Perianal Paget's disease (PPD) is a very uncommon disease, included as a subgroup within extramammary Paget's disease (EMPD),1 the most frequent location of which is vulvar. PPD represents less than 1% of all anal diseases and 6.5%2 of all EMPD cases.3 There are few cases described in the literature; in fact, a multicenter EMPD study in Korea4 reported a total of only 7 cases of PPD in a 5-year period, and another study from New York5 reported 65 patients with PPD in 60 years.
We present a clinical case treated recently at our hospital. The patient is a 59-year-old woman with a recent history of about 6 months of anal and vulvar pruritus. Anal examination revealed perianal dermatitis, as well as a raised and indurated plaque on the right side, occupying the 2 quadrants (Fig. 1), which presented whitish pseudo-lichenoid areas. Initially, the patient had been treated by the dermatology service, with little response to topical treatment with corticosteroids. She was then referred to the general surgery service.
Rectal examination and anoscopy were anodyne. Given the persistence of the lesion despite conservative treatment, a biopsy was taken, which provided the diagnosis of PPD. Colonoscopy and rectal MRI ruled out a synchronous rectal neoplasm, as no pathological findings were observed. The extension study by computed tomography was negative.
The patient was treated surgically, using local excision with wide margins and reconstruction with a unilateral V-Y advancement flap.
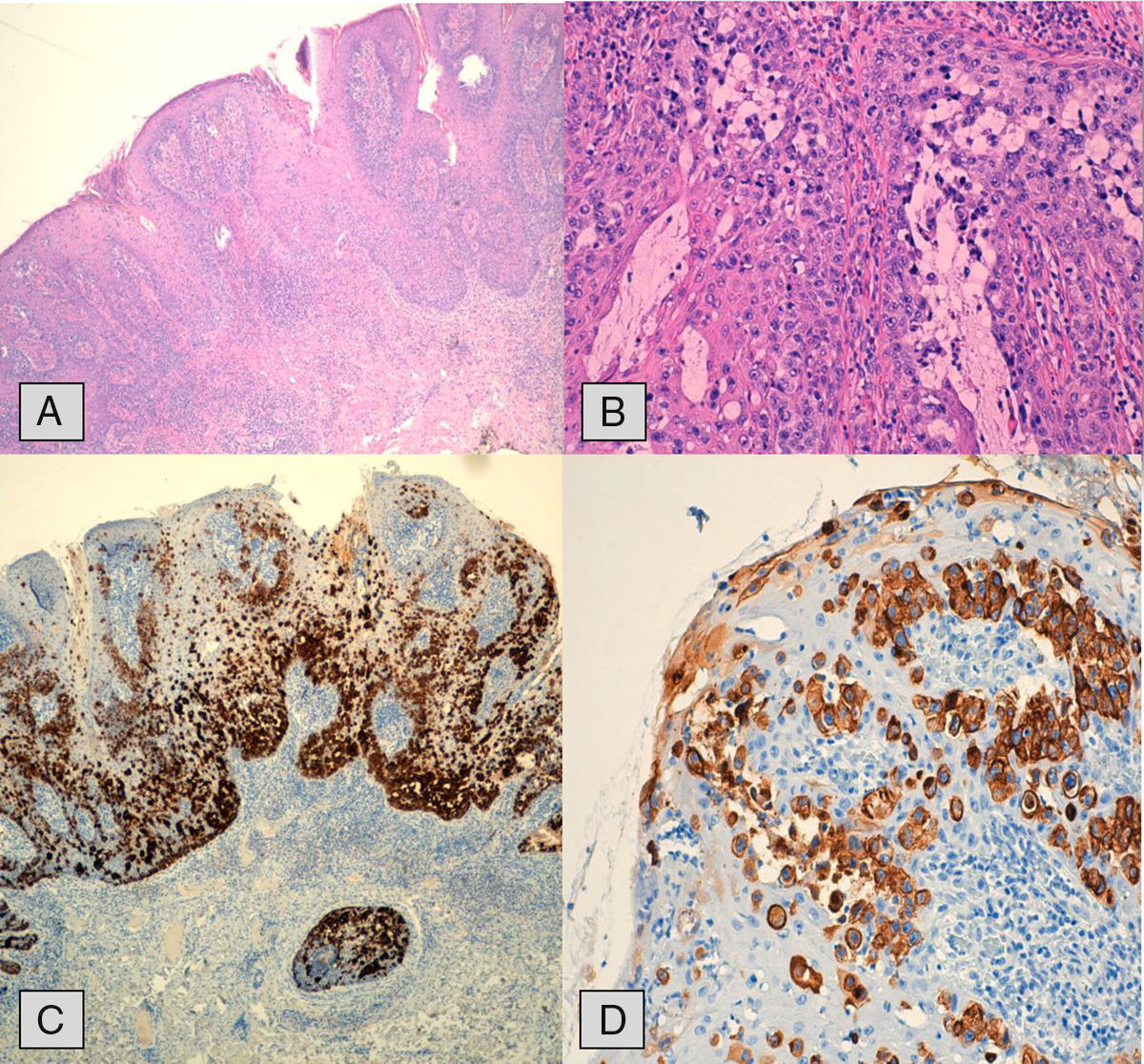
The pathology report confirmed PPD with complete resection, free margins and absence of malignization (Fig. 2A). In the histological study, the basal layer of the squamous epithelium was infiltrated by large cells with large nuclei and pale cytoplasm (Fig. 2B), suggesting the differential diagnosis with viral cytopathic changes. The positivity with immunohistochemistry for cytokeratin 7 confirmed that these were Paget cells (Fig. 2C and D).
(A) Extension study with hematoxylin–eosin stain showing infiltration and hyperplasia of the epidermal layer; (B) pagetoid cells are observed with ample cytoplasm and atypical nucleus with less prominent nucleoli; (C and D) immunohistochemistry study with cytokeratin 7 (CK7) demonstrating cytoplasmic positivity in the Paget cells, at basal layers and ascending.
The patient is currently asymptomatic after 8 months of follow-up, with no local recurrence.
Four diseases with different behaviors have been named after James Paget (1814–1899), British surgeon and pathologist: Paget's disease of bone, Paget's disease of the breast, Paget's abscess and EMPD.
EMPD is considered a premalignant lesion, a high grade intraepithelial dysplasia that can degenerate to adenocarcinoma, with dissemination capacity and high local recurrence rate. It affects the apocrine glands of the epidermis, located mainly in the perineum, vulva, scrotum, axilla, groin or thighs, and can spread to the dermis and cause lymphatic metastasis. Therefore, early identification and treatment is essential. EMPD can be associated with underlying adenocarcinoma and other internal neoplasms, being classified as primary or metastatic according to the involvement.1
Its clinical manifestation is usually nonspecific and in the form of erythematous plaque, perianal pain, pruritus, burning sensation, exfoliative/exudative warts and/or hypopigmentation, with a slow and insidious evolution that is usually confused with simple eczema. The differential diagnosis should include dermatitis/eczema, hemorrhoids, anal fissure, condylomata, Bowen's disease,6 melanoma and/or anal carcinoma. The definitive diagnosis is based on histology, which is typically positive for cytokeratins.
The initial approach to anal itching should always be conservative. PPD should be suspected for any erythematous, scaly, itchy lesion that shows no evident response after 6 weeks of topical treatment with corticosteroids. Biopsy should be taken for diagnosis.
PPD is a very rare perianal lesion, for whose diagnosis there should be a high index of suspicion. Given its metastatic potential, an excisional biopsy should be performed with wide margins, followed by a definitive anatomic pathology study to confirm clear margins. If infiltrating cancer is identified, treatment can include abdominoperineal resection, as in these cases local resection has been shown to be insufficient in terms of disease-free survival and long-term overall survival.7
We should also mention that this condition could also be an epidermotropic metastasis of a distant malignant neoplasm (urethra, rectum, sigmoid, bladder, prostate or endocervix),6 so the preoperative extension study using imaging tests is mandatory.
AuthorshipMireia Merichal Resina: article composition, data collection, and analysis and interpretation of the results.
Carlos Cerdan Santacruz and Enrique Sierra Grañón: data collection, analysis and interpretation of the results, critical review and approval of the final version.
Jordi Antoni Tarragona Foradada: analysis and interpretation of the results.
Jorge Juan Olsina Kissler: critical review and approval of the final version.
Please cite this article as: Merichal Resina M, Cerdan Santacruz C, Sierra Grañón E, Tarragona Foradada JA, Olsina Kissler JJ. Enfermedad de Paget perianal. Cir Esp. 2019;97:179–180.
This manuscript was presented at the 22nd National Meeting of the Spanish Association of Coloproctology, held in Bilbao on May 9–11, 2018.