Bariatric surgery is the most effective and long-lasting therapeutic option for the treatment of morbid obesity and its comorbidities. In the last decade, sleeve gastrectomy has been established as the most widely used surgical procedure in bariatric surgery, showing exponential growth.1 Even so, gastric bypass is the technique of choice when sleeve gastrectomy is not an absolute contraindication but should be indicated with caution, especially in cases of previous gastroesophageal reflux.2
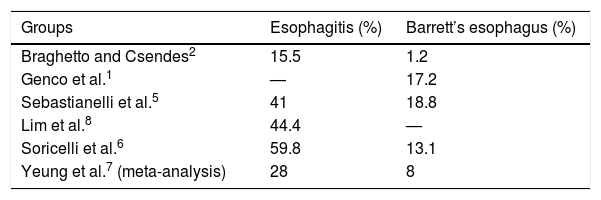
Compared to the population at large, people with morbid obesity have a higher incidence of gastroesophageal reflux, esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma.3 Although some studies describe a decrease in gastroesophageal reflux after sleeve gastrectomy,4 recent studies show the high risk of developing de novo reflux, esophagitis and Barrett’s esophagus in the medium to long term after this procedure,1,2,5–7 with the subsequent risk of malignancy. Table 1 shows the percentage of esophagitis and Barrett’s esophagus after sleeve gastrectomy observed in several studies. A recent meta-analysis has indicated that, after sleeve gastrectomy, 23% of patients have de novo gastroesophageal reflux, 28% esophagitis, and 8% develop Barrett’s esophagus7 (compared to 1.6% of the general population5). The increased incidence of reflux is probably due to an imbalance between intragastric pressure and the pressure of the lower esophageal sphincter. A directly proportional relationship has also been observed between the diameter of the tubular stomach and the incidence of reflux.8
Another notable feature is that the endoscopic findings do not correlate with the severity of the gastroesophageal reflux symptoms perceived by the patient.6 In fact, some authors suggest performing systematic follow-up endoscopies to screen for lesions associated with reflux, regardless of whether there are symptoms or not.1,5,6,8
Given that sleeve gastrectomy is widely used around the world, this is a topic of special interest in young patients, who have many years ahead to develop complications. It is unknown whether the progression to Barrett’s esophagus and adenocarcinoma occurs identically in patients who undergo sleeve gastrectomy compared to the rest of the population.8 The optimal approach to follow after the diagnosis of Barrett’s esophagus in a patient with sleeve gastrectomy is also unclear: follow-up, or conversion to gastric bypass?
Despite the above, the literature published on cases of esophageal adenocarcinomas in patients treated with sleeve gastrectomy is very limited. Khoury et al. described a patient who already had Barrett’s esophagus before sleeve gastrectomy.9 Wright et al. reported a case of a patient with a normal preoperative endoscopy study, who developed reflux after surgery and had developed esophageal adenocarcinoma 5 years later.10
We present the case of a 60-year-old patient with a history of hypertension, diabetes, dyslipidemia, acute myocardial infarction and stent placement in 2002, depression and morbid obesity, with a body mass index of 39, no symptoms of gastroesophageal reflux and previous fibrogastroscopy that was normal. In May 2011, the patient underwent sleeve gastrectomy.
Given the latest publications on esophagitis and Barrett’s esophagus after sleeve gastrectomy in asymptomatic patients, at our hospital we carried out a follow-up study of patients who had undergone sleeve gastrectomy (all of them with previous fibrogastroscopy) with more than 4 years of evolution. We analyzed both symptoms and endoscopic findings.
In the context of this study, our patient was studied by fibrogastroscopy in January 2019, which found evidence of a 9-mm lesion in the distal esophagus. Barrett’s esophagus was confirmed with high-grade epithelial dysplasia. An immunohistochemical study showed marked positivity with a component of high-grade dysplasia (CK CAM5.2), high proliferative index (Ki-67), and nuclear positivity for p53 in the high-grade component. In March 2019, endoscopic resection of the mucosa was performed; the pathological study showed Barrett’s esophagus with foci of high-grade dysplasia with free margins, and no infiltrative component. Fibrogastroscopy was repeated 2 months later and demonstrated areas of Barrett’s esophagus close to the resection area. Two cycles of radiofrequency ablation were performed. Two months later, a new endoscopic follow-up study was done and biopsies taken, but there were no pathological findings.
In October 2019, the patient underwent laparoscopic conversion of the sleeve gastrectomy to gastric bypass.
As shown in the case above, we feel it is important to monitor these patients in order to detect and treat Barrett’s esophagus and dysplasia in time, despite not being a frequent finding, before they degenerate into adenocarcinoma. This is especially important when considering that lack of symptoms does not completely rule out the disease.
To conclude, we suggest that routine endoscopies should be included in the follow-up testing of all patients who have undergone sleeve gastrectomy. More studies are needed to determine the magnitude of the problem and to adjust the indications for sleeve gastrectomy for the treatment of morbid obesity.
Please cite this article as: Lucas Guerrero V, Luna A, Rebasa P, Montmany S, Navarro S. Degeneración del esófago de Barrett tras gastrectomía vertical. Cir Esp. 2021;99:70–71.