Lumbar incisional hernias are rare abdominal wall defects, representing approximately 3.5% of all cases.1 There is no clear recommendation on what is the best surgical treatment strategy. In cases of incisional hernias of up to 8cm, some groups2 have proposed the laparoscopic approach as the technique of choice, with good results and low recurrence; in giant hernias, however, this does not seem feasible.
The Clinical Guidelines for Abdominal Wall Surgery by the Spanish Association of Surgeons proposes optimal treatments for lumbar hernias according to the characteristics of the abdominal wall defect (size, location, content, origin, any muscle atrophy, and presence or absence of previous recurrence). The classic anterior approach (open surgery) is quite traumatic, but it has the advantage of being able to carry out complete reconstruction of the abdominal wall. The laparoscopic approach has the advantages of any minimally invasive surgery, but does it not allow for controlled-tension hernioplasty or wall reconstruction. Thus, anterior herniorrhaphy is recommended for defects measuring less than 5cm with extraperitoneal contents. The laparoscopic transabdominal route is used in moderate defects measuring 5–15cm with intraperitoneal herniation. In cases of recurrence or in abdominal wall defects larger than 10–15cm, an anterior double-mesh hernioplasty is recommended. Finally, in cases of associated muscular atrophy or significant deformity, a repair under a certain amount of tension is necessary to guarantee an adequate aesthetic and functional result, an objective that cannot be achieved by laparoscopy, so a double preperitoneal prosthetic repair technique is recommended.3
We report the case of a patient with a giant lumbar incisional hernia. The defect could not be repaired with the most suitable technique (which would have been an anterior hernioplasty with double preperitoneal mesh) because there was not enough space to guarantee mesh fixation, so we opted for an intraperitoneal double-mesh repair (sandwich technique). The sandwich technique (repair using an intraperitoneal mesh associated with a supra-aponeurotic polypropylene mesh) presents a 3.9% recurrence rate within 20 months in midline laparotomy eventrations4 (in this study, a biological intraperitoneal mesh was used).
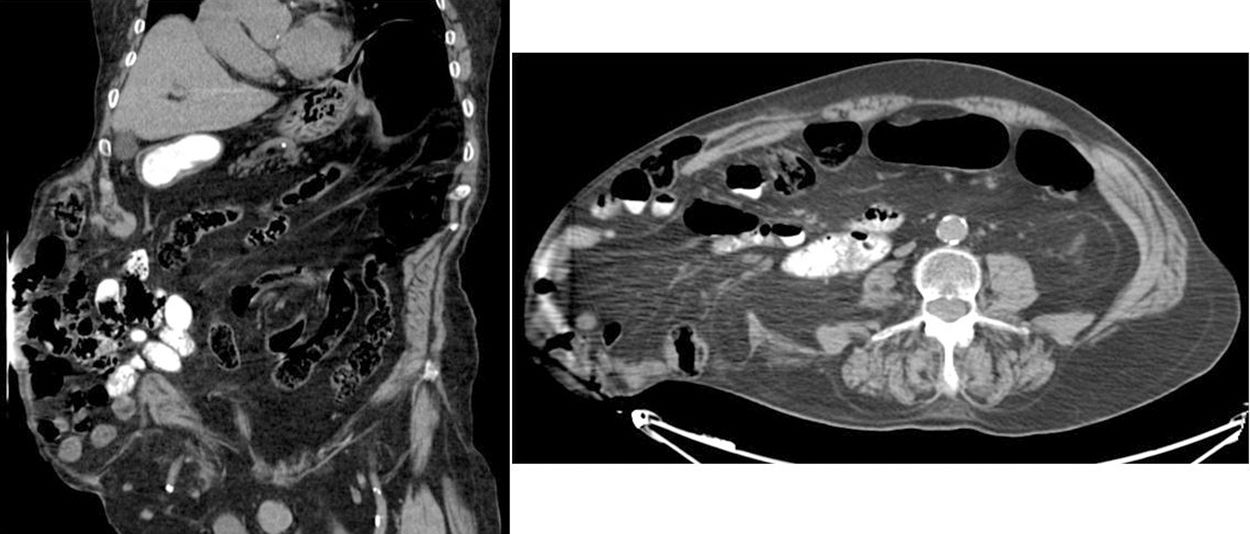
A 72-year-old male with multiple pathologies (ex-smoker, BMI 28.7, a history of arterial hypertension, atrial fibrillation, chronic bronchitis, chronic osteomyelitis, peripheral vasculopathy and ischaemic cerebrovascular accident with right brachiocrural hemiparesis as sequela), who presented a giant incisional hernia on the right flank that had been progressing for the past 2 years. Upon physical examination, an abdominal wall defect was palpated from 2cm below the last rib to the iliac crest and from the lateral edge of the rectus abdominis muscles to the lumbar area, which comprises an area of approximately 20×15cm; the defect was able to be reduced in left lateral decubitus (Fig. 1). Chevrel classification5: L1-2-3-4, W4 and R1.
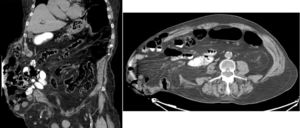
An abdominal CT scan showed the voluminous right lumbar incisional hernia containing the cecum, proximal part of the right colon and small intestine loops with no signs of complications (Fig. 2). The hernia content had an approximate volume of 6.2L, representing 16.7% of the entire abdomen (total abdominal volume approx. 37.2L). In other words, there was no loss of domain, which is defined as a hernia of more than 50% of the abdominal cavity contents.
Surgery was scheduled, and an open approach in the right flank was used to identify a large hernia sac containing the right colon and small bowel loops. The incisional hernia was repaired with placement of an intraperitoneal mesh of polypropylene and hyaluronic acid measuring 13.8×17.8cm, which was affixed to the muscle edges with PDS sutures while trying to avoid tears and tension, and another supra-aponeurotic polypropylene reinforcement mesh measuring 26×36cm that was affixed with Vicryl sutures. Two low-pressure suction drains were placed in the subcutaneous plane.
The patient progressed satisfactorily, with no evidence of persistence of hernia in the immediate postoperative period, so he was discharged 11 days after surgery. At the 3-month follow-up office visit, there was no evidence of recurrence on CT.
In the case of large incisional hernias, the use of prosthetic material is necessary to bridge the abdominal wall defect and thereby achieve tension-free closure.6 The sandwich technique enables surgeons to repair the abdominal wall with very good results, reducing the risk of developing intra-abdominal compartment syndrome and the risk of recurrence. Studies are needed to determine the long-term results and recurrence rate of this technique when used in giant lumbar hernias.
Please cite this article as: Lucas Guerrero V, Zerpa Martín C, González López JA, Rebasa P, Navarro Soto S. Reparación de eventración lumbar gigante mediante técnica sándwich. Cir Esp. 2019;97:177–178.