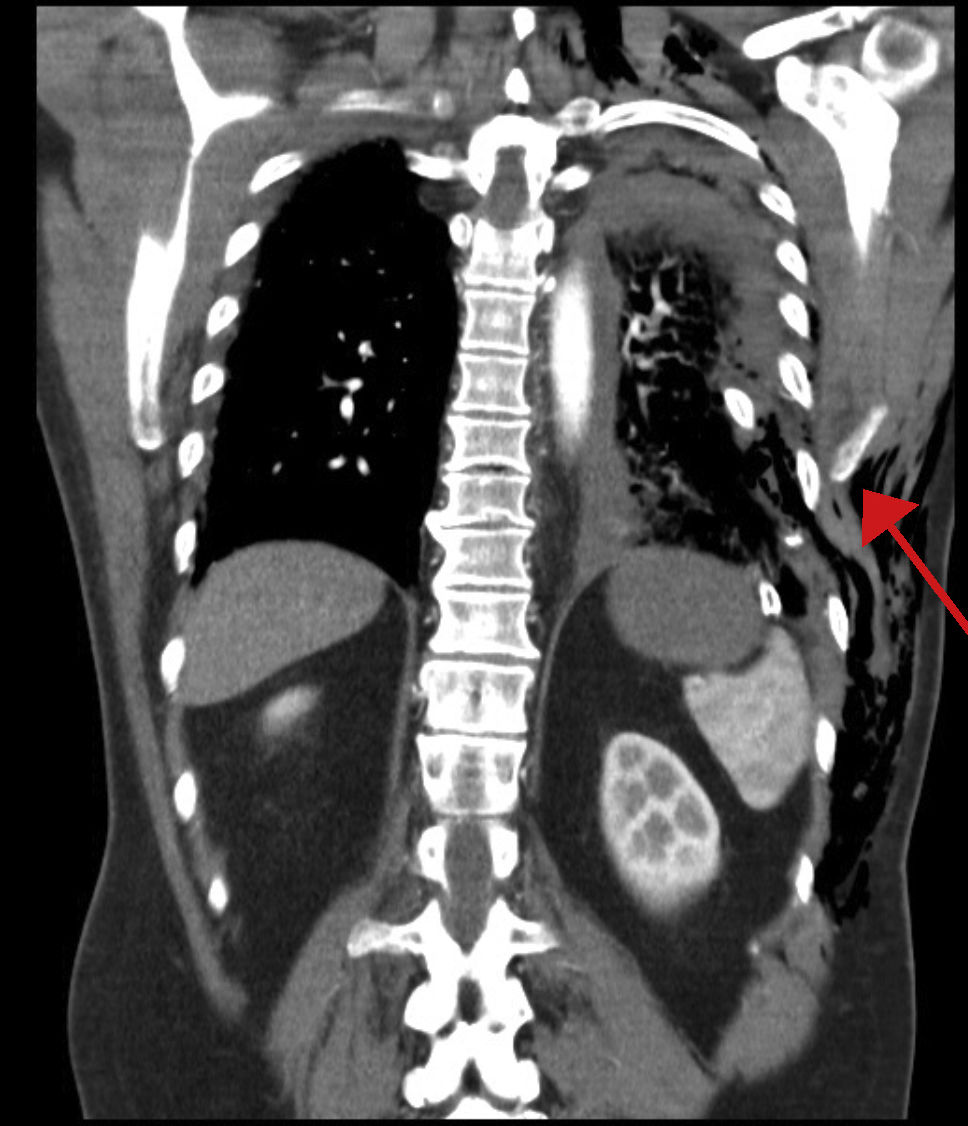
Our patient is a 60-year-old man with a history of severe chest trauma that had occurred one year prior, associated with multiple left rib fractures, pneumothorax and left subcutaneous emphysema (Fig. 1), which required drainage. One year later, the patient came to the emergency room for abdominal pain in the left flank and hypochondrium that had been developing for 2 days, associated with constipation and vomiting.
During examination, he presented pain on palpation in the left flank and hypochondrium, with no signs of peritoneal irritation but showing diminished peristalsis. Blood work reported no alterations. Chest X-ray revealed a distended gastric chamber at the thoracic level. Abdominal CT scan (Fig. 2) demonstrated a 28-mm defect in the left diaphragm with gastric herniation and associated gastric distention. Subsequently, a nasogastric tube was inserted, after which the gastric distention improved. We decided to operate and performed reduction of the hernia, closure of the diaphragmatic orifice, and mesh placement via laparoscopy.
DIAGNOSIS: Post-traumatic diaphragmatic hernia
Please cite this article as: Cambeiro Cabré L, Targarona Soler EM, Rodríguez-Otero Luppi C, Borràs Marcet J. Hernia diafragmática postraumática. Cir Esp. 2021;99:64.