservative management.21
Sepsis had delayed discharge in our patients, they had even died due to it in intensive care unit. It is well known that mortality due to sepsis increases with time. Postoperative management includes antibiotics and nasogastric tube feeding to avoid complications due to infection.22,23
We reported an overall mortality of 3% versus 1.3–7.9% reported in the literature.24 Performing a neck surgical examination did not significantly increase mortality compared to previous studies. It is noteworthy that only death by SW occurred, and no arterial injuries were reported in patients with GSW. There was no statistically significant difference between the SW and GSW groups, suggesting that both groups can be managed equally.
A limitation for our study was that clinical diagnosis was made by different general surgery specialists on call, so clinical criteria for surgery could vary. Another limitation is that this study does not assess concomitant injuries nor other offered treatments.
ConclusionsWe were not able to identify whether or not there would be an injury based on clinical characteristics. Imaging studies should be performed to avoid unnecessary neck explorations; however, depending on the clinical scenario some surgery cannot be avoided.
Statement of human and animal rightsThis article does not contain any studies with human or animal subjects performed by the any of the authors.
FundingThe present investigation has not received specific aid from agencies of public sector, commercial sector or non-profit entities.
Conflicts of interestThe authors declare no conflicts of interest.
We thank Sergio Lozano-Rodriguez, M.D. for his help in editing and translating this manuscript.