Pudendal neuralgia (PN) is an underdiagnosed chronic, disabling condition.
The diagnosis is not always straightforward, as the pelvic region is an area of confluence of several nerve trunks. Its difficult diagnosis and the fact that it is a relatively rare pathology often lead to a late diagnosis.
This condition affects women more frequently, and the average time for diagnosis is about 4 years, after a succession of consultations with different specialists.1 The International Pudendal Neuropathy Association estimates an incidence of 1/100 000, although this number could be significantly higher.
The pudendal nerve originates from the S2, S3, and S4 roots. It is a motor, autonomic and sensitive nerve responsible for the sensitivity of the perianal and genital region as well as the motor innervation of the anal and bladder sphincters. It has 3 branches: perineal, rectal and distal, which is the dorsal of the penis in men and the dorsal of the clitoris in women.
PN is also known as pudendal nerve entrapment syndrome. It is produced by compression of the pudendal nerve along its pathway and at the exit or entrance of the pelvis by any of the surrounding osteo-musculotendinous or vascular structures.2
PN can be due to prolonged compression (cyclists or professional drivers), secondary to previous surgeries, vascular compression, or endometriosis. In 70% of patients, the nerve is trapped in the ‘clamp’ formed by the sacrospinous and sacrotuberous ligaments, in 18% it is entrapped in Alcock’s canal, and in 10% the nerve rides on the falciform process of the sacrotuberous ligament.
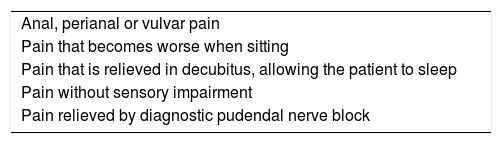
Symptoms are defined by the Nantes criteria (Table 1), described by Labat in 20083: pain in the perineal or perianal region that worsens upon sitting, is relieved when standing or lying down, and does not interrupt sleep.1,2 CT-guided pudendal nerve block confirms diagnosis.3
We present our experience in laparoscopic pudendal neurolysis, with a description of the technique and its results.
Once the diagnosis is confirmed in our Pudendal Nerve Unit, the patients are treated with neuromodulators and epidural intracanal pulsed radiofrequency.
When the response to radiofrequency is poor, pudendal nerve decompression surgery is indicated.
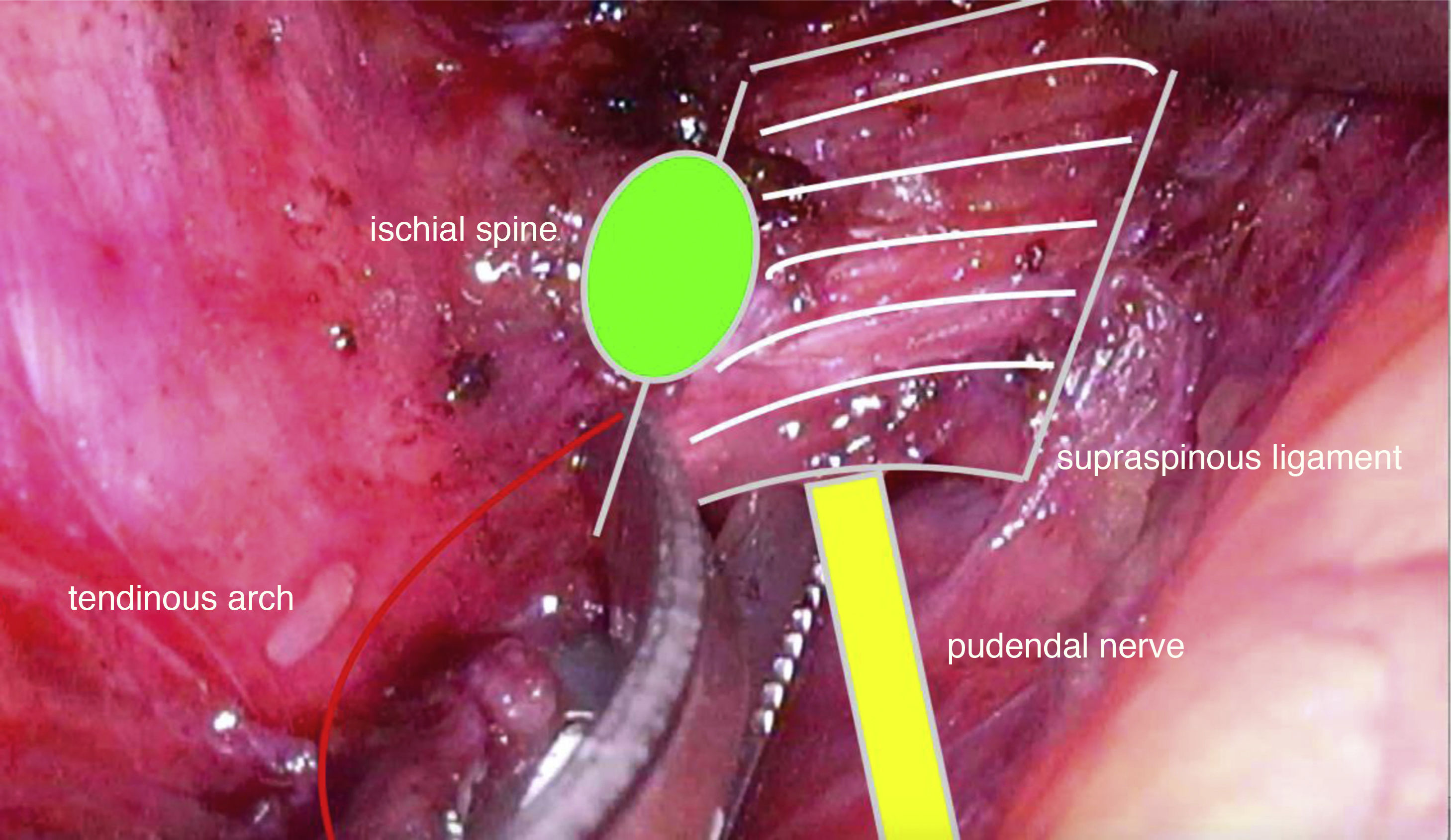
We use the laparoscopic approach (4 trocars, patient in Trendelenburg) and access the obturator foramen through an incision to the peritoneum between the common iliac vein and the umbilical artery. Progress is made caudally by identifying the obturator nerve and obturator vein, and medially by rejecting the surrounding fatty tissue. The tendinous arch and the ischial spine are viewed and, after dividing fibers of the coccygeal muscle, the sacrospinous ligament is identified, which inserts into the ischial spine and extends medially. Below the ligament and close to the spine, we then identify the pudendal neurovascular bundle.
The entire ligament is divided (Fig. 1) until fatty tissue is reached, which indicates the entry into the Alcock canal, and the mobilization of the pudendal nerve is verified.
Surgical treatment has been shown to be the most effective and definitive in the management of PN with intractable pain.
At least 5 approaches have been published in the literature.
The transperineal approach was described by Shafik in 19914 and the transvaginal approach by Bautrant in 20035; both techniques are practically blind and very personal. These authors report success rates between 62% and 70%.
The transgluteal approach was described by Robert, and it is the only approach supported to date by randomized studies6 with a success rate of 71%. Technically, it is very demanding, limiting its action to ligamentous impingement, and potential sequelae include fibrosis and persistent pain.
The robotic approach shares the same access as the laparoscopic technique and improves it in terms of image and dexterity.
The laparoscopic approach, described by Possover in 2004,7 provides an excellent view of the nerve plexuses with great definition. It therefore provides the ability to simultaneously diagnose and resolve other causes of neurological compression, such as endometriosis and postoperative fibrosis. In a series of 134 patients, Possover achieved improvement in 83% of patients.
Between March 2018 and December 2019, we performed 6 laparoscopic pudendal neurolysis procedures in 5 patients. Four patients underwent unilateral neurolysis and one patient a bilateral procedure in 2 independent interventions. All patients were female, and the mean duration of their symptoms was 4 years (2–8).
The mean operative time was 65 min (40–80). The postoperative stay was between 24 and 72 h. We had no relevant complications.
Pain intensity was measured by the visual-analog scale before surgery, in the postoperative period, and after 6 months.
In 5 out of the 6 procedures, the patients presented a reduction in pain intensity of at least 50%, which was maintained 6 months later.
In our experience, laparoscopic neurolysis of the pudendal nerval has been shown to be a minimally invasive technique that is technically feasible and safe. It provides for excellent exploration of the neurological structures of the presacral and obturator regions, as well as precise dissection of the pudendal nerve.
Please cite this article as: Moncada E, Vigorita V, de San Ildefonso A, Sánchez Santos R. Neurólisis laparoscópica para el tratamiento de la neuralgia del pudendo. Cir Esp. 2021;99:541–543.