The aim of the study was to evaluate preoperative factors associated with remission of diabetes and weight loss after laparoscopic gastric band surgery.
Materials and methodsA retrospective cohort of 95 patients who had an adjustable gastric band placed were included. A preliminary descriptive study of prognostic factors was performed using the logistic regression model with SPSS 17.0. The independent variables were age, sex, body mass index (BMI), diabetes status, and degree of obesity; dependent variables were the proportion of weight loss, change in diabetes status score, and percent changes in fasting sugar and glycosylated haemoglobin.
ResultsThe variables that were significantly associated with the percentage of changes in fasting blood sugar and glycated haemoglobin were: the degree of obesity in the first year; preoperative and diabetes status respectively. The analysis of the need for antidiabetic treatment using the modified diabetes status score showed preoperative BMI, age, and gender as significant predictors.
ConclusionsIn patients undergoing gastric band surgery, weight loss is the fundamental mechanism by which insulin sensitivity increases. This improvement in glucose metabolism is influenced by factors such as sex, age, insulin treatment, duration of diabetes, and degree of preoperative obesity.
El objetivo del estudio ha sido evaluar factores preoperatorios relacionados con remisión de la diabetes y pérdida de peso tras cirugía de banda gástrica ajustable por vía laparoscópica.
Meterial y métodosSe incluye una cohorte retrospectiva de 95 pacientes a los que se colocó banda gástrica ajustable. Se realizó un estudio preliminar descriptivo de factores pronósticos mediante el modelo de regresión logística con SPSS 17.0. Las variables independientes fueron edad, sexo, índice de masa corporal (IMC), estado de diabetes y grado de obesidad; las variables dependientes fueron proporción de peso perdido, variación del diabetes status score y porcentajes de variación en la glucemia basal y en la hemoglobina glucosilada.
ResultadosLas variables que presentaron relación estadísticamente significativa con los porcentajes de variación en la glucemia basal y en la hemoglobina glucosilada fueron: el grado de obesidad durante el primer año y el estado preoperatorio de diabetes respectivamente. El análisis de las necesidades de tratamiento antidiabético mediante el diabetes status score modificado señala al IMC preoperatorio, la edad y el sexo como factores predictores significativos.
ConclusionesEn pacientes intervenidos de cirugía con banda gástrica la pérdida de peso contribuye a mejorar la sensibilidad a insulina. Esta mejoría del metabolismo glucídico se ve influida por factores tales como el sexo, la edad, el tratamiento insulínico, el tiempo de evolución de la diabetes y el grado de obesidad preoperatorio.
Diabetes is one of the main diseases that affect health, quality of life, and survival in obese people.1 At present, it is considered a pandemic with 240 million affected people, a figure that is expected to increase to 380 million worldwide in the next 15 years.2 Although diabetes is a prevalent condition in morbidly obese patients, few studies analyse the prognostic factors of improvement in the metabolism of diabetic patients.
While in malabsorptive or mixed bariatric surgery it has been suggested that changes in gastrointestinal hormones are involved, the antidiabetic effect of gastric band surgery seems to be caused by weight loss. This weight loss reduces fat content, thus decreasing the inflammatory mediators and increasing insulin sensitivity.3
The prognostic factors and physiological mechanisms involved in the resolution of diabetes related to bariatric surgery are not as well known as those that determine weight loss. This occurs, in part, due to the different criteria used to define diabetes resolution.4 The American Diabetes Association (ADA) has recently defined complete remission as HbA1c<6%, fasting blood sugar<100mg/dL and absence of drug treatment for at least 1 year.5
The aim of this study is to identify preoperative factors that are useful to predict weight loss and optimisation of glucidic metabolism in obese patients treated with adjustable gastric band surgery.
Materials and MethodsWe present a retrospective descriptive study of patients who underwent bariatric surgery at Hospital Sierrallana from July 2009 to July 2013. All patients followed the same preoperative protocol and were assessed by a multidisciplinary team (endocrinologist, dietitian, bariatric surgeon, anaesthetist, psychiatrist, gastroenterologist, and cardiologist). A hypocaloric, hyperproteic diet was indicated before the surgery. An adjustable gastric band surgery was performed in all cases following the surgical indications of the National Institute of Health6 guidelines and using the Lap-Band system placed through the “pars flaccida” approach.
All patients were included in the same postoperative follow-up protocol. Fluid oral intake was started 12h after the procedure. Patients were discharged 24h after food intake was started, if no complications were observed. Patients were subject to follow-up by the endocrinologist, dietitian, and bariatric surgeon at 1 week, 1 month, 3 months, and every 6 months thereafter.
Demographic variables, obesity degree, and diabetes status were analysed. During follow-up after the procedure, proportion of weight loss, fasting blood sugar, HbA1c and diabetes status score were considered. Since in gastric band surgery the fundamental mechanism on diabetes is weight loss, this is studied as a response variable. For such purpose, we used the percentage of overweight loss (POL) with a cut-off value of 50%. Moreover, the criteria used by the ADA4 to define complete remission of diabetes (HbA1c, fasting blood sugar, and absence of drug treatment) were considered as response variables for a breakdown analysis of the influence of the predictive factors.
For the analysis of the antidiabetic treatment, the modified diabetes status score version by Demaria et al. was used.7,8 This 6-point scoring system assigns a numerical value from 0 to 5 to objectively quantify disease severity. Value 0 indicates that there are no diabetes symptoms; 1, changes in fasting blood sugar; 2, diabetes controlled with oral antidiabetics; 3, diabetes controlled with insulin; 4, diabetes controlled with insulin and oral antidiabetics; and 5, diabetes with severe complications.8 For the purpose of this study, >1 point decreases in the preoperative initial score were considered during the first 3 years of follow-up.
Results were analysed with the statistical software SPSS 17.0 (SPSS, Inc., Chicago, IL, USA) and logistic regression models were made for each one of the response variables. Data were expressed as mean±(standard deviation) or median (range). The Chi-square test and Fisher's exact test were used for categorical demographic data, and unpaired Student's t-test and ANOVA with Scheffé post hoc test for quantitative variables. Results were considered significant if P<.05.
ResultsPopulation CharacteristicsDuring the period between July 2009 and July 2013, a total of 95 patients with morbid obesity were included: 66 (69.5%) women and 29 (30.5%) men with a mean age of 47.71±12.2 years (range: 19–70) at the time of surgery. Mean body mass index (BMI) was 42.38±4.6kg/m2, and patients with morbid obesity 58 (63%) and type II obesity 29 (31%) predominate over other degrees of obesity. Median follow-up in our patients was 2 years and 3 months (range from 1 to 4 years). Mean fasting blood sugar in all the sample was 112.71±35.9mg/dL; mean glycated haemoglobin was 6.24±1.3% and mean diabetes status score was 1.03±0.8 (see Table 1). Out of them, 22 were diagnosed with DM2 before the surgical procedure (12 of them with at least 5 years of progress since diagnosis). In this group, mean fasting blood sugar was 133.34±9.3mg/dL; glycated haemoglobin 6.89±0.3% and diabetes status score was 2.21±0.2 (13 patients took oral antidiabetics; 4, insulin; and 2 patients took both; the rest of the subjects did not follow a specific treatment for diabetes).
Preoperative Demographic Characteristics in the Group of Diabetic Patients Compared to the Total Sample.
| Variable | Diabetic patientsNo.=22 | TotalNo.=95 | P |
|---|---|---|---|
| Age (years) | 53.1±2.1 | 47.7±12.2 | .79 |
| Sex n (%) | |||
| Female (n) | 15 (68) | 66 (69.5) | .83 |
| Male | 7 (32) | 29 (30.5) | |
| Weight (kg) | 111.25±2.34 | 114.76±15.9 | .81 |
| BMI (kg/m2) | 41.6±1.11 | 42.38±4.6 | .72 |
| HbA1c (%) | 6.89±0.33 | 6.24±1.3 | .06 |
| Fasting blood sugar (g/dL) | 133±9.31 | 112.71±35.9 | .04 |
| Diabetes status score | 2.21±0.2 | 1.03±0.8 | .02 |
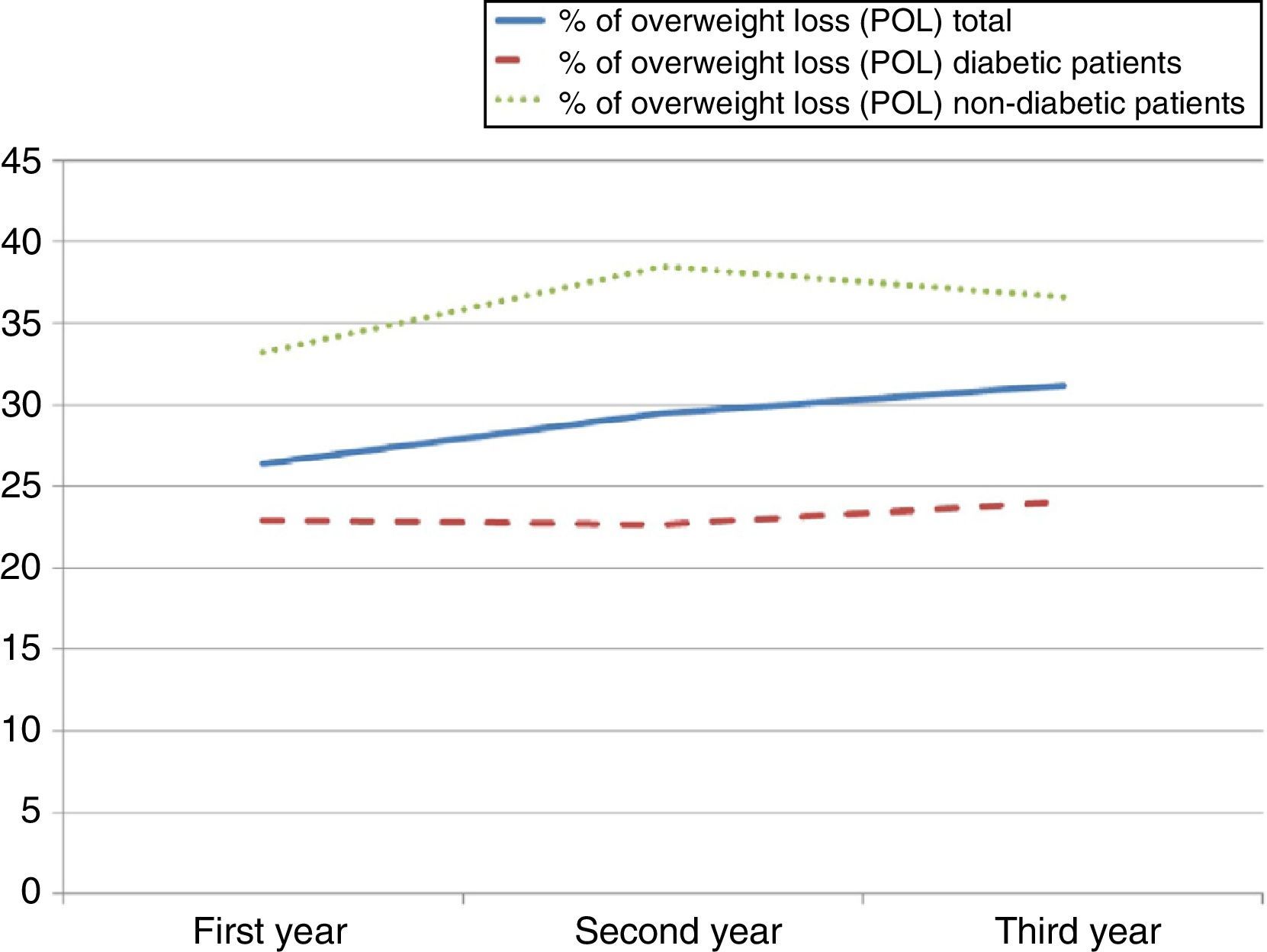
Mean POL in the first year was 26.40±4.8%, in the second year 29.50±5.9% and in the third year 31.14±5.5% (see Fig. 1). From the studied factors, only preoperative diabetes status shows a statistically significant relationship with POL during the first year after surgery (P=.042; odds ratio [OR]=0.77; 95% confidence interval [CI]: 0.68–0.88). During the second and third years, proportion of POL continues being greater in non-diabetic patients, but it does not reach a statistically significant result (see Table 2).
Factors Associated With the Percentage of Overweight Loss.
| Variable % (n) | First year | P | Second year | P | Third year | P | |||
|---|---|---|---|---|---|---|---|---|---|
| total | 82.8 (77) | 17.2 (16) | 72 (31) | 28 (12) | 76.5 (13) | 23.5 (4) | |||
| <50% POL | ≥50% POL | <50% POL | ≥50% POL | <50% POL | ≥50% POL | ||||
| Sex | |||||||||
| Female | 82.8 (53) | 17.2 (11) | .99 | 66.7 (22) | 33.3 (11) | .15 | 75 (9) | 25 (3) | .82 |
| Male | 82.8 (24) | 17.2 (5) | 90 (9) | 10 (1) | 80 (4) | 20 (1) | |||
| DM | .01 | .52 | .85 | ||||||
| Diabetic patients | 100 (22) | 0 (0) | 80 (8) | 20 (2) | 80 (4) | 20 (1) | |||
| Non-diabetic patients | 77.5 (55) | 22.5 (16) | 69.7 (23) | 30.3 (10) | 75 (9) | 25 (3) | |||
| Age | .31 | .95 | .45 | ||||||
| <45 years | 77.8 (28) | 22.2 (8) | 71.4 (10) | 28.6 (4) | 85.7 (6) | 14.3 (1) | |||
| ≥45 years | 86.0 (49) | 14 (8) | 72.4 (21) | 27.6 (8) | 70 (7) | 30 (3) | |||
| BMI | .24 | .44 | .68 | ||||||
| ≤40kg/m2 | 77.5 (31) | 22.5 (9) | 66.7 (14) | 33.3 (7) | 71.4 (5) | 28.6 (2) | |||
| >40kg/m2 | 86.8 (46) | 13.2 (7) | 77.3 (17) | 22.7 (5) | 80 (8) | 20 (2) | |||
| Obesity | .69 | .99 | .68 | ||||||
| Obesity I | 75 (3) | 25 (1) | – | – | – | – | |||
| Obesity II | 86.2 (25) | 13.8 (4) | 72.2 (13) | 27.8 (5) | 71.4 (5) | 28.6 (4) | |||
| Morbid obesity | 80.4 (45) | 19.6 (11) | 72 (18) | 28 (7) | 80 (8) | 20 (2) | |||
| Supermorbid obesity | 100 (4) | 0 (0) | – | – | – | – | |||
Bivariate analysis with Chi-square test (or Fisher's exact test). Proportion of overweight loss (POL) has been categorised with the cut-off value of 50%.
DM, diabetes mellitus; BMI, body mass index; O, obesity; Obesity I, BMI 30–34.9; Obesity II, BMI 35–39.9; morbid obesity, BMI 40–49.9; supermorbid obesity, BMI>50; POL, percentage of overweight loss.
The percentage of decrease in postoperative fasting blood sugar was 13.6±11, 12.2±9 and 14.6±9.6% in the first, second, and third years, respectively. As shown in Table 3, it is influenced by the degree of obesity in the first year of follow-up (P=.01). However, this statistical association of the bivariate analysis is not confirmed by the logistic regression model (P=.31; OR=1.27).
Prognostic Values of Changes in Fasting Blood Sugar.
| Variable % | First year | P | Second year | P | Third year | P |
|---|---|---|---|---|---|---|
| Total | 13.6±10.8 | 12.2±8.7 | 14.6±9.6 | |||
| Sex | .89 | .06 | .10 | |||
| Female | 12.60±11.7 | 11.49±8.3 | 8.50±10.7 | |||
| Male | 12.98±14.1 | 18.29±13.8 | 20.76±18.2 | |||
| DM | .76 | .10 | .46 | |||
| Diabetic patients | 13.41±18.2 | 14.54±10.5 | 8.10±13.9 | |||
| Non-diabetic patients | 12.46±9.7 | 8.55±7.5 | 13.78±14.2 | |||
| Age | .08 | .68 | .74 | |||
| <45 years | 10.14±1.2 | 12.20±2.0 | 10.74±3.2 | |||
| >45 years | 14.21±2.0 | 13.61±2.1 | 13.07±5.4 | |||
| BMI | .03 | .95 | .09 | |||
| <40kg/m2 | 8.06±12.3 | 13.21±1.6 | 5.58±4.2 | |||
| >40kg/m2 | 16.03±1.6 | 13.09±2.7 | 16.68±4.5 | |||
| Obesity | .01 | .50 | .11 | |||
| Obesity I | – | – | – | |||
| Obesity II | 6.03±9.8 | 11.88±6.7 | 5.58±11.1 | |||
| Morbid obesity | 15.55±12.0 | 14.03±12.1 | 16.68±14.4 | |||
| Supermorbid obesity | 24.77±14.9 | – | – | |||
Bivariate analysis with t-test (or ANOVA).
DM, diabetes mellitus; B, BMI 40–49.9; supermorbid obesity, BMI>50.
The influence of overweight loss on the change in fasting blood sugar (P=.008) (r=0.289) is confirmed, as shown in Fig. 2.
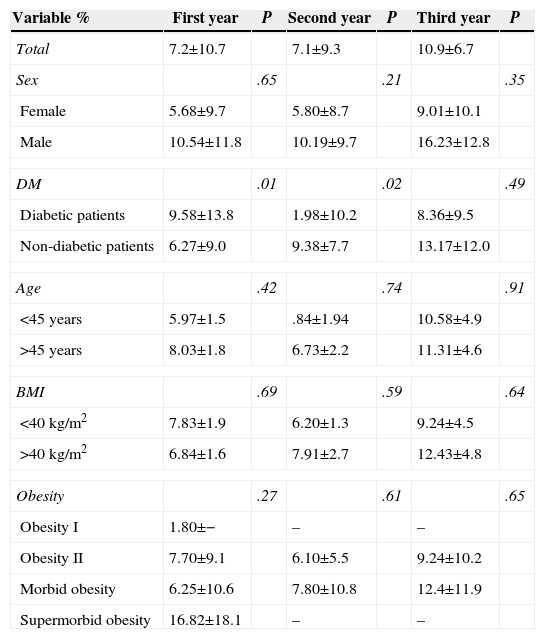
Total change in HbA1c was 7.2±10% in the first year and 7.1±9.3 and 10.9±6.7% in the second and third years, respectively. The preoperative diabetes status is considered a factor of less change in postoperative glycated haemoglobin compared to preoperative glycated haemoglobin in the second year of follow-up. This finding of the bivariate study reflected in Table 4 could not be confirmed with the logistic regression model (P=.07; OR=0.67).
Prognostic Factors of Changes in HbA1c.
| Variable % | First year | P | Second year | P | Third year | P |
|---|---|---|---|---|---|---|
| Total | 7.2±10.7 | 7.1±9.3 | 10.9±6.7 | |||
| Sex | .65 | .21 | .35 | |||
| Female | 5.68±9.7 | 5.80±8.7 | 9.01±10.1 | |||
| Male | 10.54±11.8 | 10.19±9.7 | 16.23±12.8 | |||
| DM | .01 | .02 | .49 | |||
| Diabetic patients | 9.58±13.8 | 1.98±10.2 | 8.36±9.5 | |||
| Non-diabetic patients | 6.27±9.0 | 9.38±7.7 | 13.17±12.0 | |||
| Age | .42 | .74 | .91 | |||
| <45 years | 5.97±1.5 | .84±1.94 | 10.58±4.9 | |||
| >45 years | 8.03±1.8 | 6.73±2.2 | 11.31±4.6 | |||
| BMI | .69 | .59 | .64 | |||
| <40kg/m2 | 7.83±1.9 | 6.20±1.3 | 9.24±4.5 | |||
| >40kg/m2 | 6.84±1.6 | 7.91±2.7 | 12.43±4.8 | |||
| Obesity | .27 | .61 | .65 | |||
| Obesity I | 1.80±− | – | – | |||
| Obesity II | 7.70±9.1 | 6.10±5.5 | 9.24±10.2 | |||
| Morbid obesity | 6.25±10.6 | 7.80±10.8 | 12.4±11.9 | |||
| Supermorbid obesity | 16.82±18.1 | – | – | |||
Bivariate analysis with t-test (or ANOVA).
DM, diabetes mellitus; BMI, body mass index; O, obesity; Obesity I, BMI 30–34.9; Obesity II, BMI 35–39.9; morbid obesity, BMI 40–49.9; supermorbid obesity: BMI>50.
The analysis of weight loss related to changes in glycated haemoglobin highlights the influence of the former (P=.021) (r=0.188), as shown in Fig. 3.
The analysis of the need for antidiabetic treatment through the modified diabetes status score points to preoperative sex, age, degree of obesity, and BMI as statistically significant predictive factors (see Table 5). At the end of the first year of follow-up, 61% of our patients had experienced an improvement in their status score and 29.4% had discontinued the antidiabetic treatment. During the follow-up period, diabetic patients with less than 5 years of progress decreased an average of one point in status score, while those who had diabetes with more than 5 years of progress decreased 0.80±0.3 points in average in the first year (P=.001) and 0.14±0.4 points in the second year (P=.078).
Factors Associated With an Improvement in the Diabetes Status Score.
| Variable % (n) | First year | P | Second year | P | Third year | P | |||
|---|---|---|---|---|---|---|---|---|---|
| total | 49.4 (43) | 50.6 (44) | 46.3 (19) | 53.7 (22) | 43.7 (7) | 56.3 (9) | |||
| ≤1 point | >1 point | ≤1 point | >1 point | ≤1 point | >1 point | ||||
| Sex | .05 | .89 | .77 | ||||||
| Female | 54.8 (34) | 45.2 (28) | 46.9 (15) | 53.1 (17) | 41.7 (5) | 58.3 (7) | |||
| Male | 36 (9) | 64 (16) | 44.4 (4) | 55.6 (5) | 50 (2) | 50 (2) | |||
| Age | .05 | .75 | .28 | ||||||
| <45 years | 44.1 (15) | 55.9 (19) | 42.9 (6) | 57.1 (8) | 28.6 (2) | 71.4 (5) | |||
| ≥45 years | 52.8 (28) | 47.2 (25) | 48.1 (13) | 51.9 (14) | 55.6 (5) | 44.4 (4) | |||
| BMI | .00 | .63 | .33 | ||||||
| ≤40kg/m2 | 73 (27) | 27 (10) | 55.0 (11) | 45.0 (9) | 83.3 (5) | 16.7 (1) | |||
| >40kg/m2 | 32.0 (16) | 68.0 (34) | 47.6 (10) | 52.4 (11) | 60 (6) | 40 (4) | |||
| Obesity | .01 | .85 | .33 | ||||||
| Obesity I | 100 (1) | 0 (0) | – | – | – | – | – | ||
| Obesity II | 72.4 (21) | 27.6 (8) | 52.9 (9) | 47.1 (8) | 83.3 (5) | 16.7 (1) | |||
| Morbid obesity | 37.7 (20) | 62.3 (33) | 50 (12) | 50 (12) | 60 (6) | 40 (4) | |||
| Supermorbid obesity | 25 (1) | 75 (3) | – | – | – | – | – | ||
Bivariate analysis with Chi-square test (or Fisher's exact test). Changes in diabetes status score have been categorised based on the fact that the difference from the preoperative status is greater or less than one point.
DM: diabetes mellitus; BMI: body mass index; O, obesity; Obesity I, BMI 30–34.9; Obesity II, BMI 35–39.9; morbid obesity, BMI 40–49.9; supermorbid obesity, BMI>50.
The analysis performed through binary logistic regression points to female sex and BMI<40kg/m2 as factors of less improvement (OR: 0.27 and 0.99), while age<45 years favoured remission of diabetes status (OR: 3.18) (see Table 6).
Remission and ImprovementResults in terms of improvement of diabetes during the follow-up period were 17.6% in the first year; 12.5% in the second year; and 34% in the third year. Complete remissions occur in 29.4% in the first year; 34% in the second year; and 37.5% in the third year of follow-up. All of them occurred in patients who initially took oral antidiabetics and none of them occurred in patients treated with insulin.
DiscussionWeight loss is the fundamental mechanism by which restrictive surgery increases insulin sensitivity. It has been shown that at least 30% weight loss provides a significant improvement or even DM remission.9 Such mechanism involves the decrease in chronically elevated inflammatory mediators in obese patients.3 The statistical analysis of our population confirms the obesity–diabetes relationship by showing, on the one hand, that patients with a higher degree of obesity have greater improvements in glucidic metabolism and, on the other hand, the circumstance indicated by other authors10 related to the fact that diabetic patients tend to less ponderal loss.
Regarding the studied predictive factors, for some authors, male sex would be a favourable factor for diabetes remission. Despite the fact that this has not been consistently shown in all the studies,11 we do state that there is a positive trend towards a decrease in fasting blood sugar and glycated haemoglobin associated with the male sex.
As is clear in this paper, age is an unfavourable predictive factor for resolution of diabetes. This seems to occur due to the fact that older age is associated with higher progression of impaired pancreatic β-cells. Such impairment reaches a critical point from which weight loss itself does not produce significant improvements in glucidic metabolism.12
There is vast literature that shows results of diabetes remission with gastric band surgery around 50%.13–16 Criteria used in different studies are heterogeneous, which makes comparison difficult. Keogh et al.15 show a remission rate of 16% understood as HbA1c<6.5% in the absence of treatment. Moreover, Dixon et al.14,16 in a recent systematic revision show remission rates ranging from 53% to 70%. However, just a few studies provide reliable results since ADA defined the concepts of partial remission, complete remission, prolonged remission and improvement. In this paper, we showed improvement rates up to 34% and complete remission rates up to 37.5% in the third year.
Duration of diabetes before the surgical treatment is one of the negative predictive factors more unanimously pointed out in literature.12,17–20 Although there is no agreement on the point in diabetes duration from which it turns more refractory, we have proved that diabetic patients with more than five years of progress had less improvement in their antidiabetic treatment.
Likewise, the use of insulin before surgery has been associated with a lower remission rate.11 In our analysis, no patient under insulin treatment reached complete remission; this may be due to the fact that the need for preoperative insulin therapy involves greater prior impairment of pancreatic β-cells.4 This effect relating to the deficit in insulin production in diabetic patients becomes evident in the lower proportion of decreases in HbA1c they reach, compared to non-diabetic patients in our paper.
It should be noted that the retrospective nature of this study is considered a limitation. This makes information analysis difficult and restricts its extrapolation to clinical practice. However, in spite of this limitation, the results of percentage of weight loss and diabetes remission are close to those obtained in some prospective studies.8
Since bariatric surgery is one that seeks highly concrete results in terms of ponderal loss and glycemic improvements, it is essential to perform an adequate selection of patients. In view of our results, we can conclude that with the adjustable gastric band, weight loss is the fundamental mechanism for optimisation of diabetes. This improvement in glucidic metabolism is clinically evident through the decreases in fasting blood sugar and glycated haemoglobin, but especially in the reduced need for treatment. For such reason, young male patients with a high BMI have significantly better results with the gastric band surgery.
Nevertheless, these results should be confirmed with studies including a higher number of patients and also longer follow-up, in order to come to conclusions with a greater statistical power and extrapolation to long-term results.
Conflict of InterestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Colsa Gutiérrez P, Kharazmi Taghavi M, Sosa Medina R, Gutiérrez Cabezas JM, Ovejero Gómez VJ, Ruiz JL, et al. Factores predictivos en resolución de insulinorresistencia con cirugía de banda gástrica ajustable. Cir Esp. 2015;93:159–165.