The objective is to study the medium-term results of angioplasty and stenting in the femoro-popliteal sector in patients with critical limb ischemia (CLI), and identify angiographic predictive factors of primary patency.
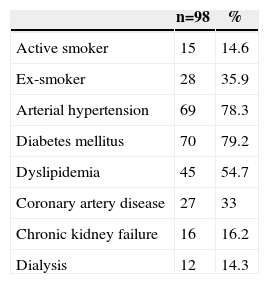
Patients and methodsRetrospective review of 98 patients with critical ischemia and angiographic lesions characterized as TASC A=13 (14%), B=38 (40%), C=24 (25%) or D=20 (21%). A total of 106 angioplasties and primary self-expanding stents (mean length of stent coverage of 19cm) were performed between January 2006 and January 2011.
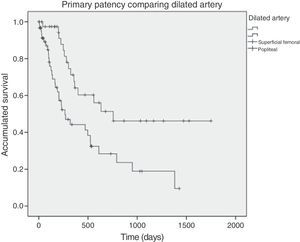
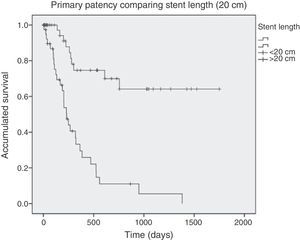
ResultsThe immediate results of patency, limb salvage and survival were 95, 96 and 96%, respectively. Primary patency at 1 and 2 years was 54 and 38%, respectively. Twenty-seven cases (25%) required endovascular iterative procedures, providing an assisted patency at 1 and 2 years of 72 and 60%, and a secondary patency of 80 and 67%. A lower primary patency was observed (log rank) when stent length was >20cm (P<.001), popliteal artery was involved (P=.004), and in TASC C and D lesions (P=.04). In multivariate analysis (Cox), only stent length >20cm was an independent negative predictor for primary patency (HR=5.7, P<.001). The limb salvage at 1 and 2 years was 83 and 81%, respectively.
ConclusionsAngioplasty with stent in the femoro-popliteal sector is a safe technique, but with significantly lower permeability results in injuries that require stent coverage of more than 20cm. In these cases, vein bypass surgery should be the procedure of choice.
Conocer los resultados a medio plazo de la angioplastia con stent del sector femoropoplíteo en pacientes con isquemia crítica e identificar aquellos factores angiográficos que inciden en la permeabilidad primaria.
Pacientes y métodosRevisión retrospectiva de 98 pacientes consecutivos con isquemia crítica y caracterizados angiográficamente como TASC A=13 (14%), B=38 (40%), C=24 (25%) y D=20 (21%), sobre los que se realizaron 106 angioplastias con implantación primaria de stents autoexpandibles entre 2006 y 2011.
ResultadosLos resultados inmediatos de permeabilidad, salvamento de extremidad y supervivencia fueron del 95, 96 y 96%, respectivamente. La permeabilidad primaria a 1 y 2 años fue del 54 y 38%, respectivamente. Veintisiete casos (25%) requirieron procedimientos endovasculares iterativos, determinando una permeabilidad asistida a 1 y 2 años del 72 y 60%, y secundaria del 80 y 67%. Se asociaron (log rank) a una menor permeabilidad primaria una longitud del stent mayor de 20cm (p<0,001), afectación de la arteria poplítea (p=0,004) y lesiones TASC C y D (p=0,04). En el análisis multivariable (Cox), solo una longitud de stent >20cm mostró carácter predictor independiente y negativo sobre la permeabilidad primaria (HR=5,7; p<0,001). El salvamento de extremidad a 1 y 2 años fue de 83 y 81%, respectivamente.
ConclusionesLa angioplastia con stent primario en el sector femoropoplíteo es una técnica segura aunque con unos resultados a medio plazo pobres en pacientes con isquemia crítica cuyas lesiones femoropoplíteas requieren una cobertura mayor de 20cm. En estos casos, el bypass con vena adecuada debería constituir la técnica de elección.
Arterial disease of the lower extremities is a frequent manifestation of systemic arteriosclerosis, and superficial femoral artery (SFA) and popliteal involvement is especially prevalent among these patients.1 Although the most frequent clinical manifestation is intermittent claudication, in cases of critical ischemia with pain while at rest or ischemic lesions there is a real risk of losing the extremity. Efforts at revascularization are directed at these situations.
Saphenous vein bypass has traditionally been the revascularization treatment of reference, with a reported 70% of extremities saved after 5 years.2,3 In recent years, the use of endovascular techniques has grown because they are less invasive procedures, and they have evolved immensely thanks to the advent of new materials and smaller devices. In fact, the Trans-Atlantic Inter-Society Consensus4 (TASC) document from 2007 indicates endovascular treatment as the first choice in TASC A femoro-popliteal lesions and as an alternative treatment in type B and C lesions.
The mid- to long-term results of endovascular treatment, however, continue to show less patency when compared with saphenous vein bypass.3 Meanwhile, these techniques require a higher number of assisted interventions to maintain competitive results. It is therefore necessary to identify what type of arterial lesions could most benefit from its application, thereby avoiding inadequate interventions. The objectives of this study were to assess the mid-term results of a consecutive series of patients with critical ischemia who were treated with angioplasty and primary implantation of a femoro-popliteal stent and to identify angiographic characteristics of arteriosclerotic lesions that could be predictive for the primary patency of the procedure.
Patients and MethodsWe retrospectively reviewed the cases of 98 consecutive patients with critical ischemia due to femoro-popliteal lesions during the period 2006–2011. Mean age was 74.2, and 60% of the patients were male. As is characteristic, 79.2% of the patients were diabetic and 14.3% were on dialysis. All patients presented critical ischemia with pain at rest (21%) or trophic lesions (79%). Table 1 shows other clinical characteristics of the patient sample.
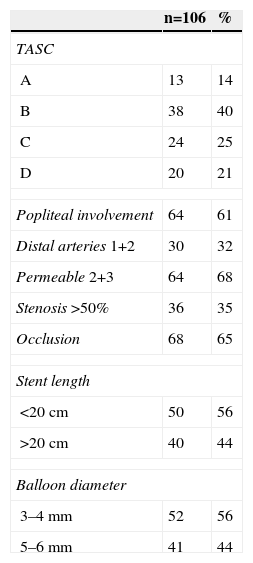
Out of these 98 patients, 106 angioplasties were performed (in 8 cases, both lower limbs were treated) with primary self-expanding nitinol stent implantation in the femoro-poplíteal sector. The angiographic characteristics of the treated lesions are specified in Table 2. In 9 cases, the TASC classification was not reliably established because complete angiographic examination was not available before the intervention. We excluded the cases in which there was associated treatment of the tibial arteries or popliteal lesions distal to the articular interline.
Angiographic Characteristics of the Treated Lesions.
| n=106 | % | |
|---|---|---|
| TASC | ||
| A | 13 | 14 |
| B | 38 | 40 |
| C | 24 | 25 |
| D | 20 | 21 |
| Popliteal involvement | 64 | 61 |
| Distal arteries 1+2 | 30 | 32 |
| Permeable 2+3 | 64 | 68 |
| Stenosis >50% | 36 | 35 |
| Occlusion | 68 | 65 |
| Stent length | ||
| <20cm | 50 | 56 |
| >20cm | 40 | 44 |
| Balloon diameter | ||
| 3–4mm | 52 | 56 |
| 5–6mm | 41 | 44 |
TASC: Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC-II).4
The procedures were performed by vascular surgeons in an operating room with a digital angiography system (Siemens Axiom Artis). Femoral puncture was contralateral in 87 cases (82%) and ipsilateral in the remainder. Angioplasty was performed under systemic heparinization (1mg per kg of weight of heparin sodium). The implanted stents were Smart Control (Cordis) in 97 (91%) cases. The rest were: 3 Maris Deep (Medtronic), 2 Zilver (Cook), 2 Absolute (Abbot), 1 Sinus (OptiMed) and 1 Lifestent (Bard). The mean implanted stent length was 19.1cm. Hemostasis of the puncture site was performed with the Starclose (Abbott) percutaneous device in 80 cases (76%) and the remainder by manual compression. Dual antiplatelet therapy was indicated for 3 months after the procedure. The endovascular technique was considered successful if follow-up angiography showed patency of the treated sector or a residual stenosis of less than 20%.
The patients were followed-up as outpatients in accordance with standard clinical and hemodynamic controls. The patency analysis was calculated by means of Kaplan–Meyer curves with the SPSS 15.0 program. For the inferential study of predictive characteristics for primary patency, an event was considered restenosis of more than 50% or occlusion of the technique. The variables included in the analysis were the artery treated (exclusively superficial femoral vs associated popliteal artery involvement), type of lesion (stenosis vs occlusion), run-off (2–3 vs 0–1 patent distal vessels), implanted stent length (<20 vs ≥20cm) and angioplasty balloon diameter (3–4 vs 5–6mm). TASC-II classifications of the lesions treated (A+B vs C+D) were also included. The factors that showed statistically significant association with primary patency were included in a multivariable analysis (Cox regression). A P value <.05 was considered statistically significant.
ResultsImmediate ResultsPatency after 30 days was 96%. Immediate local complications derived from the endovascular intervention were 5 minor hematomas, 1 femoral hemorrhage that required urgent surgical intervention and 5 pseudoaneurysms, 3 of which needed surgical correction.
Systemic medical complications included: 1 patient with respiratory failure, 1 congestive heart failure, 1 stroke, 1 upper gastrointestinal bleeding, 2 acute kidney failures and 5 patients with systemic sepsis. As a consequence of these complications, 4 patients (4%) died within the first 30 days after surgery: 2 due to sepsis, 1 acute renal failure (who did not meet criteria for hemodialysis), and 1 patient with massive gastrointestinal hemorrhage.
The limb salvage rate after 30 days was 96%.
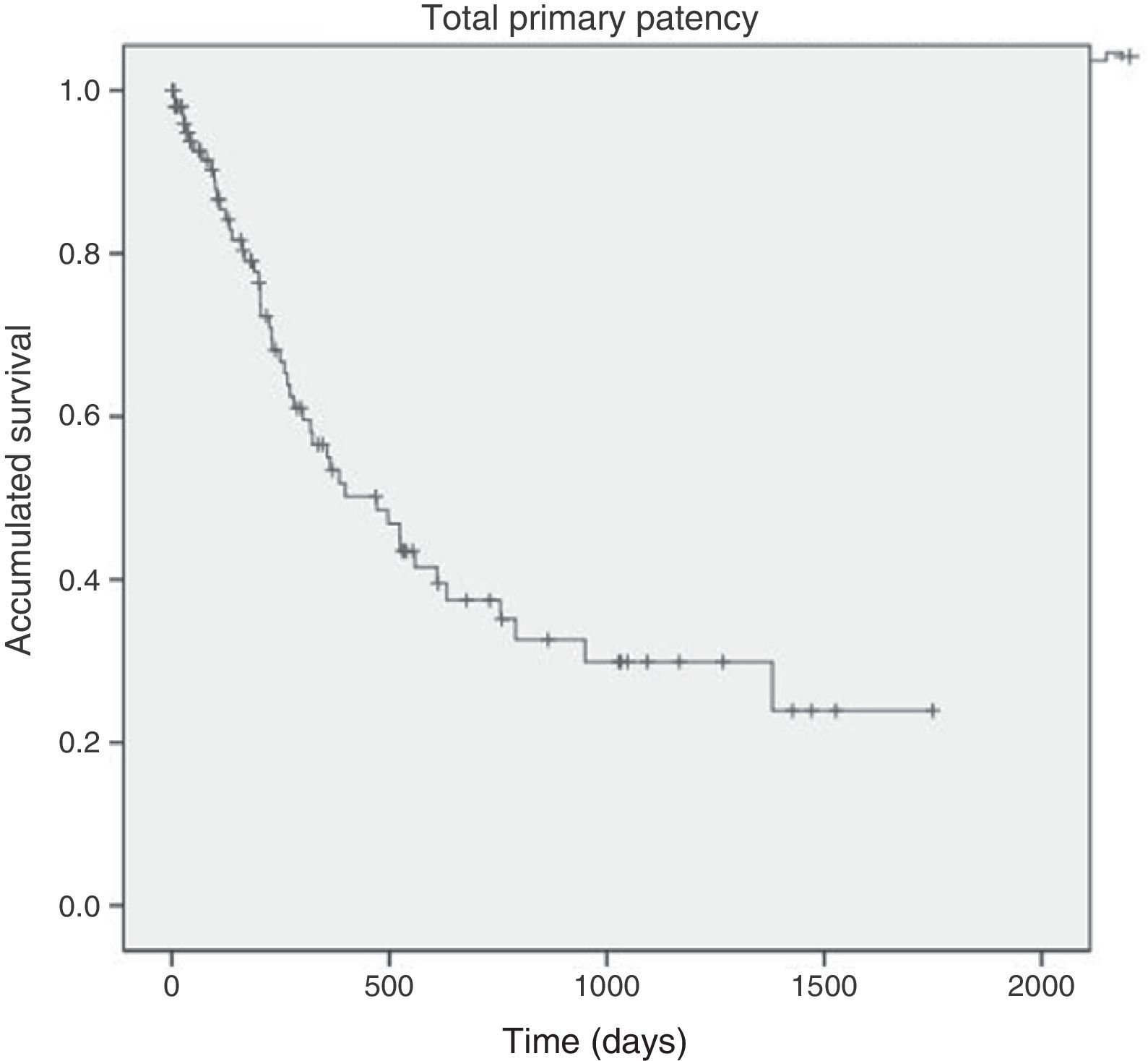
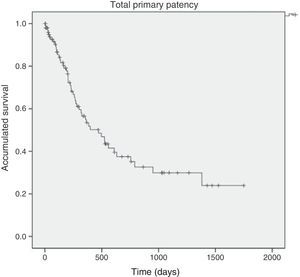
Patency Results and Follow-upMean follow-up was 24 months. Primary patency of the endovascular technique was 54% (±5.8) after one year and 38% (±6.1) after 2 years (Fig. 1). Twenty-seven patients required a repeat endovascular procedure (in 29 of the initial techniques 41 re-angioplasties were done), reaching an assisted patency after 1 and 2 years of 72% (±5.1) and 60% (±6.0), respectively, and secondary patency of 80% (±4.4) and 67% (±5.9), respectively. In 17 patients, conversion to bypass was necessary.
The one-year, two-year and three-year limb salvage rates were 83%, 81% and 77%, respectively. Fifteen patients required major amputation, although 9 were performed with permeable endovascular technique due to infectious complications in the area of the neurotrophic foot ulcers. One-, two- and three-year survival rates were 82, 74 and 68%, respectively.
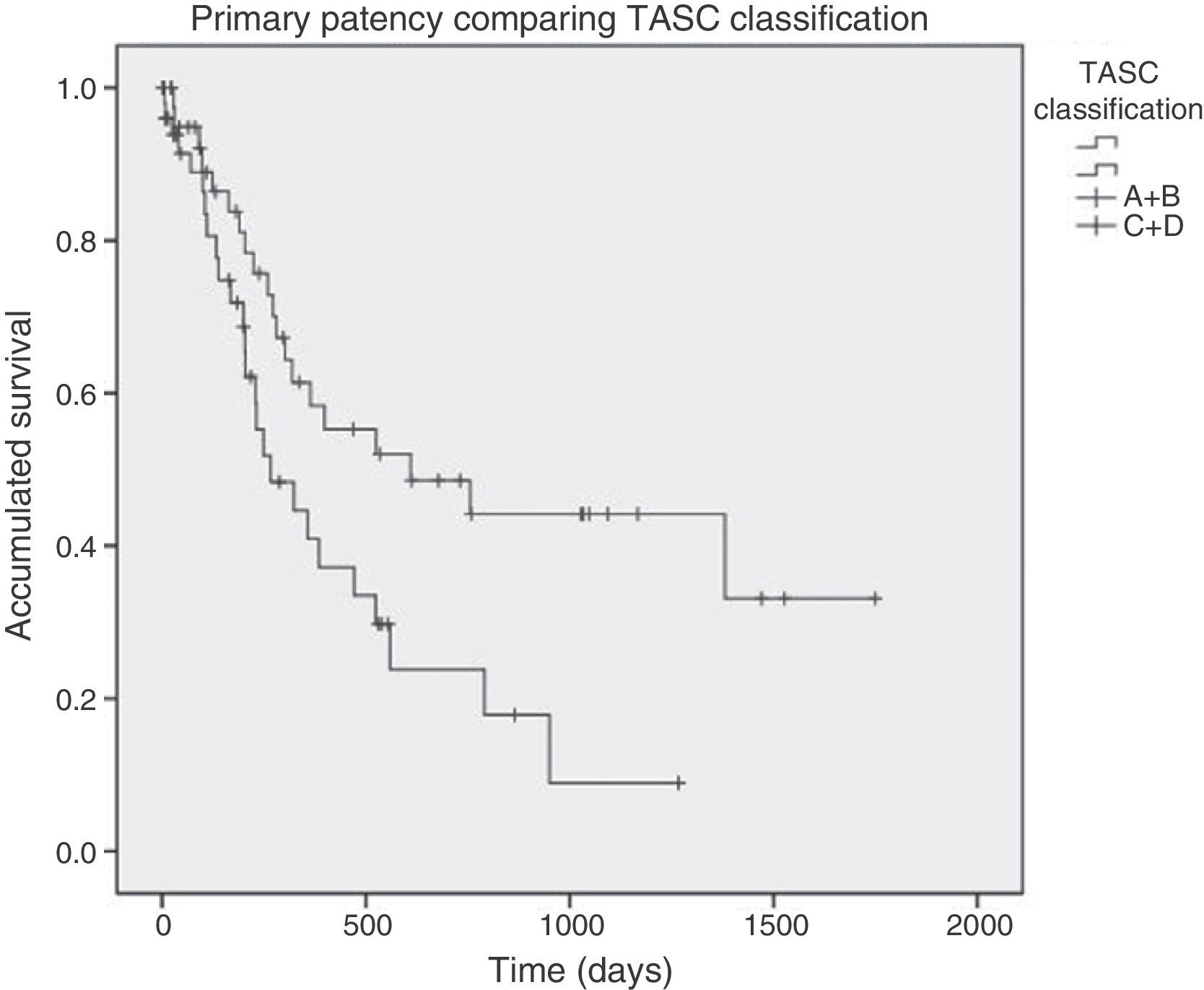
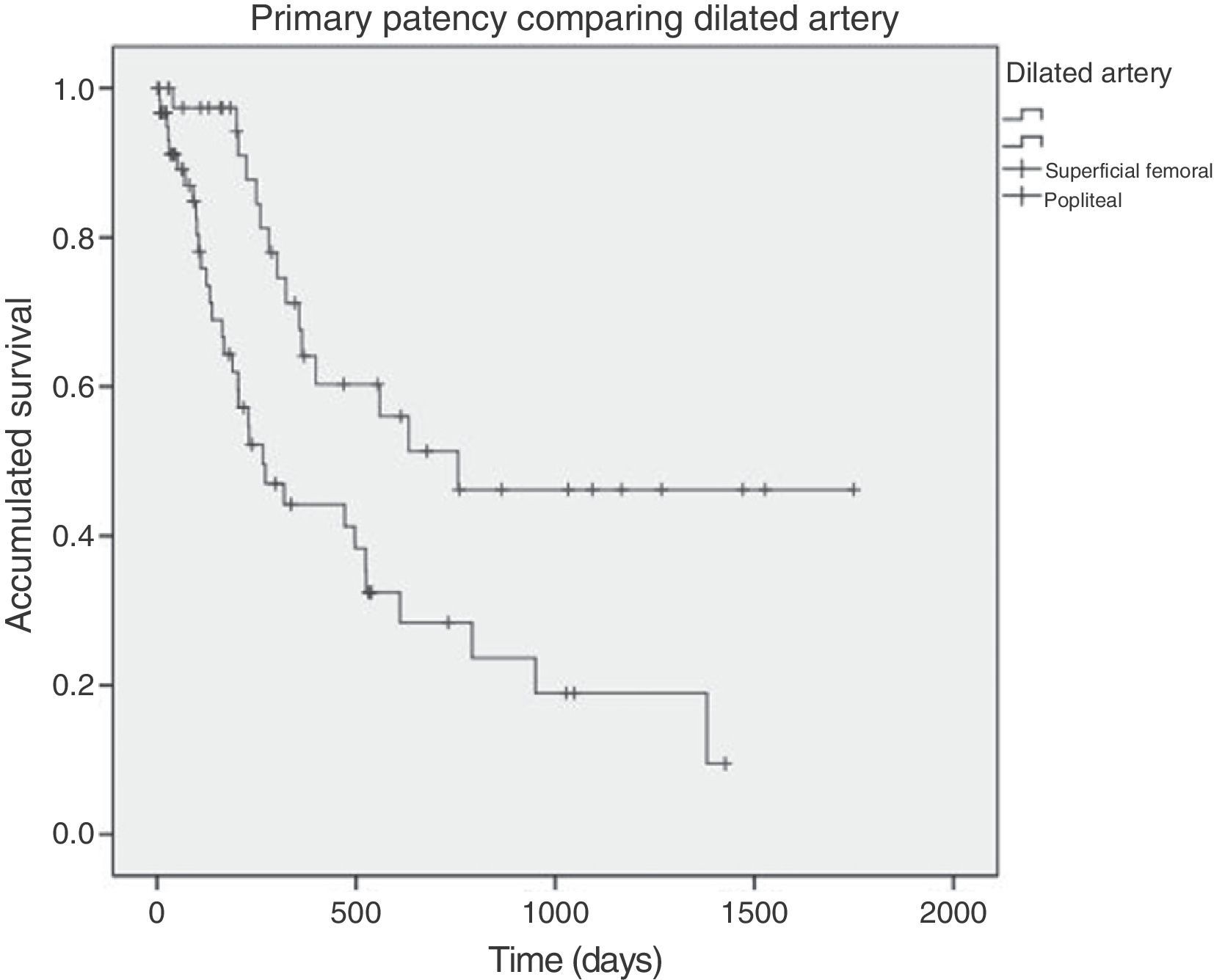
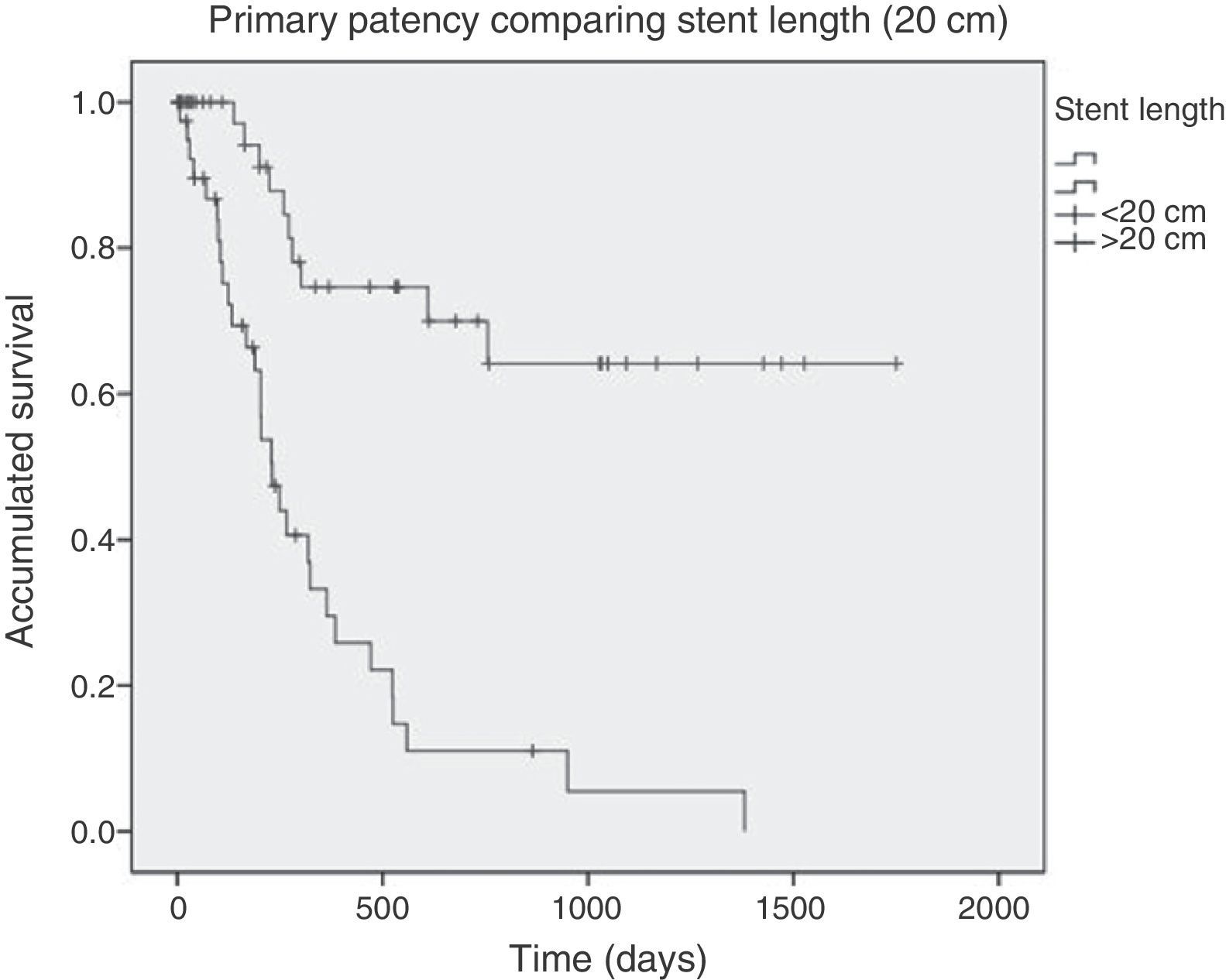
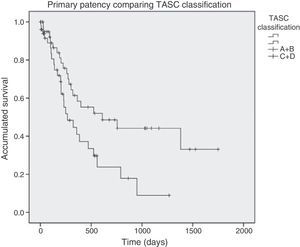
Lesion Characteristics That Predict Primary PatencyIn the bivariate study, primary patency values at 1 and 2 years associated with TASC C and D lesions were significantly lower than that observed in TASC A and B lesions (47/25 vs 59/49%; P=.04) (Fig. 2). Likewise, primary patency in those cases that required coverage of the popliteal artery was significantly lower (52/28 vs 65/44%; P=.004) (Fig. 3). Lastly, greater stent coverage was also significantly associated with primary patency, which was lower when the length treated was greater than 20cm (30/11 vs 76/70%; P<.001) (Fig. 4). Occlusive lesions and poor run-off were not associated with poorer patency results. In the multivariable analysis, only an implanted stent length greater than 20cm was an independent predictor for poor primary patency (RR=5.7; P<.001).
Comparison of primary patency of TASC A+B vs C+D lesions in angioplasty plus stenting of the femoro-popliteal region. TASC: Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC-II).4
Our study shows that the length of the artery covered by the stent is the most influential angiographic factor in stent patency in the femoro-popliteal sector of patients with critical ischemia. Although the TASC classification also takes into account the length of the lesion and is a predictor of patency in the bivariate analysis, an implanted stent length ≥20cm was more precisely and independently associated with primary patency. This finding has also been demonstrated in recent studies. In a series of 499 femoro-popliteal lesions treated with self-expanding nitinol stents, Han et al.6 observed poorer primary and assisted patency and a higher percentage of restenosis in patients with long lesions and TASC D. Taneja et al.7 reported permeabilities of 27% after one year in angioplasty of long lesions (mean 23.8cm). Moreover, the European Society of Vascular Surgery has recently published treatment guidelines for patients with critical ischemia,8 which propose planning the treatment of femoro-popliteal lesions not according to the TASC classification, but instead according to the length of the affected artery. For instance, lesions <5cm would be an indication for simple angioplasty and complementary stent implantation if the results were not satisfactory. In lesions between 5 and 15cm, angioplasty would be recommended with self-expanding stents. In lesions larger than 15cm, and especially in young patients or those with a life expectancy of more than 2 years, a saphenous vein bypass is recommended. In these longer lesions, endovascular treatment would only be indicated in patients with very high surgical risk or with no available vein. The results of our series concur with these recommendations for longer lesions because our results improved significantly when we selected the subgroup with a treated artery length of less than 20cm: one-year and two year primary permeabilities were 76 and 70%, respectively, versus 30 and 11% in patients with longer treated lesions. These results were obtained with self-expanding nitinol stents, which have been demonstrated to have better associated patency.5
Angioplasty with stenting of the femoro-popliteal region is considered a safe revascularization option with very low morbidity and mortality. Our results show that, although low, the morbidity and mortality rates associated with this procedure are not insignificant. Therefore, the procedure should be limited to cases in which the prospects for patency are satisfactory, especially when the competitive patency results in this sector are often reached with repeat endovascular procedures. The two-year percentages for secondary patency close to 70% are similar to those obtained with saphenous vein bypass (>70 after 2 years3,9), and they surpass the patency of bypasses with prosthetic material (57% after 2 years and 37% after 5 years10–12).
The objective of our study was to assess femoro-popliteal lesions. The majority of these patients presented associated distal lesions, which are reflected in the run-off parameter. The femoro-popliteal sector was treated initially in the hopes of improving the ischemia classification. However, in some cases the concomitance of more distal lesions required later distal reinterventions, reconversions to open surgery or, in the worst of cases, major amputation when revascularization was not possible.
In spite of the limitations inherent to retrospective studies with a limited number of cases (in which associations can be inferred, but causality cannot), our results confirm the importance of providing the necessary length of stent coverage in the endovascular treatment of the femoro-popliteal region due to critical ischemia. Patients with femoro-popliteal lesions greater than 20cm with acceptable surgical risk and an available vein should preferably be treated with bypass, and the endovascular option should be used as a last resort.
Conflicts of interestNone.
Please cite this article as: Velescu A, Mateos Torres E, Clará Velasco A. Factores predictores de permeabilidad a medio plazo en el stenting primario del sector femoro-poplíteo en pacientes con isquemia crítica. Cir Esp. 2015;93:105–109.
Content from this article was presented at the 58th Congress of the Spanish Society of Angiology and Vascular Surgery in Barcelona, 31 May–2 June, 2012.