The resection of hepatic metastasis (HM) of colorectal cancer increases survival, and in some cases the 5-year survival rate reaches 50%.1–4 The major problem is that only 20%–25% of HM are initially resectable, which is usually due to insufficient future remnant liver volume.4–8 In patients with initially unresectable HM, there are several strategies used to increase resectability: in situ split, neoadjuvant chemotherapy, combined surgery and radiofrequency ablation, and two-stage (TS) surgery combined with portal embolization, developed by Adam et al.1,4–8
In the first stage of TS surgery, the metastases located in the future remnant (usually the left liver) are resected.1,5–9 After portal vein ligation or embolization, the second stage of surgery involves major hepatectomy of the embolized lobe.1,5–8 TS surgeries are generally performed by means of laparotomy. However, we present our experience using laparoscopy for the first stage.
We present the results of patients who had been treated with a TS liver surgery strategy in whom the first stage involved a laparoscopic approach in the period between January 2007 and December 2012. Fifty-seven patients underwent HM, and 6 were treated with a TS strategy (10.5%). All patients had synchronous bilobar liver metastases in whom, after CT volumetry, it was determined that there would not be sufficient remnant for one-stage liver surgery (<30%).
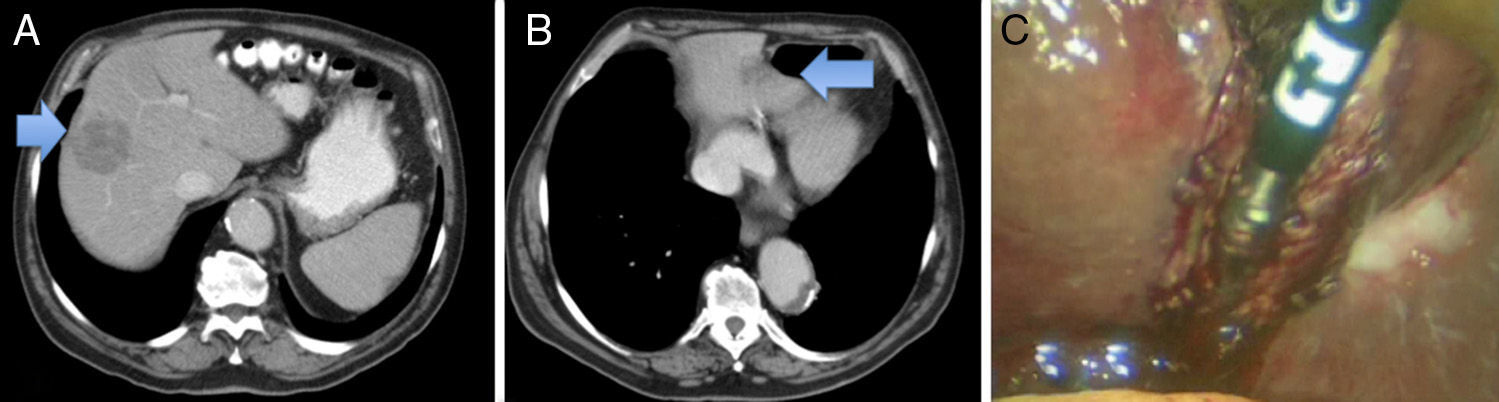
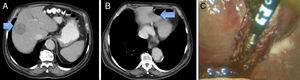
In 3 patients, the first stage of surgery was performed using a laparoscopic approach. In the remaining 3 patients, laparotomy was used due to the anatomical location of the HM. Table 1 presents the clinical characteristics of the patients who were treated by laparoscopy. All the liver resections were performed in 20° reverse Trendelenburg lithotomy position. The approach utilized 3 trocars: one 5mm in the right hypochondrium, one umbilical 11mm trocar and one 12mm in the left hypochondrium. The procedures included: 2 limited resections and 1 partial left lateral sectionectomy (Fig. 1). Afterwards, 2 trocars were added to perform the colorectal surgery.
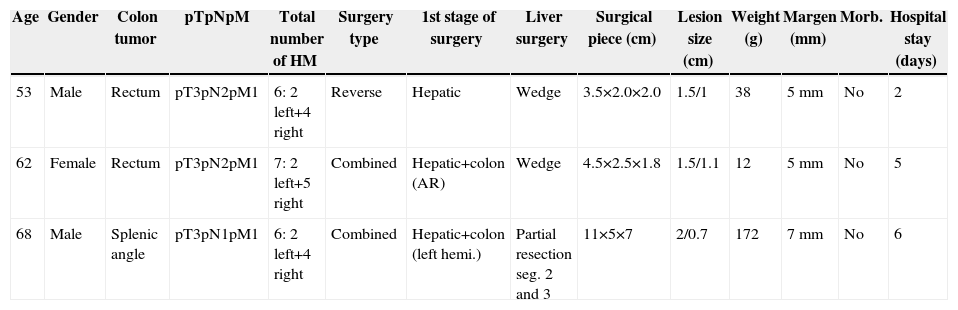
Clinical Characteristics of Patients Who Were Treated by Laparoscopy.
| Age | Gender | Colon tumor | pTpNpM | Total number of HM | Surgery type | 1st stage of surgery | Liver surgery | Surgical piece (cm) | Lesion size (cm) | Weight (g) | Margen (mm) | Morb. | Hospital stay (days) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 53 | Male | Rectum | pT3pN2pM1 | 6: 2 left+4 right | Reverse | Hepatic | Wedge | 3.5×2.0×2.0 | 1.5/1 | 38 | 5mm | No | 2 |
| 62 | Female | Rectum | pT3pN2pM1 | 7: 2 left+5 right | Combined | Hepatic+colon (AR) | Wedge | 4.5×2.5×1.8 | 1.5/1.1 | 12 | 5mm | No | 5 |
| 68 | Male | Splenic angle | pT3pN1pM1 | 6: 2 left+4 right | Combined | Hepatic+colon (left hemi.) | Partial resection seg. 2 and 3 | 11×5×7 | 2/0.7 | 172 | 7mm | No | 6 |
HM: hepatic metastasis.
In 2 patients, laparoscopic surgery of the colorectal tumor was combined with laparoscopic liver resection (anterior resection and left hemicolectomy). In the third patient, who had presented occlusive symptoms due to a rectal neoplasm, we inserted an auto-expandable stent using reverse surgery. Morbidity was 0%. The hospital stay was 2 days for the patient who only underwent liver surgery, and 5 and 6 days in the patients with combined laparoscopic colon resection. After 10 days, all 3 patients underwent percutaneous portal vein embolization, and right hepatectomy was performed one month later using laparotomy. In the second stage, the number of intraabdominal adherences was minimal and hilar dissection was difficult.
It has been demonstrated that laparoscopic hepatectomies used to treat malignant lesions involve less bleeding, shorter hospitalizations and fewer complications. Quality of life is better than after laparotomy, with the same efficacy and oncologic safety.1,3,4,10
There are very few published cases of totally/partially laparoscopic TS surgeries. In 2010, Machado et al. and Jain et al. published almost simultaneously one totally laparoscopic TS surgery each.1,4 Later, in 2012, Robles et al. published another 2 totally laparoscopic TS procedures.8 The longest reported experience is that of a series of 8 partially/totally laparoscopic TS strategies, 5 with an initial laparoscopic stage and a second laparotomy stage, one conversion to laparotomy, and only 2 completely laparoscopic cases.6
The first stage of TS can usually be completed laparoscopically as it generally entails minor hepatectomy of the left liver, which may or may not be associated with colon surgery and/or right portal vein ligation.2,6,11 Although it is feasible and provides good results, laparoscopic right portal ligation has been done in few patients.2 The advantages of an initial laparoscopic stage are: fewer intraabdominal adherences (but not hilar), correct staging, less pain, shorter hospitalization, faster recuperation, and maintained abdominal wall integrity.1,6,9 The second part of TS (major hepatectomy) can be done using either laparoscopy or laparotomy, but major laparoscopic hepatectomies require a high level of technical skill, and their use still has not become widespread.3,6
Another point of debate is combined laparoscopic hepatic and colorectal surgery. Classically, in patients with synchronous HM, combined surgery was not performed as it was argued to have higher morbidity and mortality than sequential procedures, especially in rectal tumors or major hepatectomies.8,9 However, sequential surgeries also present disadvantages: longer hospitalization, 2 anesthesia times, delayed chemotherapy, etc.9 Several series have demonstrated that combined and sequential surgeries obtain similar results. Furthermore, if combined surgery is not used in patients with two-stage surgery, then 3 surgeries are needed.5 In 2010, Karoui et al. published a series of 33 patients with exclusively TS combined surgeries, which gave good results (morbidity 21% and mortality 0%).5,8,9 The combined laparoscopic approach of colorectal tumors and HM has certain advantages, including simpler access to both intraabdominal regions, abdominal wall preservation, postoperative recovery, hospital stay, tumor staging, etc., as well as no increase in morbidity or mortality and shorter hospital stay. Even so, it has not become popular.5,8–10
In conclusion, the laparoscopic approach of the first stage in two-stage liver surgery is feasible and provides certain benefits. The combination of colon surgery and minor laparoscopic hepatectomy is safe and also provides certain advantages.
Please cite this article as: Ramia JM, Adel F, de La Plaza R, Veguillas P, García-Parreño J. Primer tiempo laparoscópico en una cirugía hepática en 2 tiempos. Cir Esp. 2015;93:125–127.