The main step in curative treatment for breast cancer is surgery. Its use in an ambulatory setting can contribute toward more efficient healthcare, providing additional benefits for patients. In this study, we analyze the results obtained with this treatment method and identify factors related with conversion to hospitalization.
MethodsResults were analyzed from the 206 surgeries performed for breast cancer in 2016, using three different methods: day surgery, overnight ambulatory (23h) and conventional hospitalization. The ambulatory success and conversion rates were calculated for the global sample and stratified, distinguishing between conservative surgery, mastectomy and axillary surgery. A univariate analysis was performed to identify the factors involved in conversion.
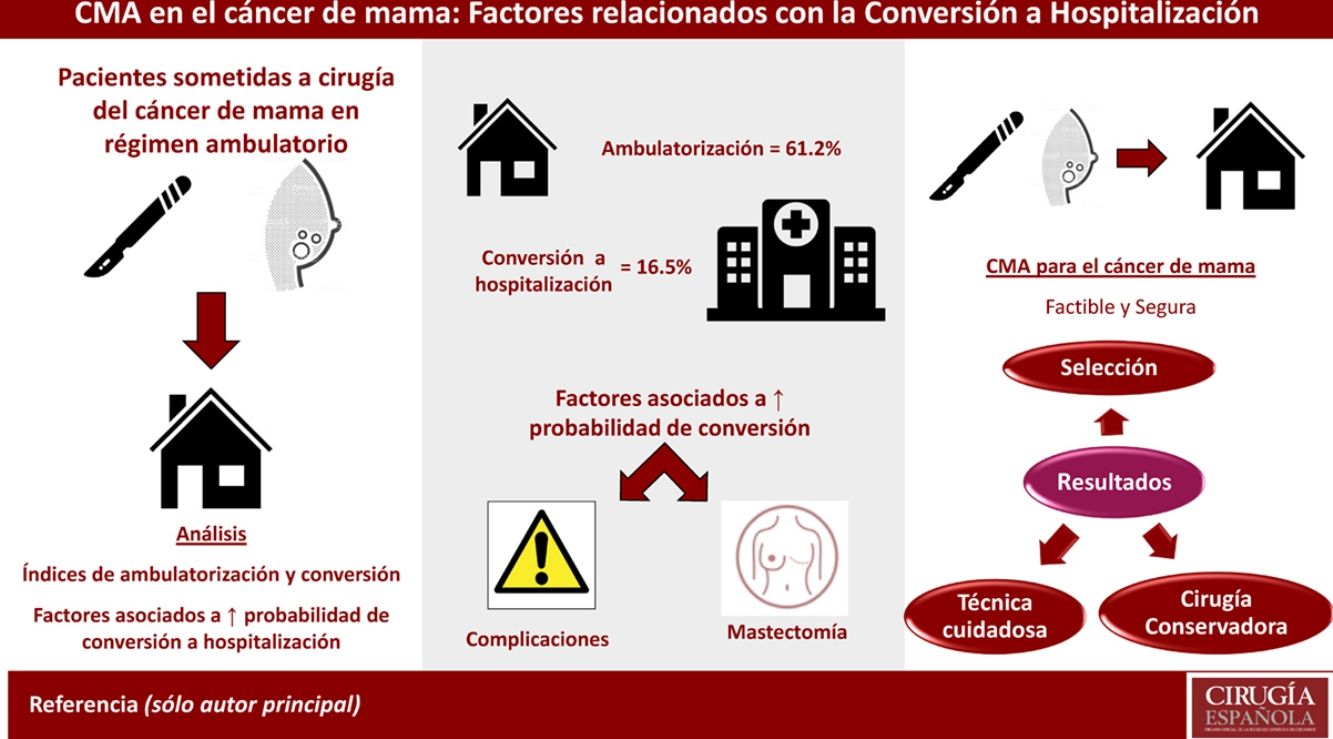
ResultsFor the global sample, the ambulatory surgery rate was 61.2%, 16.5% conversions and a success rate of 83.4%. For conservative surgery, ambulatory, success and conversion rates were 78.8%, 88.6 and 11.4%, respectively. For mastectomies, the ambulatory rate was 28.6%, with 62.9% success and 37.1% conversions. The 11 axillary surgeries were performed as day surgeries. Factors associated with conversion were mastectomy versus conservative surgery and the appearance of postoperative complications.
ConclusionsAmbulatory surgery for the surgical treatment of breast cancer should be standard care. Optimized results require adequate patient selection and the performance of surgical technique that needs to be as careful and as conservative as possible.
La realización de cirugía oncológica mamaria en régimen ambulatorio se está convirtiendo en una práctica estándar entre los centros públicos por los distintos beneficios que aporta. En este estudio se analizan los resultados obtenidos con esta modalidad asistencial y se identifican los factores relacionados con su fracaso.
MétodosSe analizaron retrospectivamente los datos de las 206 pacientes intervenidas por cáncer de mama en el año 2016 bajo 3 tipos de régimen: ambulatorio puro, ambulatorio-23h y hospitalario convencional. Se describen los índices de ambulatorización, éxito y conversión, tanto de forma global como distinguiendo entre cirugía conservadora, mastectomía±reconstrucción inmediata y cirugía axilar. Se realiza un análisis univariante para hallar aquellos factores relacionados con la conversión a régimen hospitalario.
ResultadosPara la muestra global se obtuvo un índice de ambulatorización del 61,2%, con un 16,5% de conversiones y un éxito del 83,4%. Para cirugía conservadora, ambulatorización, éxito y conversión fueron del 78,8, el 88,6 y el 11,4%, respectivamente. En las mastectomías la ambulatorización fue del 28,6%, con un 37,1% de conversión y un éxito del 62,9%. Las 11 cirugías axilares culminaron en régimen ambulatorio. Los factores asociados a una mayor probabilidad de conversión fueron la realización de mastectomía frente a cirugía conservadora y la aparición de complicaciones postoperatorias.
ConclusionesLa cirugía del cáncer de mama en régimen ambulatorio es factible y segura. Para la optimización de resultados resultan imprescindibles la cuidadosa selección de las candidatas y el desarrollo de una técnica quirúrgica cuidadosa y lo más conservadora posible.
Major ambulatory surgery (MAS) is defined as a surgical program in which moderately complex surgical procedures are performed and the patient leaves the hospital on the same day as the procedure.
Breast cancer is a pathology with a high incidence in our setting, and surgery is one of the pillars of its treatment with curative intent. Until recently, surgical procedures for the treatment of breast cancer (mastectomies, lymphadenectomies, etc.) were aggressive treatments. However, the implementation of breast-conserving surgery (lumpectomy) and multidisciplinary care programs has led to the development of outpatient breast cancer surgery. Some studies1,2 have shown that MAS for the treatment of breast cancer provides multiple advantages (greater patient satisfaction and psychological benefits, lower healthcare costs, etc.) without compromising surgical outcomes in terms of morbidity or readmissions. However, there are still cases in which patients selected for MAS are ultimately hospitalized for various reasons. In order to reduce this rate, factors leading to conversion should be identified in order to develop strategies to minimize their impact.
The objective of this study was to analyze the results obtained with an ambulatory surgical program for breast cancer surgery in a Breast Cancer Oncology Unit, as well as to identify the factors that led to possible failures.
MethodsAn observational and retrospective study was conducted including all the surgeries performed for breast cancer with a histological diagnosis of carcinoma (infiltrating or in situ) at the Breast Cancer Unit of a tertiary hospital in 2016.
From this global sample, we studied the patients selected for outpatient surgery. For the selection of candidates for this treatment regimen, the standard criteria of the hospital's MAS unit were applied, and the patients were assessed individually by a multidisciplinary team, including a surgeon, anesthesiologist and nurse:
- –
Absence of medical comorbidity (ASA I–III) or severe psychiatric comorbidity
- –
Adequate socio-family support
- –
Adequate understanding of the characteristics of the surgery and postoperative care
- –
Home less than one hour from the hospital
- –
Lumpectomy
In this manner, 3 patient groups were created:
- –
Patients selected for day surgery (DS): met all the above criteria; left the hospital on the same day of the surgery.
- –
Patients selected for the 23h ambulatory treatment (23h AT): did not meet one criterion, but were considered apt for ambulatory treatment; spent the night in the hospital and discharged the following day less than 24h after surgery. The patients who underwent mastectomy or lumpectomy with intraoperative radiotherapy (IORT) are usually in this group, unless another criterion was not met.
- –
Patients treated in the conventional regimen: did not meet 2 or more criteria.
The previously described criteria are applied with a certain flexibility. Thus, after discussion of the case by the multidisciplinary team in charge of selection, a patient may be selected for DS or 23h AT despite not strictly meeting a criterion in an exceptional and individual manner.
Data for the following variables were collected: age; ASA classification; comorbidities (Charlson comorbidity index); type of breast surgery performed, either breast-conserving surgery (lumpectomy±selective sentinel lymph node biopsy [SLNB]/axillary lymphadenectomy±‘oncoplastic technique’ IORT), mastectomies (simple, modified radical or with immediate reconstruction) or exclusively axillary surgeries (SLNB pre-chemotherapy/lymphadenectomy); and complications. We also analyzed the regimen in which the surgery was performed, the conversion to surgery with conventional hospitalization and the reason for conversion.
Statistical AnalysisThe data were analyzed with the SPSS statistical package for Windows v.20. (Chicago, IL, USA).
First, a descriptive study of the sample was carried out comparing the baseline characteristics (age, surgical risk and comorbidities), as well as the type of surgery performed among the patients selected for ambulatory treatment or hospitalization.
Afterwards, rates were calculated for ambulatory treatment, its success (number of procedures completed as MAS/number of MAS surgeries planned) and conversion to hospitalization for both the global sample and for the different types of surgery done (lumpectomy±IORT, mastectomy and axillary surgery). Next, a univariate analysis was performed to detect the factors associated with a higher rate of conversion to conventional hospitalization.
The categorical variables were expressed as frequency and percentage. The numerical variables as mean±standard deviation. In order to analyze the relationship between the qualitative variables, the χ2 test or Fisher's exact test was used. For the relationships between quantitative variables, the Student's t test or the Mann–Whitney U test was used, depending on whether the parameters studied followed a normal distribution or not. A P level <.05 was considered statistically significant. The odds ratio was used to measure risk, with a corresponding 95% confidence interval.
The project for this study was subjected to a strict evaluation process by the ethics committee at our hospital. The included patients signed informed consent for the inclusion of their data in the registry for further statistical analysis.
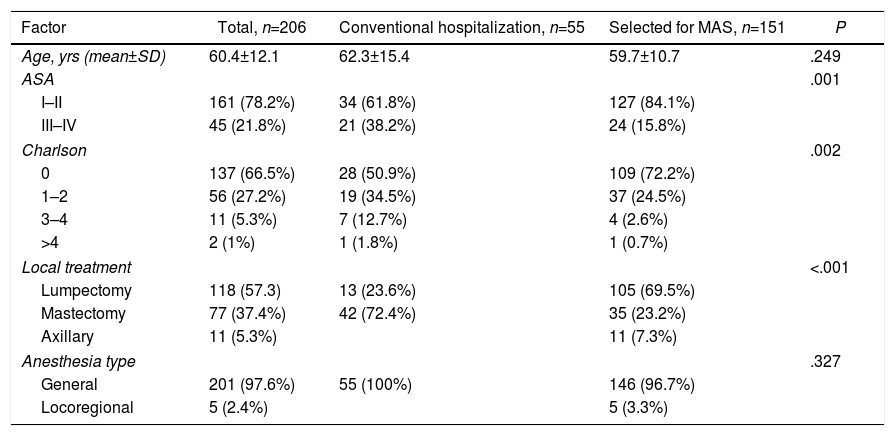
ResultsDuring the study period, a total of 206 breast cancer surgeries were performed; all patients were women, with an average age of 60.4±12.1. Table 1 shows the baseline characteristics (age, surgical risk, comorbidities) of the patients who underwent surgery and the type of surgery performed, both for the global sample and for the patients selected to undergo hospital or outpatient treatment (DS+23h AT). The patients selected for the ambulatory program had a statistically significant lower surgical risk and fewer comorbidities; they were also treated with lumpectomy at a significantly higher rate.
Baseline Characteristics of the Population Included in the Study and Type of Surgery Performed; Differences Between the Patients Selected for Surgery With Conventional Hospitalization or Ambulatory Care.
| Factor | Total, n=206 | Conventional hospitalization, n=55 | Selected for MAS, n=151 | P |
|---|---|---|---|---|
| Age, yrs (mean±SD) | 60.4±12.1 | 62.3±15.4 | 59.7±10.7 | .249 |
| ASA | .001 | |||
| I–II | 161 (78.2%) | 34 (61.8%) | 127 (84.1%) | |
| III–IV | 45 (21.8%) | 21 (38.2%) | 24 (15.8%) | |
| Charlson | .002 | |||
| 0 | 137 (66.5%) | 28 (50.9%) | 109 (72.2%) | |
| 1–2 | 56 (27.2%) | 19 (34.5%) | 37 (24.5%) | |
| 3–4 | 11 (5.3%) | 7 (12.7%) | 4 (2.6%) | |
| >4 | 2 (1%) | 1 (1.8%) | 1 (0.7%) | |
| Local treatment | <.001 | |||
| Lumpectomy | 118 (57.3) | 13 (23.6%) | 105 (69.5%) | |
| Mastectomy | 77 (37.4%) | 42 (72.4%) | 35 (23.2%) | |
| Axillary | 11 (5.3%) | 11 (7.3%) | ||
| Anesthesia type | .327 | |||
| General | 201 (97.6%) | 55 (100%) | 146 (96.7%) | |
| Locoregional | 5 (2.4%) | 5 (3.3%) | ||
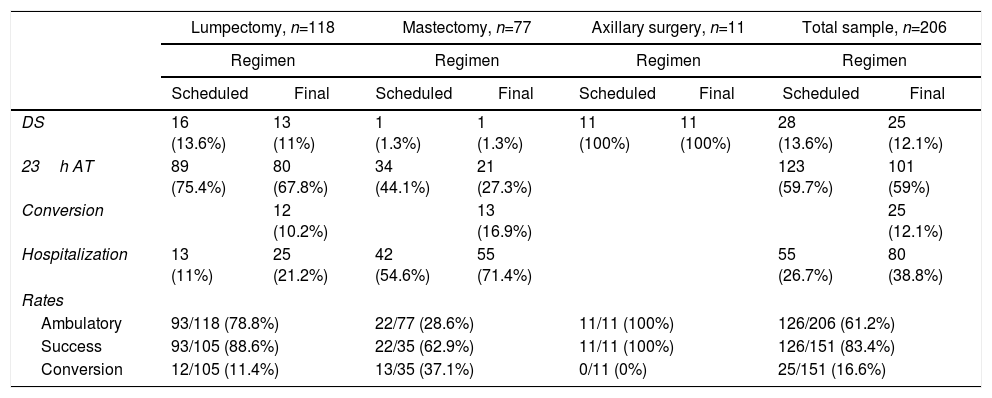
Out of the total of 151 (73.3%) interventions initially selected to be performed under the MAS regimen, 28 patients (13.6%) were programmed for DS and 123 patients (59.7%) for 23h AT. Among those cases selected for MAS, there were a total of 25 conversions to hospitalization (conversion rate=16.6%). In the end, 126 out of 206 procedures were ambulatory (ambulatory rate=61.2%), with a success rate of 83.5% (126/151).
The results obtained for the global sample and for each type of surgery, as well as the different calculated rates, are shown in Table 2.
Treatment According to the Different Types of Procedures Done, Including Ambulatory, Success and Conversion Rates for Each.
| Lumpectomy, n=118 | Mastectomy, n=77 | Axillary surgery, n=11 | Total sample, n=206 | |||||
|---|---|---|---|---|---|---|---|---|
| Regimen | Regimen | Regimen | Regimen | |||||
| Scheduled | Final | Scheduled | Final | Scheduled | Final | Scheduled | Final | |
| DS | 16 (13.6%) | 13 (11%) | 1 (1.3%) | 1 (1.3%) | 11 (100%) | 11 (100%) | 28 (13.6%) | 25 (12.1%) |
| 23h AT | 89 (75.4%) | 80 (67.8%) | 34 (44.1%) | 21 (27.3%) | 123 (59.7%) | 101 (59%) | ||
| Conversion | 12 (10.2%) | 13 (16.9%) | 25 (12.1%) | |||||
| Hospitalization | 13 (11%) | 25 (21.2%) | 42 (54.6%) | 55 (71.4%) | 55 (26.7%) | 80 (38.8%) | ||
| Rates | ||||||||
| Ambulatory | 93/118 (78.8%) | 22/77 (28.6%) | 11/11 (100%) | 126/206 (61.2%) | ||||
| Success | 93/105 (88.6%) | 22/35 (62.9%) | 11/11 (100%) | 126/151 (83.4%) | ||||
| Conversion | 12/105 (11.4%) | 13/35 (37.1%) | 0/11 (0%) | 25/151 (16.6%) | ||||
The most frequent reasons for conversion in the group of conservative surgery were postoperative nausea/vomiting and the development of hematoma in the immediate postoperative period. For mastectomies, the most frequent reasons for conversion were complications of the surgical wound and postoperative pain.
In the lumpectomy group, IORT was done in 40 patients (33.9%). Twenty-eight (70%) of these breast-conserving interventions with IORT were performed as 23h AT and one (2.5%) as DS. Seven of the 36 cases initially planned for conservative surgery with IORT in MAS had to be converted (success rate: 29/36=80.6%; conversion rate: 7/36=19.4%).
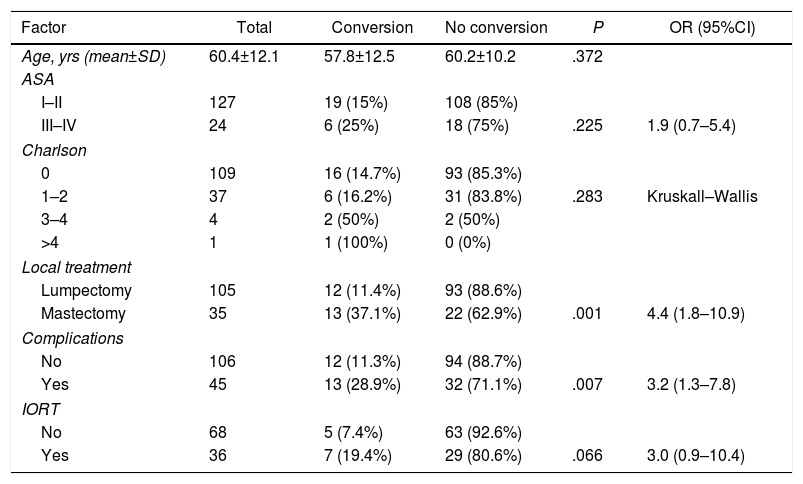
Table 3 shows the results of the univariate analysis in terms of conversion to hospitalization. The factors associated with a higher probability of conversion were mastectomy versus lumpectomy and the development of complications in the immediate postoperative period. In contrast, age, surgical risk estimated by the ASA classification, degree of comorbidity or the performance of IORT in patients with conservative surgery did not present an association with a higher probability of conversion.
Univariate Analysis of Factors Associated With a Greater Likelihood of Conversion.
| Factor | Total | Conversion | No conversion | P | OR (95%CI) |
|---|---|---|---|---|---|
| Age, yrs (mean±SD) | 60.4±12.1 | 57.8±12.5 | 60.2±10.2 | .372 | |
| ASA | |||||
| I–II | 127 | 19 (15%) | 108 (85%) | ||
| III–IV | 24 | 6 (25%) | 18 (75%) | .225 | 1.9 (0.7–5.4) |
| Charlson | |||||
| 0 | 109 | 16 (14.7%) | 93 (85.3%) | ||
| 1–2 | 37 | 6 (16.2%) | 31 (83.8%) | .283 | Kruskall–Wallis |
| 3–4 | 4 | 2 (50%) | 2 (50%) | ||
| >4 | 1 | 1 (100%) | 0 (0%) | ||
| Local treatment | |||||
| Lumpectomy | 105 | 12 (11.4%) | 93 (88.6%) | ||
| Mastectomy | 35 | 13 (37.1%) | 22 (62.9%) | .001 | 4.4 (1.8–10.9) |
| Complications | |||||
| No | 106 | 12 (11.3%) | 94 (88.7%) | ||
| Yes | 45 | 13 (28.9%) | 32 (71.1%) | .007 | 3.2 (1.3–7.8) |
| IORT | |||||
| No | 68 | 5 (7.4%) | 63 (92.6%) | ||
| Yes | 36 | 7 (19.4%) | 29 (80.6%) | .066 | 3.0 (0.9–10.4) |
In addition to specific advantages for different procedures, MAS provides a great savings in healthcare resources and a faster return to daily activity. This makes it an ideal option for certain types of surgeries, even more so in these times when it is important to increase the efficiency of public healthcare systems.
Oncological breast surgery is a suitable candidate for this regimen, especially considering the evolution of the integral treatment of this disease in recent decades, requiring progressively less aggressive procedures in both the breast and axillary region. Initially, performing lymphadenectomies limited the applicability due to the need for good analgesic control, increased risk of hemorrhage and specialized control of axillary drainage.3 After the introduction of the sentinel lymph node in MAS, it was proven that lymphadenectomy could also be included and that the key was in the immediate postoperative monitoring by specialized nursing personnel.
Currently, surgical interventions with low morbidity are generally considered for MAS, whose complications, for the most part, do not require specific treatment. It is also applicable in techniques developed more recently, such as oncoplastic surgery, which also have low morbidity rates.4 The development of more efficient anesthetic drugs and techniques for pain control and postoperative nausea/vomiting allow these patients to adequately control their symptoms at home. These factors have contributed to the increase in outpatient rates for these procedures to the point of becoming a standard care option.5
Ambulatory breast surgery does not compromise patient safety. Several studies have reported incidences of complications and readmissions similar or even lower than those of conventional surgery. The benefits are not economic alone. Ambulatory procedures have been associated with psychosocial advantages (high satisfaction rates and significantly higher scores on quality-of-life questionnaires),1,6–8 although the study by Margolese and Lasry1 found that 40% of patients would prefer to spend a night in the hospital.
Based on the results presented in this and other similar studies, the 23h AT stands out as a suitable alternative for the ambulatory treatment of more aggressive surgical procedures with longer surgical and anesthesia times, such as mastectomies with or without associated reconstruction or procedures with IORT. This regimen has wider acceptance and a feeling of safety among patients and medical professionals themselves.9
In our series, we achieved ambulatory rates that can be considered acceptable if we compare them with other studies of similar design in a comparable setting. Thus, our ambulatory percentage for the different procedures surpass those reported by Sánchez-García et al.,9 where a global ambulatory management rate of 47.7% was reached (69.4% for lumpectomy with SLNB, 8.1% in lumpectomy with axillary lymphadenectomy, and rates below 10% for mastectomies). Even so, our figures are far from the results obtained by other studies that achieved success rates of up to 70%, with significantly lower conversion figures (6%).10 However, the geographic characteristics of the island of Gran Canaria (patients with residences far from the hospital; a large percentage of rural population) must be taken into account, as well as the treatment of patients coming from Lanzarote Island, which are limiting factors for achieving higher rates of ambulatory treatment.
Most authors agree that, in order to achieve the greatest possible success in outpatient surgery programs for breast cancer, a multidisciplinary approach is necessary with the participation of several specialists: surgeons, anesthesiologists, nurses specialized in breast care, psycho-oncologists, etc. In order to increase ambulatory success and minimize conversion, it is first necessary to properly select patients based on their autonomy, ability to comprehend the procedure, family support and psycho-social circumstances, as well as their surgical risk; equally important is a thorough explanation about the care necessary during the postoperative period.3,11 For our group, another priority is having a nursing staff specialized in the care of patients who undergoing breast and axillary surgery. Their work is essential, both before surgery to instruct patients as well as in the postoperative management of the surgical wound, drain tubes and minor postoperative complications, such as seromas and hematomas.
What makes this study interesting is the inclusion of patients with breast-conserving surgery in addition to IORT in an outpatient surgery program. IORT is an alternative to external radiotherapy for selected patients that has been proven to be safe from an oncological standpoint and well tolerated by patients both in international clinical trials12 and in local studies conducted in our setting.13 It is a technique that does not significantly increase the morbidity of the procedure.14,15 This therapy enables us to complete the surgical treatment and local adjuvant treatment in the same day, thereby avoiding external radiotherapy in a large percentage of patients, with the resulting positive impact on their quality of life. Therefore, lumpectomy with IORT conducted in an ambulatory program, as carried out in 70% of our series among the candidates for this treatment, provides a synergistic benefit from the psychological point of view and in terms of quality of life. Furthermore, this therapeutic strategy combines the advantages of IORT with those of outpatient surgery in order to save costs.
As shown by the analysis of the factors correlating with the conversion to hospitalization in this study, the development of a surgical technique that is as conservative as possible and carefully minimizes tissue damage while thoroughly controlling hemostasis plays a crucial role in the prevention of the development of complications that, as we have seen, increase the likelihood of conversion. In cases with these complications, the previous instruction of the patients and ambulatory follow-up by specialized nursing staff can avoid hospitalization. Regarding age, as shown by the review by Bryson et al.,16 there is no clear association with higher conversion rates to hospitalization, although some studies show a higher incidence of adverse events (especially hemodynamic) in senior patients.17 It is likely that the absence of an association between the degree of comorbidity (estimated by the Charlson Comorbidity Index) or the surgical risk (ASA) and the conversion rates is due to an adequate preoperative selection of patients for outpatient surgery, as shown by the differences regarding these variables among the patients selected for hospital or outpatient care.
The limitations of this study would be the retrospective nature of the data collection, although a large part was included prospectively. In addition, it is a single-center study, which limits its validity. Also, certain psychosocial factors have not been included among the study variables, such as psychiatric comorbidities, the absence of family support, etc., which may determine a lower rate of ambulatory treatment or lead to a greater number of conversions.
Breast cancer surgery in a MAS regimen is feasible, safe and efficient, especially for conservative surgery, although 23h AT is an ideal alternative for more aggressive interventions. To optimize the results, it is essential to carefully select the potential candidates for the different MAS regimens, as well as the development of a meticulous surgical technique that is as conservative as possible while respecting the oncological safety criteria.
Conflict of InterestsThe authors who contributed to this manuscript have no conflict of interests.
Please cite this article as: Medina Velázquez R, Jiménez Díaz L, Fernández Carrión J, Rosas Bermúdez C, Miralles Curto M, Acosta Mérida MA, et al. Cirugía mayor ambulatoria del cáncer de mama: factores relacionados con la conversión a hospitalización convencional. Cir Esp. 2019;97:40–45.