Malignant tumours occur in 0.1% of pregnant women. The most common types are cervical, breast, melanoma, lymphoma and leukaemia.1 Pancreatic cancer is unusual in women of child-bearing age.2 The average age for the diagnosis of pancreatic ductal adenocarcinoma is 72, and less than 3% of diagnosed patients are under the age of 45.3 We present a case of pancreatic adenocarcinoma during pregnancy.
The patient is a 35-year-old woman who had had 2 pregnancies, 1 normal delivery, and was at 16 weeks gestation. She presented with vomiting, pain in the left epigastrium and hypochondrium, general weakness and weight loss. Physical examination revealed a painful abdomen with positive Murphy sign and normal vitals. Lab results were: haemoglobin 8.6g/dL, total bilirubin 2.49mg/dL, direct bilirubin 1.4mg/dL, aspartate aminotransferase 120IU/L, alanine aminotransferase 125IU/L, phosphatase alcaline 313IU/L, serum amylase 136IU/L and urine amylase 426IU/L.
Abdominal ultrasound reported the absence of cholelithiasis or choledocholithiasis and multiple hypodense liver masses. Fine-needle biopsy demonstrated the presence of cells compatible with adenocarcinoma of the pancreas.
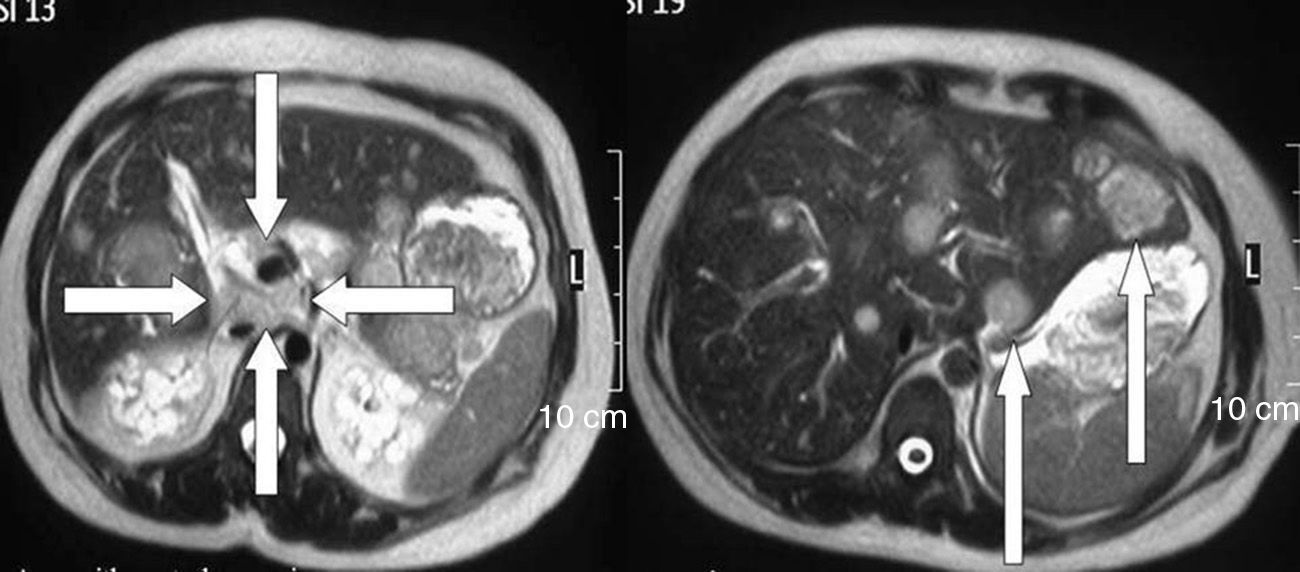
Tumour marker levels were: CA15-3, 36U/mL; carcinoembryonic antigen, 860ng/mL; CA19-9, 2750U/mL; and CA125, 2221U/mL. Endoscopic ultrasound demonstrated metastatic liver disease, several lymphadenopathies and a neoplastic mass in the tail of the pancreas measuring 40mm in diameter with central necrosis. Magnetic resonance confirmed the existence of an area of necrosis measuring 2cm×3cm in the pancreas, lesions in the liver and several lymphadenopathies in the hepatic-pancreatic hilum (Fig. 1).
Six days later, obstetric ultrasound confirmed the death of the foetus. Uterine evacuation obtained a foetus weighing 120g, followed by curettage.
The patient was discharged on the third day to later initiate outpatient chemotherapy, but she died 26 days later. The pathology study demonstrated the presence of a poorly differentiated adenocarcinoma of the pancreas. The tumour was larger than 6cm in diameter, with extension beyond the pancreas towards the lymph nodes and perineural invasion.
Although the exact cause is unknown, pancreatic cancer has several risk factors that have been identified (older age, male sex, diabetes, obesity, chronic pancreatitis and smoking).3 Certain genetic syndromes and germline mutations have been associated with cancer: familial atypical multiple mole melanoma, Peutz-Jeghers syndrome, hereditary pancreatitis, etc. However, these cases have been estimated to represent less than 20% of hereditary pancreatic cancer cases.2,3
In the present case, the pancreatic lesion was able to be identified by ultrasound since the uterus was not so large as to displace the organs or impede visualisation of the pancreas. Computed tomography and magnetic resonance are not limited by the size of the uterus or foetus and should be used for the diagnosis of pancreatic disease during pregnancy.4 Endoscopic retrograde cholangiopancreatography is used for the diagnosis and treatment of pancreatic tumours that cause obstructive jaundice, and it has been used during pregnancy. This technique should be considered for biliary drainage if surgery is not indicated or in pregnant women with jaundice.3
In pregnant patients with pain in the upper right abdomen and a large mass near the liver, CA19-9 concentrations should be measured. CA19-9 concentrations are useful in the diagnosis of pancreatic adenocarcinoma without jaundice in which a cut value of 100U/mL has provided a sensitivity of 55% and a specificity of 99%.5 CA19-9 levels are unaffected by pregnancy and can confirm the presence of malignant disease.4,6,7
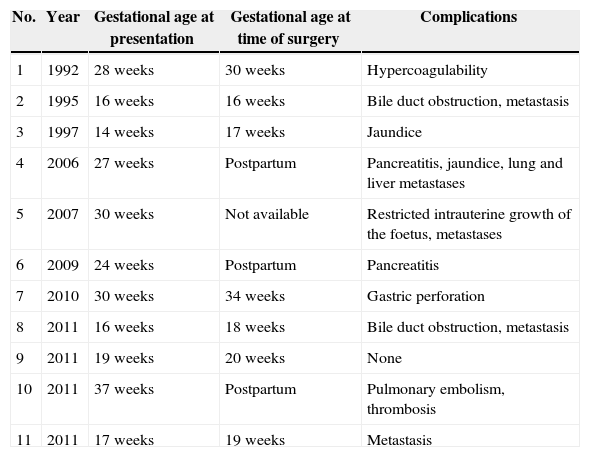
The prognosis of pancreatic adenocarcinoma during pregnancy, particularly in resectable cases, is unknown because most patients have advanced disease.7Table 1 summarises the published reports of pancreatic adenocarcinomas during pregnancy. Kazoka et al.2 reported a case of pancreatic adenocarcinoma during pregnancy and reviewed another 6 patients, 5 of whom died within the following 3 months due to advanced and unresectable disease. The patient of the case reported herein had an unresectable tumour and died within 3 months of the diagnosis.
Reports of Pancreatic Adenocarcinoma During Pregnancy.
| No. | Year | Gestational age at presentation | Gestational age at time of surgery | Complications |
|---|---|---|---|---|
| 1 | 1992 | 28 weeks | 30 weeks | Hypercoagulability |
| 2 | 1995 | 16 weeks | 16 weeks | Bile duct obstruction, metastasis |
| 3 | 1997 | 14 weeks | 17 weeks | Jaundice |
| 4 | 2006 | 27 weeks | Postpartum | Pancreatitis, jaundice, lung and liver metastases |
| 5 | 2007 | 30 weeks | Not available | Restricted intrauterine growth of the foetus, metastases |
| 6 | 2009 | 24 weeks | Postpartum | Pancreatitis |
| 7 | 2010 | 30 weeks | 34 weeks | Gastric perforation |
| 8 | 2011 | 16 weeks | 18 weeks | Bile duct obstruction, metastasis |
| 9 | 2011 | 19 weeks | 20 weeks | None |
| 10 | 2011 | 37 weeks | Postpartum | Pulmonary embolism, thrombosis |
| 11 | 2011 | 17 weeks | 19 weeks | Metastasis |
The 2 most important factors for determining the treatment strategy for pancreatic adenocarcinoma during pregnancy are disease stage and gestational age. In patients with a resectable mass in the first trimester of pregnancy, delayed surgery can lead to the lesion becoming unresectable, which would reduce survival.2 Pancreaticoduodenectomy can be performed during pregnancy since the risk of mortality associated with surgery is lower than 2%, even though the morbidity rates are high (close to 50%), while the 5-year survival rate after pancreatic cancer surgery is about 15%.3,6,7
Treatment with chemotherapy and radiotherapy is an additional therapeutic consideration for the management of pancreatic cancer as either adjuvant or neoadjuvant therapy, but there are obvious limitations during pregnancy.8,9 Most patients are not physically prepared to initiate treatment until 6 weeks after resection, during which time the disease has the chance to progress.2,7,8
Please cite this article as: Labarca-Acosta M, Reyna-Villasmil E, Aragón-Charris J, Santos-Bolívar J. Adenocarcinoma pancreático durante el embarazo. Cir Esp. 2015;93:475–477.