Meckel's diverticulum is a congenital anomaly due to the incomplete closure of the omphalomesenteric duct during foetal development. Its incidence is estimated at around 2% of the population, and it is asymptomatic in most cases. Occasionally, it may cause symptoms of diverticulitis, lower gastrointestinal bleeding, occlusion or perforation. Symptoms are more frequent during childhood and rare in adults. Meckel's diverticulitis can have symptoms similar to acute appendicitis; generally, the diagnosis is an incidental intraoperative finding and treatment is diverticulectomy.
We present the case of a 26-year-old male patient with no personal or family history of interest who underwent emergency surgery due to suspected acute appendicitis using a laparoscopic approach. During surgery, the vermiform appendix showed no alterations and a Meckel's diverticulum was found with signs of inflammation that was 40cm from the ileocecal valve. We performed diverticulectomy and appendectomy, and the patient was discharged 4 days after surgery.
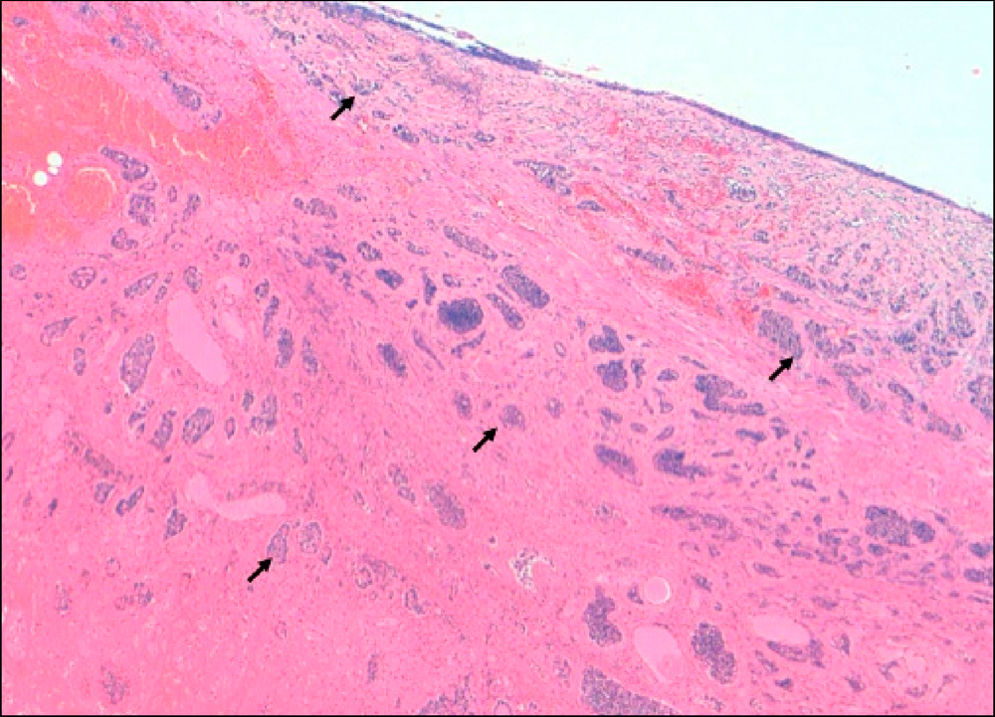
The histological study showed evidence of a 0.5cm neuroendocrine tumor (NET) in the lumen of the diverticulum that was well differentiated with 1% Ki-67 expression, positivity for chromogranin A and synaptophysin, invasion of all the layers of the intestinal walls to the serosa and free margins (Fig. 1). The thoracoabdominal study with computed tomography (CT) and OctreoScan® showed no evidence of residual lymph node disease or distant metastasis.
Given the degree of wall invasion of the neoplasm, radical oncological elective surgery was scheduled, and ileal-mesentery resection was performed at the site of the previous diverticulectomy. The pathology study showed no evidence of residual disease.
The presence of a NET in a Meckel's diverticulum is a very uncommon finding. In a bibliographic review from the Mayo Clinic of 1476 cases of Meckel's diverticulectomy, there was a reported incidence of 2.1%.1
NET of the gastrointestinal tract originate from neuroendocrine enterochromaffin cells located in the mucosa of the gastrointestinal tract. These form part of the Amine Precursor Uptake Decarboxylase (APUD) system, which is a hormone system parallel to the common endocrine system, whose hormone production does not come from glands but instead from epithelial cells.
Among gastrointestinal NET, small bowel tumors are the most frequent, followed by the rectum, cecal appendix, colon and stomach.2 NET can be functioning or non-functioning depending on whether they are accompanied by symptoms secondary to hormone secretion, such as carcinoid syndrome, which is mostly related with hepatic metastatic disease due to the inability to metabolise amines in the blood circulation. The indication for surgical resection of Meckel's diverticulum as an incidental finding is controversial.
There is consensus about prophylactic resection in paediatric patients, although this is not recommended in adults. Park et al. suggest that diverticulectomy can be beneficial in patients with one or more of the following conditions: male, younger than 50, length of the diverticulum greater than 2cm or suspicious/doubtful macroscopic appearance.1
Clinical management guidelines for NET do not make specific reference to the tumors located in a Meckel's diverticulum3 and, classically, they have been considered and treated like NET of the cecal appendix. Nonetheless, recent studies have reported that the behaviour and prognosis of NET in Meckel's diverticulum are similar to ileal tumors.4,5
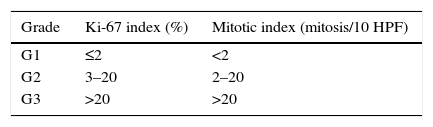
In the existing literature, there is a wide consensus that, if the NET found in a Meckel's diverticulum has a size greater or equal to 2cm, surgical rescue with radical intent is indicated, by extending the resection to the small bowel segment and mesentery corresponding with the previous diverticulectomy. The 2cm cut-point is based on experience with appendiceal tumors. Other authors consider it appropriate to indicate intestinal resections with lesions larger than or equal to 1cm, while tumors smaller than 1cm and no factors for a poor prognosis could benefit from diverticulectomy. In addition to size greater than or equal to 2cm, other risk factors for poor prognosis include affected resection margins, wall invasion surpassing the muscularis propria, vascular invasion and a classification equal to or greater than G2 according to the degree of Ki-67 expression and the mitotic index (Table 1).6
Jejunal-Ileal NET Grades According to the Percentage of Positivity for Ki-67 and Mitotic Rate, According to the ENETS/UICC.
| Grade | Ki-67 index (%) | Mitotic index (mitosis/10 HPF) |
|---|---|---|
| G1 | ≤2 | <2 |
| G2 | 3–20 | 2–20 |
| G3 | >20 | >20 |
ENETS: European Neuroendocrine Tumor Society; NNE: neoplasias neuroendocrine; UICC: Union for International Cancer Control.
Source: Pape et al.3
The prognosis, incidence of metastasis and incidence of carcinoid syndrome symptoms are similar to those associated with ileal NET7: 5-year survival is 100% in stages I/II, 97.1% in stage III and 84.8% in stage IV.8
In the case we have described, surgical rescue was considered due to the wall invasion that surpassed the muscularis propria as one of the previously stated factors for a poor prognosis.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Escarrà JM, Fraccalvieri D, Paules Villar MJ, Kreisler Moreno E. Tumor neuroendocrino en divertículo de Meckel: un hallazgo inusual. Cir Esp. 2015;93:e135–e136.