Residents in our country have achieved a homogenous surgical training by following a structured residency program. This is due to the existence of specific training programs for each specialty. The current program, approved in 2007, has a detailed list of procedures that a surgeon should have performed in order to complete training. The aim of this study is to analyze the applicability of the program with regard to the number of procedures performed during the residency period.
Material and methodsA data collection form was designed that included the list of procedures from the program of the specialty; it was sent in April 2014 to all hospitals with accredited residency programs. In September 2014 the forms were analyzed, and a general descriptive study was performed; a subanalysis according to the resident's sex and Autonomous region was also performed. The number of procedures performed according to the number of residents in the different centers was also analyzed.
ResultsThe survey was sent to 117 hospitals with accredited programs, which included 190 resident places. A total of 91 hospitals responded (53%). The training offered adapts in general to the specialty program. The total number of procedures performed in the different sub-areas, in laparoscopic and emergency surgery is correct or above the number recommended by the program, with the exception of esophageal-gastric and hepatobiliary surgery. The sub-analysis according to Autonomous region did not show any significant differences in the total number of procedures, however, there were significant differences in endocrine surgery (P=.001) and breast surgery (P=.042). A total of 55% of residents are female, with no significant differences in distribution in Autonomous regions. However, female surgeons operate more than their male counterparts during the residency period (512±226 vs 625±244; P<.01). The number of residents in the hospital correlates with the number of procedures performed; the residents with more procedures trained in hospitals where there were less residents (669±237 vs 527±209; P=.004).
ConclusionThe surgical activity performed by Spanish surgeons is adequate to the specialty program, except in hepatobiliary and esophageal-gastric surgery. The distribution is homogeneous in the different autonomous regions, although there are differences that depend on the number and sex of the residents in each hospital. This information is essential to evaluate the quality of the specialty program and to design new training programs.
El entrenamiento quirúrgico siguiendo un periodo de residencia ha conseguido que los residentes en nuestro país posean una formación homogénea y satisfactoria para el desarrollo de su actividad profesional. Ello se debe a la existencia de planes de formación específicos para cada especialidad. El plan vigente promulgado en 2007 detallaba el número mínimo de intervenciones quirúrgicas y procedimientos que un cirujano debía haber efectuado para completar su periodo de formación. El objetivo de este estudio es conocer la aplicación del programa de la especialidad en cuanto al número de intervenciones practicadas durante el periodo de residencia.
Material y métodosSe diseñó una hoja de recogida de datos que incluía la relación de intervenciones enunciada en el programa de la especialidad, que fue remitida en abril de 2014 a todos los hospitales que disponen de unidades acreditadas para la formación de residentes. En septiembre de 2014 se tabularon las respuestas remitidas y se efectuó un estudio estadístico descriptivo general, y un subanálisis en función del sexo del residente y de la comunidad autónoma. A la vez se analizó la actividad efectuada en función del número de residentes que existiera en cada unidad docente acreditada.
ResultadosLa encuesta se remitió a los 117 hospitales con unidades acreditadas, que incluyen un total de 190 plazas ofertadas. De ellas se obtuvieron 91 respuestas (53%). La formación ofrecida se adapta en líneas generales a la propuesta por el plan de la especialidad. El número global de intervenciones practicadas de acuerdo a las diferentes subáreas, en cirugía laparoscópica y de urgencias, cumple o supera las cifras previstas, excepto en cirugía esofagástrica y HPB. El subanálisis de la actividad quirúrgica según la comunidad autónoma no evidencia diferencias significativas en el número total de intervenciones, sin embargo, sí se objetivan diferencias en cirugía endocrina (p=0,001) y de la mama (p=0,042). Un 55% de los residentes eran mujeres, sin diferencias significativas en cuanto a su distribución en las comunidades autónomas. Sin embargo, las cirujanas operan más que los cirujanos durante la residencia (625±244 vs. 527±209; p<0,01). También se observa que el número de residentes adscrito a cada unidad docente se correlaciona con el número de intervenciones realizadas: han efectuado más intervenciones los cirujanos que están solos en su unidad que aquellos que tienen compañeros de su mismo año (669±237 vs. 527±209; p=0,004).
ConclusiónLa actividad quirúrgica efectuada por los cirujanos españoles se adecua a la propuesta por el plan actual de la especialidad, excepto en cirugía HPB y esofagogástrica. La distribución es homogénea de acuerdo a las comunidades autónomas, aunque existen diferencias en función del número de residentes por hospital y el sexo del residente. Esta información es esencial para evaluar la idoneidad del plan de formación y el diseño de nuevos planes formativos.
In Spain, the application of a surgical training program following a structured residency has meant that specialists in General and Gastrointestinal Surgery in our country have satisfactory, homogenous training to perform their professional activity. This important progress in medical training is undoubtedly due to the introduction of the Spanish MIR residency system more than 30 years ago and the development of specific training programs for each medical specialty.1
Due to the recently published Decree for compulsory educational requirements,2,3 we are currently on the verge of conceptual and structural changes of the training model for medical specialties. Nonetheless, it has only been 7 years since the current specialty program was initiated, and only two resident groups have completed their full training period in accordance with the current plan (2009–2013 and 2010–2014). This plan, which was developed in 2007, included important advances and modifications in training concepts, detailed basic information that surgeons should master, courses and rotations, and an important emphasis on research experience. Meanwhile, it defined the minimum number of surgical interventions and procedures that a surgeon is required to perform before completion of the training period.
Logically, any training program should be audited in order to determine its true applicability. Furthermore, it should be submitted to continuous evaluation to identify its strong points and/or defects.4,5 The National Medical Specialty Commission sent out an evaluation questionnaire to all the training units at Spanish teaching hospitals in April 2013, but the lack of uniformity in the responses obtained encumbered proper analysis. Therefore, a new, structured survey was sent out in April 2014 in order to analyze the applicability of the medical specialty program and the number of procedures done during residency. The data will enable us to know how the program has been adapted to the surgical reality in teaching units, and, based on this information, minimal requirements can be modified or adapted. Reference data will also be compiled to aid us in designing the future medical specialty plan in accordance with the new Decree on core requirements.
Material and MethodsThe National Medical Specialty Commission, which was in place up to June 2014, designed a data collection survey that included the interventions listed in the surgical specialty program, as well as the minimum number of interventions that surgery residents should have performed or should have assisted during the 5-year residency. This document, together with a request for it to be filled out and returned to the Commission office, was sent out in April 2014 (along with a reminder in June) to all the teaching hospitals that currently have accredited resident training units.
In September 2014, the responses returned to the Commission were tabulated. A general descriptive statistical study was generated. Afterwards, a subanalysis was completed for the distribution of the activity according to resident sex, Spanish autonomous community (i.e. province) and surgical subarea (gastroesophageal, coloproctological, hepato-pancreato-biliary, endocrine, breast, abdominal wall, laparoscopic, and emergency surgeries). Meanwhile, we also generated an analysis that correlated the surgical activity per resident and the number of residents involved in each accredited teaching unit.
The data analysis was calculated with the SPSS 20.0® statistical program. A univariate analysis of the data was created using the t-test, χ2 and ANOVA, as necessary. A P value of less than .05 was considered statistically significant.
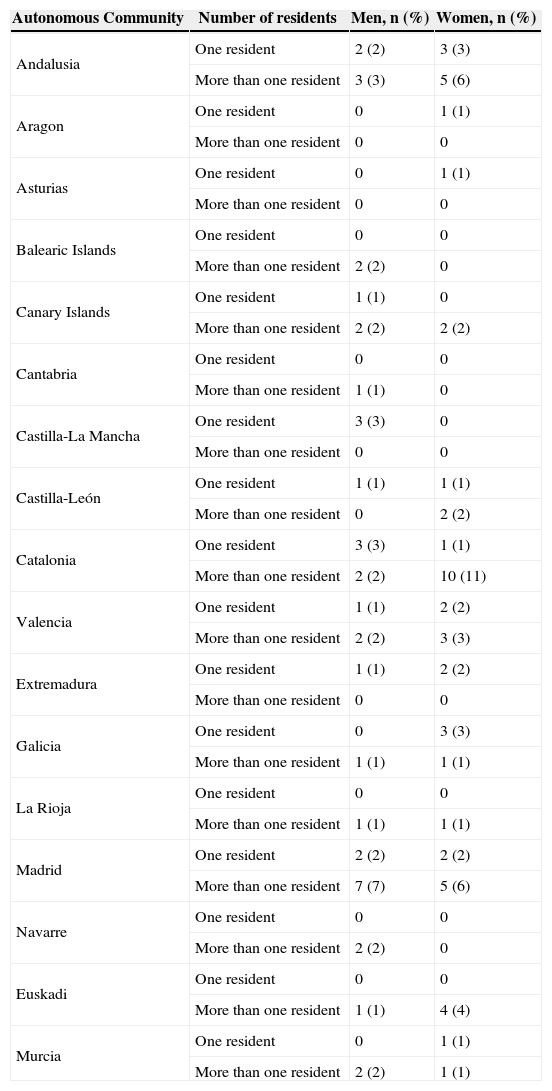
ResultsThe survey was sent to the 117 hospitals with accredited teaching units, which offered a total of 190 residency positions (Table 1). Twelve hospitals reported that they had no 5th year residents in 2014, so the total number of potential responses was 178. A total of 91 responses (53%) were received.
Distribution of the General Surgery Residents Who Completed the Survey According to Region/Autonomous Community.
| Autonomous Community | No. | % |
|---|---|---|
| Andalusia | 13 | 14 |
| Aragon | 1 | 1 |
| Asturias | 1 | 1 |
| Balearic Islands | 2 | 2 |
| Canary Islands | 5 | 6 |
| Cantabria | 1 | 1 |
| Castilla-La Mancha | 3 | 3 |
| Castilla-León | 4 | 4 |
| Catalonia | 16 | 18 |
| Valencia | 8 | 9 |
| Extremadura | 3 | 3 |
| Galicia | 5 | 6 |
| La Rioja | 2 | 2 |
| Madrid | 16 | 18 |
| Navarre | 2 | 2 |
| Euskadi | 5 | 6 |
| Murcia | 4 | 4 |
| Total | 91 | 100 |
Table 2 shows the regional distribution, resident sex, and number of residents per unit. Tables 3–5 demonstrate the mean±standard deviation of the number of operations performed by residents during their residency.
Distribution of the Residents According to Region/Autonomous Community, Number of Residents per Teaching Unit and Sex.
| Autonomous Community | Number of residents | Men, n (%) | Women, n (%) |
|---|---|---|---|
| Andalusia | One resident | 2 (2) | 3 (3) |
| More than one resident | 3 (3) | 5 (6) | |
| Aragon | One resident | 0 | 1 (1) |
| More than one resident | 0 | 0 | |
| Asturias | One resident | 0 | 1 (1) |
| More than one resident | 0 | 0 | |
| Balearic Islands | One resident | 0 | 0 |
| More than one resident | 2 (2) | 0 | |
| Canary Islands | One resident | 1 (1) | 0 |
| More than one resident | 2 (2) | 2 (2) | |
| Cantabria | One resident | 0 | 0 |
| More than one resident | 1 (1) | 0 | |
| Castilla-La Mancha | One resident | 3 (3) | 0 |
| More than one resident | 0 | 0 | |
| Castilla-León | One resident | 1 (1) | 1 (1) |
| More than one resident | 0 | 2 (2) | |
| Catalonia | One resident | 3 (3) | 1 (1) |
| More than one resident | 2 (2) | 10 (11) | |
| Valencia | One resident | 1 (1) | 2 (2) |
| More than one resident | 2 (2) | 3 (3) | |
| Extremadura | One resident | 1 (1) | 2 (2) |
| More than one resident | 0 | 0 | |
| Galicia | One resident | 0 | 3 (3) |
| More than one resident | 1 (1) | 1 (1) | |
| La Rioja | One resident | 0 | 0 |
| More than one resident | 1 (1) | 1 (1) | |
| Madrid | One resident | 2 (2) | 2 (2) |
| More than one resident | 7 (7) | 5 (6) | |
| Navarre | One resident | 0 | 0 |
| More than one resident | 2 (2) | 0 | |
| Euskadi | One resident | 0 | 0 |
| More than one resident | 1 (1) | 4 (4) | |
| Murcia | One resident | 0 | 1 (1) |
| More than one resident | 2 (2) | 1 (1) |
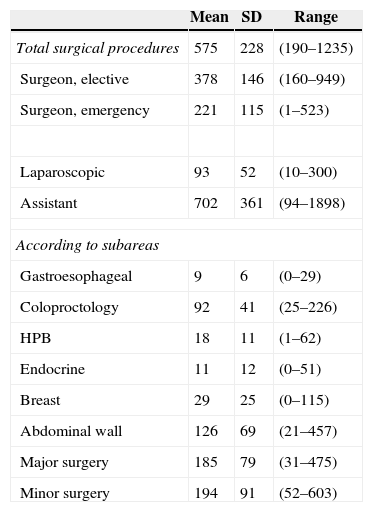
Summary of Surgical Activity of the Residents From the 2010 to 2014 Program.
| Mean | SD | Range | |
|---|---|---|---|
| Total surgical procedures | 575 | 228 | (190–1235) |
| Surgeon, elective | 378 | 146 | (160–949) |
| Surgeon, emergency | 221 | 115 | (1–523) |
| Laparoscopic | 93 | 52 | (10–300) |
| Assistant | 702 | 361 | (94–1898) |
| According to subareas | |||
| Gastroesophageal | 9 | 6 | (0–29) |
| Coloproctology | 92 | 41 | (25–226) |
| HPB | 18 | 11 | (1–62) |
| Endocrine | 11 | 12 | (0–51) |
| Breast | 29 | 25 | (0–115) |
| Abdominal wall | 126 | 69 | (21–457) |
| Major surgery | 185 | 79 | (31–475) |
| Minor surgery | 194 | 91 | (52–603) |
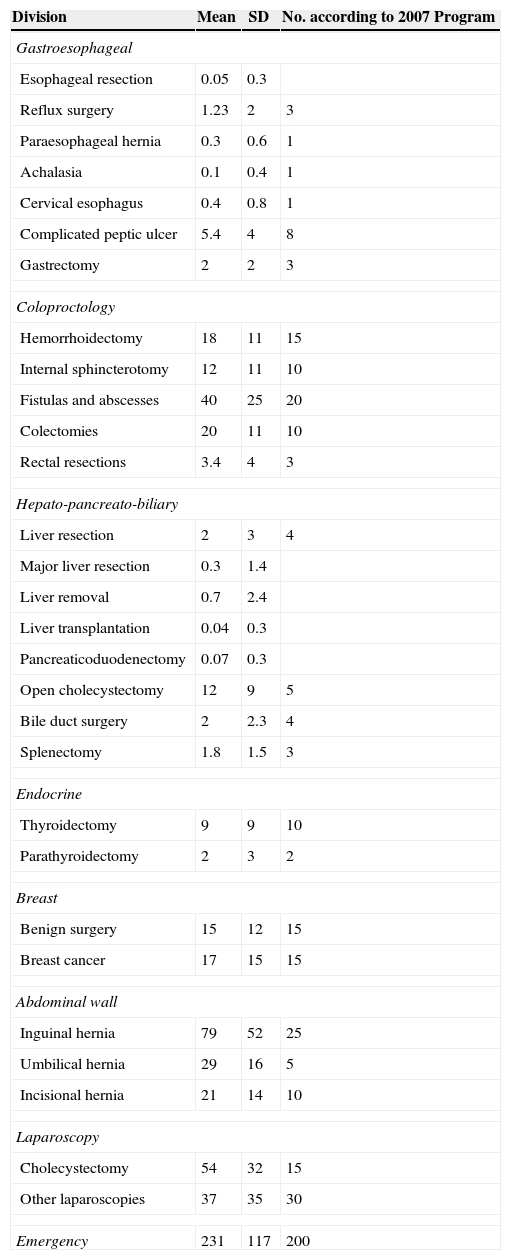
Mean Activity Per Surgeon.
| Division | Mean | SD | No. according to 2007 Program |
|---|---|---|---|
| Gastroesophageal | |||
| Esophageal resection | 0.05 | 0.3 | |
| Reflux surgery | 1.23 | 2 | 3 |
| Paraesophageal hernia | 0.3 | 0.6 | 1 |
| Achalasia | 0.1 | 0.4 | 1 |
| Cervical esophagus | 0.4 | 0.8 | 1 |
| Complicated peptic ulcer | 5.4 | 4 | 8 |
| Gastrectomy | 2 | 2 | 3 |
| Coloproctology | |||
| Hemorrhoidectomy | 18 | 11 | 15 |
| Internal sphincterotomy | 12 | 11 | 10 |
| Fistulas and abscesses | 40 | 25 | 20 |
| Colectomies | 20 | 11 | 10 |
| Rectal resections | 3.4 | 4 | 3 |
| Hepato-pancreato-biliary | |||
| Liver resection | 2 | 3 | 4 |
| Major liver resection | 0.3 | 1.4 | |
| Liver removal | 0.7 | 2.4 | |
| Liver transplantation | 0.04 | 0.3 | |
| Pancreaticoduodenectomy | 0.07 | 0.3 | |
| Open cholecystectomy | 12 | 9 | 5 |
| Bile duct surgery | 2 | 2.3 | 4 |
| Splenectomy | 1.8 | 1.5 | 3 |
| Endocrine | |||
| Thyroidectomy | 9 | 9 | 10 |
| Parathyroidectomy | 2 | 3 | 2 |
| Breast | |||
| Benign surgery | 15 | 12 | 15 |
| Breast cancer | 17 | 15 | 15 |
| Abdominal wall | |||
| Inguinal hernia | 79 | 52 | 25 |
| Umbilical hernia | 29 | 16 | 5 |
| Incisional hernia | 21 | 14 | 10 |
| Laparoscopy | |||
| Cholecystectomy | 54 | 32 | 15 |
| Other laparoscopies | 37 | 35 | 30 |
| Emergency | 231 | 117 | 200 |
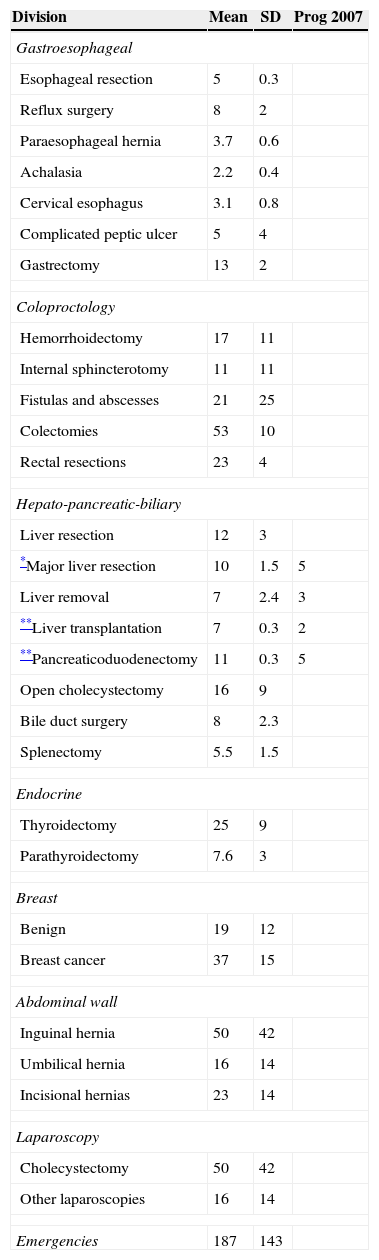
Mean Activity as Assistant.
| Division | Mean | SD | Prog 2007 |
|---|---|---|---|
| Gastroesophageal | |||
| Esophageal resection | 5 | 0.3 | |
| Reflux surgery | 8 | 2 | |
| Paraesophageal hernia | 3.7 | 0.6 | |
| Achalasia | 2.2 | 0.4 | |
| Cervical esophagus | 3.1 | 0.8 | |
| Complicated peptic ulcer | 5 | 4 | |
| Gastrectomy | 13 | 2 | |
| Coloproctology | |||
| Hemorrhoidectomy | 17 | 11 | |
| Internal sphincterotomy | 11 | 11 | |
| Fistulas and abscesses | 21 | 25 | |
| Colectomies | 53 | 10 | |
| Rectal resections | 23 | 4 | |
| Hepato-pancreatic-biliary | |||
| Liver resection | 12 | 3 | |
| *Major liver resection | 10 | 1.5 | 5 |
| Liver removal | 7 | 2.4 | 3 |
| **Liver transplantation | 7 | 0.3 | 2 |
| **Pancreaticoduodenectomy | 11 | 0.3 | 5 |
| Open cholecystectomy | 16 | 9 | |
| Bile duct surgery | 8 | 2.3 | |
| Splenectomy | 5.5 | 1.5 | |
| Endocrine | |||
| Thyroidectomy | 25 | 9 | |
| Parathyroidectomy | 7.6 | 3 | |
| Breast | |||
| Benign | 19 | 12 | |
| Breast cancer | 37 | 15 | |
| Abdominal wall | |||
| Inguinal hernia | 50 | 42 | |
| Umbilical hernia | 16 | 14 | |
| Incisional hernias | 23 | 14 | |
| Laparoscopy | |||
| Cholecystectomy | 50 | 42 | |
| Other laparoscopies | 16 | 14 | |
| Emergencies | 187 | 143 | |
The subanalysis of resident surgical activity by autonomous community showed no significant differences in the total number of surgeries. There were differences, however, in endocrine (P=.001) and breast (P=.042) surgeries.
In recent years, an absolute increase has been observed in the number of female medical students and in the proportion of residents of both sexes who choose surgery as their specialty. This fact was reflected in the survey, where we observed that 55% of the resident population were women and 45% were men. No significant differences were observed in regional distribution according to sex. We also observed that female surgeons operated more (in absolute values) than male surgeons during residency (625±244 vs 527±209; mean difference 113±51; P=.029).
It was also observed that the number of residents assigned to each teaching unit correlated with the total number of surgical procedures completed. Thus, surgeons who were alone in their units completed more surgeries than those who had colleagues in their same year (669±237 vs 527±209; mean difference 141±48; P=.004).
DiscussionPostgraduate training in surgery, especially in the specialization phase (residency), involves variable aspects related with the knowledge, skills, and professionalism that residents should integrate in a limited timeframe (5 years). At the same time, it requires adequate exposure to elective and urgent surgeries as well as familiarization with a series of diagnostic and therapeutic procedures (radiology, ultrasound, endoscopy, etc.). Training does not end when mere medical objectives are met; it should also include a solid base in the fundamentals of research. In spite of this fact, the nucleus of surgical activity is the operating room. The evaluation of surgical training, however, is complex. Inevitably, the number of procedures performed or assisted is an imperfect scale, although it does enable us to quantitatively define surgical learning. The results presented in this study allow us to better understand the application of the current surgical program.
An initial analysis of the results includes several considerations. First of all is the participation in the survey of residents and teaching units. This survey has been answered by a few more than half of the residents from the 2010 to 2014 MIR. Even though this percentage of responses allows us to have a reliable impression of the surgical training reality in Spain, the number of answers should be considered low. This is especially true since the survey is a requirement of the Commission, and its final objective is to evaluate and be able to improve the residency program. We must demand greater involvement and commitment from residents and teaching units because the evaluation process is essential to improve the residency period.
Second of all, a global assessment of the data leads to the conclusion that, in general, the training provided meets the requirements of the surgical specialty program. The overall number of operations done according to subareas, laparoscopic surgery and emergency procedures either meets or surpasses expected levels. This did not occur, however, in 2 very specific areas: gastroesophageal and hepato-pancreato-biliary (HPB) surgeries. There is a possible explanation for each subarea. The prevalence of patients with gastroesophageal disease is low, and most of these pathologies require a laparoscopic approach. Although its use is widespread, implementation is still low due to its technical complexity (according to a recently published survey with data from the last 25 years in Spain).6 As for HPB surgery, the greater technical complexity surely limits access of residents to this type of procedures. These data can justify the future development of specific skill areas, in keeping with the spirit of the core requirement decree.
The experience in laparoscopic surgery required in the initial program has been easily surpassed as a consequence of the success and universalization of these procedures. We should highlight the commitment of the Endoscopic Surgery Division of the AEC (Spanish Society of Surgeons) toward providing the courses in minimally invasive surgery required by the specialty program.
Finally, the data confirm the fact that Spanish surgeons are well trained in emergency procedures, which represent 36% of the operations performed.
As there were no differences observed in the number of surgeries per resident from the different autonomous communities, the results from this survey confirm a homogenous distribution among the accredited centers. There were differences, however, in resident gender and surgical activity. The progressive feminization of the specialty should be mentioned as the number of women surpassed that of men (55/45). Meanwhile, female surgeons in training operated more than their male colleagues, a finding that is more difficult to explain and should keep their male counterparts on their toes.
Another result that deserves mention is the fact that the residents who did their residency at hospitals accredited for only one resident per year operated significantly more than those who trained at larger or tertiary hospitals with more than one resident per year. This could be due to the completion of a greater number of less complex procedures or the greater agility and integration at smaller hospitals. This finding is of interest for the residency directors, who should be concerned with avoiding these differences and adjusting residents’ scheduling.
An aspect to keep in mind is that, even though no overall differences were observed in the number of procedures among autonomous communities and in most of the subareas analyzed, there was a significant difference in some autonomous communities regarding the number of endocrine or breast surgeries. This leads us to believe that, in some hospitals, these procedures may be done by other specialties instead of general surgery (ORL or gynecology).
Immediately after the publication of the program for the specialty, both the Training Division of the AEC7 as well as some regional surgical societies8 analyzed the possible difficulties involved in the application of said program. Some of these predictions correlated with the findings we have obtained.
In 2008, the Valencian Society of Surgery created a survey aimed at evaluating whether the accredited teaching hospitals could potentially meet the objectives proposed in the current surgical specialty plan.8 The survey for residency directors (n: 10) and residents from each year (n: 57) had a high level of participation (>90%) and identified the potential difficulties involved in the implementation of the program, basically having to do with the academic activities of each department. They also identified some aspects confirmed by our survey, especially regarding the difficulty to perform gastroesophageal and hepatobiliary procedures. Mention was also made of the possible difficulty to experience laparoscopic surgery, although this was not seen in our survey.
The Endoscopic Surgery Division of the AEC published 2 surveys done in 2010.7 These were sent to 626 residents and 142 tutors and had low response rates (19% and 29%). Out of the residents who responded, 32% were 1st year residents and only 7% were 5th year, which means that these results should be evaluated with caution. The overriding opinion of the residents was support for the specialty program, and that surgical activity had followed the plan proposals.
The assessment of the 2 previous studies and the results from this survey demonstrate the lack of an objective method to compile data about residents’ surgical activity. The medical specialty Decree specifies the mandatory use of the “resident book” by all residents and instructors for monitoring resident's activity. Its use has not become widespread as per the Decree. The AEC and its Training Division designed a free-access resident book that can be obtained from the Society website. There are publications that demonstrate the interest in and the use of this instrument in Spain. Serra-Aracil et al. presented in 20099 and recently10 the use of this tool in the follow-up of residents’ activity, which is able to monitor activity and assess its adaptation to the indications of the Decree. Meanwhile, in 2012, Cirugía Española published the results of a multicenter study carried out in 10 Spanish hospitals that registered residents’ activity over a 6-month period.11 Both experiences, the short-term multicenter study (6 months) as well as the long-term single-center one, demonstrated the usefulness of this continuous evaluation instrument for reaching the objectives detailed in the specialty plan. A possible disadvantage is the lack of a centralized activity register that would be able to evaluate overall resident activity. Obviously, one of the defects of this survey is that it was not completed by all the residents nationwide.
Our survey also has some weak points. The response was not universal, and the origin of the data reported cannot be certified. The observation of great variability in the number of interventions emphasizes the need for annual audits of the surgical activity carried out by each resident and the activity offered by each teaching unit. The development of computer programs and tools (apps) could facilitate and universalize this useful tool for monitoring and supervision.
The general surgery training program also includes other essential activities during the residency period, such as collaboration on scientific communications, scientific articles, participation at congress, and activities with other teaching units. These aspects have not been assessed in this survey, although they should be included in future surveys.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Targarona Soler EM, Jover Navalon JM, Gutierrez Saiz J, Turrado Rodríguez V, Parrilla Paricio P, en nombre de la Comisión Nacional de la Especialidad de Cirugía General y del Aparato Digestivo. ¿Qué operan los residentes españoles durante la residencia?: análisis de la aplicabilidad del programa de la especialidad de Cirugía General y Digestiva al finalizar el periodo de residencia. Cir Esp. 2015;93:152–158.
Members of the Comisión Nacional de la Especialidad: Eduardo M. Targarona, Antonio J. Torres, José Luis Gallego, David Pacheco, José Luis Salvador-Sanchis, Eugenio Hernández, José Luis Lucena, Francisco José del Riego, José M. Jover, Julia Piña, David Saavedra.