This study sought to evaluate the natural history of patients undergoing below-knee amputation (BKA) and compare their evolution over 2 decades, as well as survival predictors, prosthetic fitting, and contralateral amputation.
MethodsRetrospective study of 209 consecutive patients (mean age 72.9 years; 68% males) who underwent BKA in 2 periods: 1996–2005 and 2006–2015. The fitting of prostheses, risk of contralateral amputation and survival, as well as their predictive factors, were assessed by survival analysis.
Results133 BKA were performed from 1996 to 2005 and 106 from 2006 to 2015. The etiology that motivated the BKA was acute ischemia (4.3%), chronic ischemia (34.0%), infection (9.1%) or mixed (chronic+infection, 52.6%), with no differences found between periods. Survival: mortality within one month=9.2%, one year=31.9%, 2 years=43.8% and 5 years=63.9%, with no significant differences between the 2 periods. Prosthetic: the fitting rate was 44.5% throughout the follow-up, with no significant differences between the two periods. 41.1% patients managed to walk. Contralateral amputation: 20.1% of the patients later required a major contralateral amputation, with no significant differences between the two periods.
ConclusionsIn the last decade, fewer BKA have been performed probably, due to higher previous interventional revascularization. Despite this, the results of fitting, contralateral amputation or survival was not modified. In any case, the number of patients who are able to achieve ambulation is modest, so it emphasizes the need for an optimal selection of patients with BKA with the goal of prosthetic fitting.
El objetivo de este estudio es conocer la historia natural de los pacientes sometidos a una amputación infracondílea (AIC) y comparar su evolución a lo largo de 2 décadas, así como los factores predictores de supervivencia, protetización, y amputación contralateral.
MétodosEstudio retrospectivo de 209 pacientes consecutivos (edad media 72,9 años, varones 67,9%) sometidos a AIC a lo largo de 2 periodos: 1996-2005 y 2006-2015. Se valoró mediante análisis de supervivencia la protetización, el riesgo de amputación contralateral y la supervivencia, así como sus factores predictores.
ResultadosSe realizaron 133 AIC en el 1996-2005 y 106 en el 2006-2015. La etiología global que motivó la AIC fue por isquemia aguda (4,3%), crónica (34%), infección (9,1%) o mixta (crónica+infección, 52,6%), sin diferencias entre periodos. Se incrementaron las revascularizaciones previas entre ambas décadas del 31,6 al 54,3%. Supervivencia: mortalidad a un mes=9,2%; un año=31,9%; 2 años=43,8% y 5 años=63,9%, sin diferencias significativas entre ambos periodos. Protetización: tasa de protetización global del 44,5% durante todo el seguimiento, sin diferencias significativas entre ambos periodos. Lograron deambular el 41,1% de los pacientes. Amputación contralateral: El 20,1% de los pacientes requirieron posteriormente una amputación mayor contralateral, sin hallar diferencias significativas entre ambos periodos.
ConclusionesEn la última década han disminuido las AIC probablemente por un incremento del intervencionismo de revascularización previo. A pesar de ello, no se modificaron los resultados de protetización, amputación contralateral o supervivencia. En cualquier caso, el número de pacientes que llegan a alcanzar la deambulación es modesto, por lo que se subraya la necesidad de una óptima selección del paciente tributario a AIC con el objetivo de protetizarse.
Every year, more than one million people in the world require major limb amputation, which is one amputation every 30s.1 Despite the progress made in prevention, advances made in revascularization for critical lower limb ischemia, and the aggressive medical-surgical approach of diabetic foot sepsis, there is still a percentage of patients who require major lower extremity amputation.
For these patients, the main treatment objective is to achieve the best possible quality of life by preserving independence through the ability to walk.2 Although the benefits and the need to perform a below-knee amputation (BKA) may seem obvious in terms of achieving ambulation and patient autonomy, possible subsequent complications can increase morbidity and mortality.3
With an increasingly aging population and a significant increase in comorbidities, previous studies have indicated that patient characteristics such as age, sex, cognitive status and associated pathologies are related not only to poor functional prognosis, but also to higher mortality after surgery.4,5 Furthermore, amputation of the lower extremities is performed in patients where both lower extremities are at risk, and, to date, the literature on the evolution of the contralateral limb is quite scarce and discouraging.6 Knowing the risk factors associated not only with healing of the stump but also with medium-term patient survival, prosthetic use and evolution of the contralateral limb can be of great importance in the process of indicating BKA and avoiding expectations of unrealistic functional recovery.
The objective of the present study is to analyze the cohort of patients who underwent BKA at our hospital over the last 20 years in order to determine factors associated with prosthetic fitting, survival and contralateral amputation, comparing the results between the 2 decades evaluated.
MethodsWe studied a retrospective cohort of consecutive patients who underwent BKA between January 1996 and December 2015 at a single hospital. They were divided into 2 periods: those carried out from 1996 to 2005 and those performed from 2006 to 2015.
The data were obtained from medical records and telephone contact with patients or their family members. The variables collected included demographic data (age, sex), clinical history (diabetes mellitus, arterial hypertension, ischemic heart disease, previous cerebrovascular accident [CVA], chronic renal failure and hemodialysis), history of amputations and previous revascularization techniques.
We also recorded data on surgical characteristics, immediate complications after the technique and reoperations.
During follow-up, data were collected on patient survival, date of prosthetic fitting (day of admission to the Rehabilitation Service for prosthetic adaptation), as well as the date of ambulation annotated by this department.
Statistical AnalysisThe statistical analysis was conducted with SPSS® version 22 for Windows by IBM®. For the descriptive analysis, the mean and standard deviation were used for the quantitative variables, and frequency and percentages were used for qualitative variables. The comparison between groups was done with Student's t test for quantitative variables and the chi-squared or Fisher's test for qualitative variables. The survival and prosthetic analyses were performed using Kaplan–Meier curves and their comparison using the log-rank test. A multivariate analysis was performed using Cox regression to compare the preoperative variables of patients with survival results, prosthetic fitting and contralateral amputation, expressing the increased risk as a hazard ratio (HR). A P value of less than .05 was considered significant.
ResultsWe performed 239 consecutive BKA in 209 patients: 133 BKA from 1996 to 2005, and 106 BKA from 2006 to 2015. The procedure was bilateral in 30 patients and simultaneous in one case.
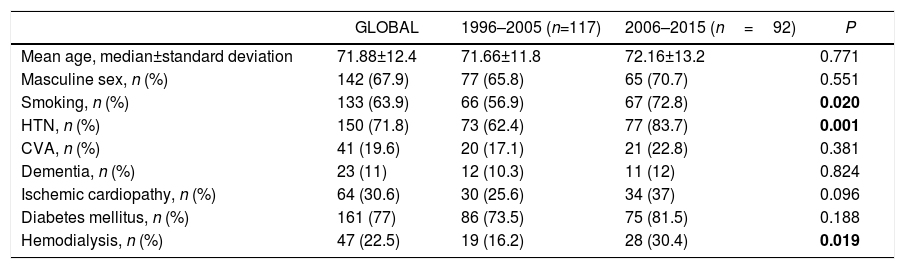
Clinical Characteristics. Mean age was 71.88 years, and 67.9% of patients were males. The clinical characteristics of the operated patients are described in Table 1, while the preoperative characteristics of the limbs treated surgically are shown in Table 2.
Preoperative Clinical Characteristics of the Patients (n=209).
| GLOBAL | 1996–2005 (n=117) | 2006–2015 (n=92) | P | |
|---|---|---|---|---|
| Mean age, median±standard deviation | 71.88±12.4 | 71.66±11.8 | 72.16±13.2 | 0.771 |
| Masculine sex, n (%) | 142 (67.9) | 77 (65.8) | 65 (70.7) | 0.551 |
| Smoking, n (%) | 133 (63.9) | 66 (56.9) | 67 (72.8) | 0.020 |
| HTN, n (%) | 150 (71.8) | 73 (62.4) | 77 (83.7) | 0.001 |
| CVA, n (%) | 41 (19.6) | 20 (17.1) | 21 (22.8) | 0.381 |
| Dementia, n (%) | 23 (11) | 12 (10.3) | 11 (12) | 0.824 |
| Ischemic cardiopathy, n (%) | 64 (30.6) | 30 (25.6) | 34 (37) | 0.096 |
| Diabetes mellitus, n (%) | 161 (77) | 86 (73.5) | 75 (81.5) | 0.188 |
| Hemodialysis, n (%) | 47 (22.5) | 19 (16.2) | 28 (30.4) | 0.019 |
CVA: cerebrovascular accident; HTN: arterial hypertension
Statistically significant results are shown in bold (P<.05).
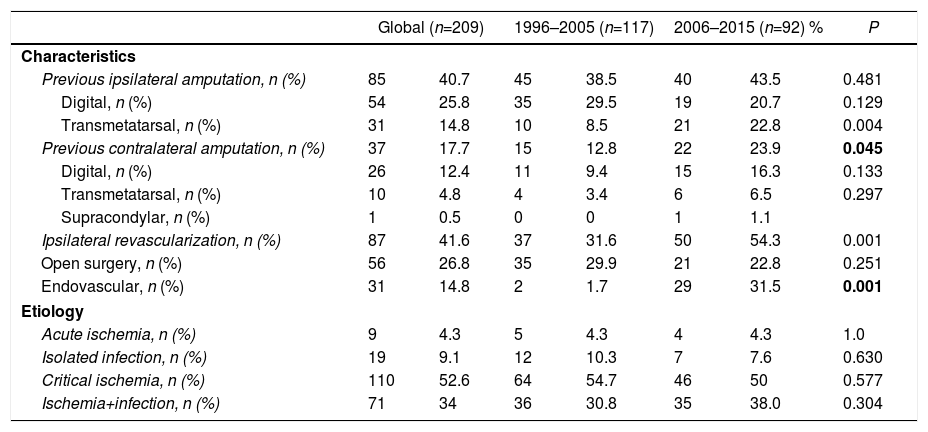
Preoperative Characteristics and Etiology of the lImb Treated.
| Global (n=209) | 1996–2005 (n=117) | 2006–2015 (n=92) % | P | ||||
|---|---|---|---|---|---|---|---|
| Characteristics | |||||||
| Previous ipsilateral amputation, n (%) | 85 | 40.7 | 45 | 38.5 | 40 | 43.5 | 0.481 |
| Digital, n (%) | 54 | 25.8 | 35 | 29.5 | 19 | 20.7 | 0.129 |
| Transmetatarsal, n (%) | 31 | 14.8 | 10 | 8.5 | 21 | 22.8 | 0.004 |
| Previous contralateral amputation, n (%) | 37 | 17.7 | 15 | 12.8 | 22 | 23.9 | 0.045 |
| Digital, n (%) | 26 | 12.4 | 11 | 9.4 | 15 | 16.3 | 0.133 |
| Transmetatarsal, n (%) | 10 | 4.8 | 4 | 3.4 | 6 | 6.5 | 0.297 |
| Supracondylar, n (%) | 1 | 0.5 | 0 | 0 | 1 | 1.1 | |
| Ipsilateral revascularization, n (%) | 87 | 41.6 | 37 | 31.6 | 50 | 54.3 | 0.001 |
| Open surgery, n (%) | 56 | 26.8 | 35 | 29.9 | 21 | 22.8 | 0.251 |
| Endovascular, n (%) | 31 | 14.8 | 2 | 1.7 | 29 | 31.5 | 0.001 |
| Etiology | |||||||
| Acute ischemia, n (%) | 9 | 4.3 | 5 | 4.3 | 4 | 4.3 | 1.0 |
| Isolated infection, n (%) | 19 | 9.1 | 12 | 10.3 | 7 | 7.6 | 0.630 |
| Critical ischemia, n (%) | 110 | 52.6 | 64 | 54.7 | 46 | 50 | 0.577 |
| Ischemia+infection, n (%) | 71 | 34 | 36 | 30.8 | 35 | 38.0 | 0.304 |
Statistically significant results are shown in bold (P<.05)
During the second decade of the study, the patients had a higher prevalence of smoking, hypertension, hemodialysis, previous contralateral amputation and previous endovascular revascularization, with no differences between the two groups for open surgery.
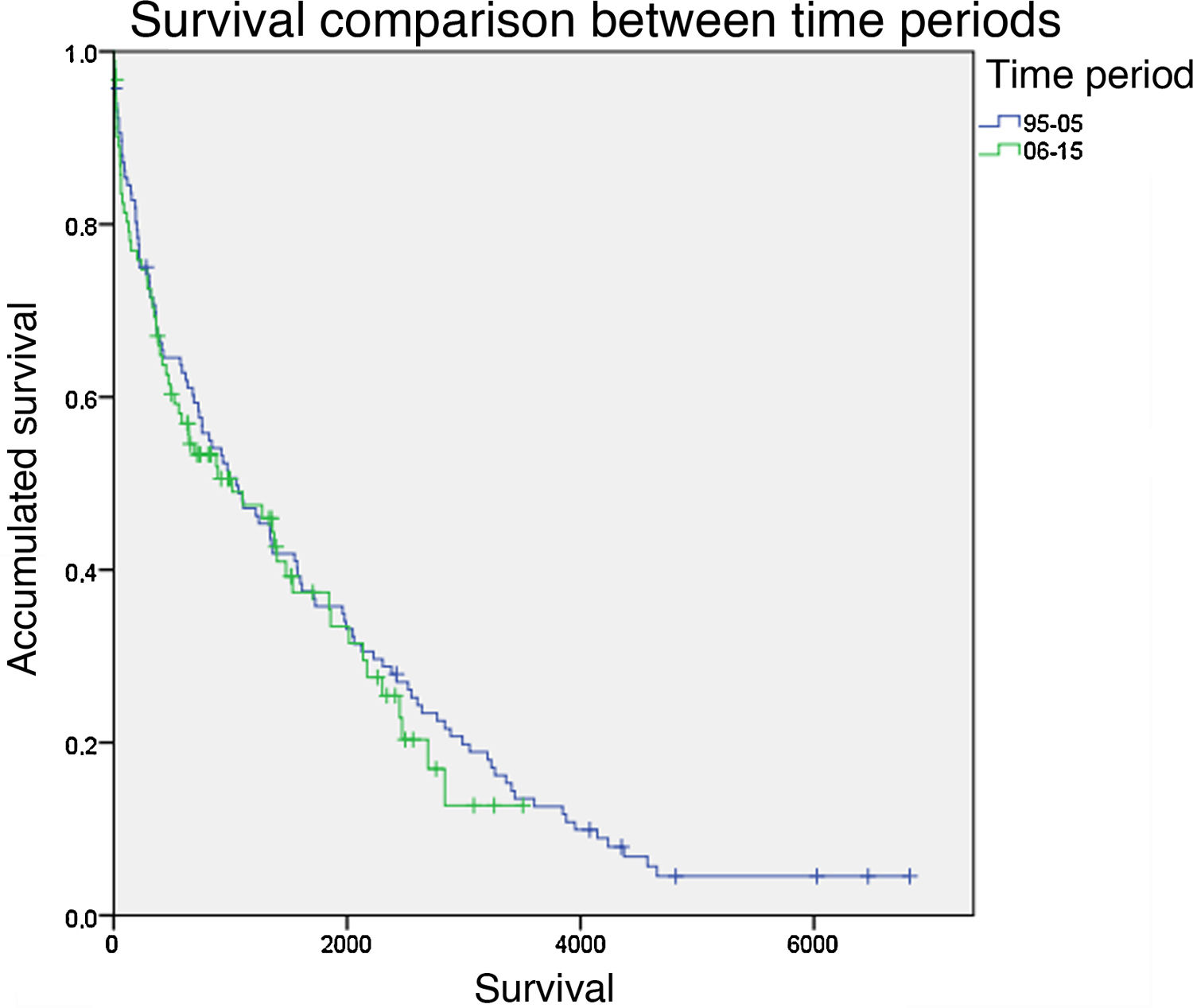
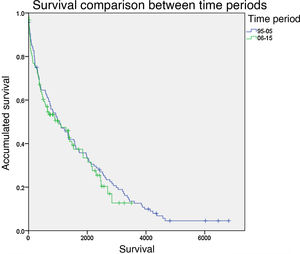
Survival. Immediate mortality during the first month was 9.2%. The one-year survival rate was 68.1%, the 2-year rate was 56.2% and the 5-year rate was 36.1%. No statistically significant differences were observed between the two periods compared (Fig. 1). Protective factors included previous revascularization (HR=0.596; P=.002) and infectious etiology (HR=0.375; P=.002), while increased mortality was associated with dementia (HR=2.441; P<.001), hemodialysis (HR=1.757; P=.003), hypertension (HR=1.585; P=.018) and previous contralateral amputation (HR=1.614; P=.019)
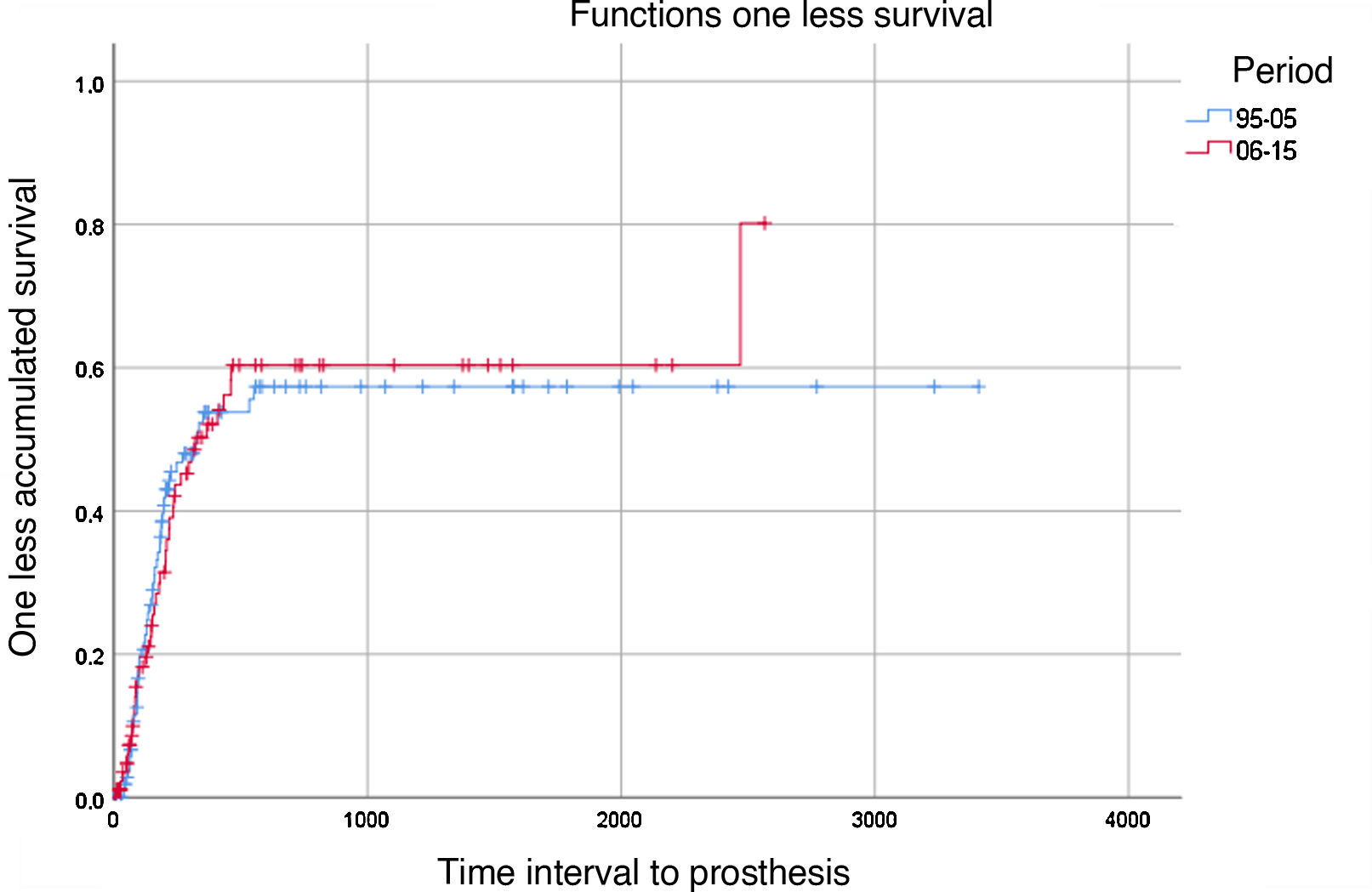
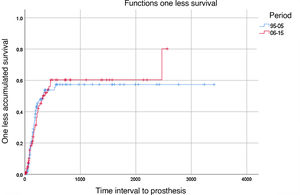
Prostheses. 44.5% of the total number of the patients were fitted with prostheses, and 41.1% of the total were able to complete the rehabilitation process and walk. There were no statistically significant differences between the time periods compared (Fig. 2). Dementia (HR=0.286; P=.033), previous contralateral amputation (HR=0.446; P=.013), previous AVC (HR=0.504; P=.027) and female sex (HR=0.521; P=.008) were associated with a lower rate of prosthetic use.
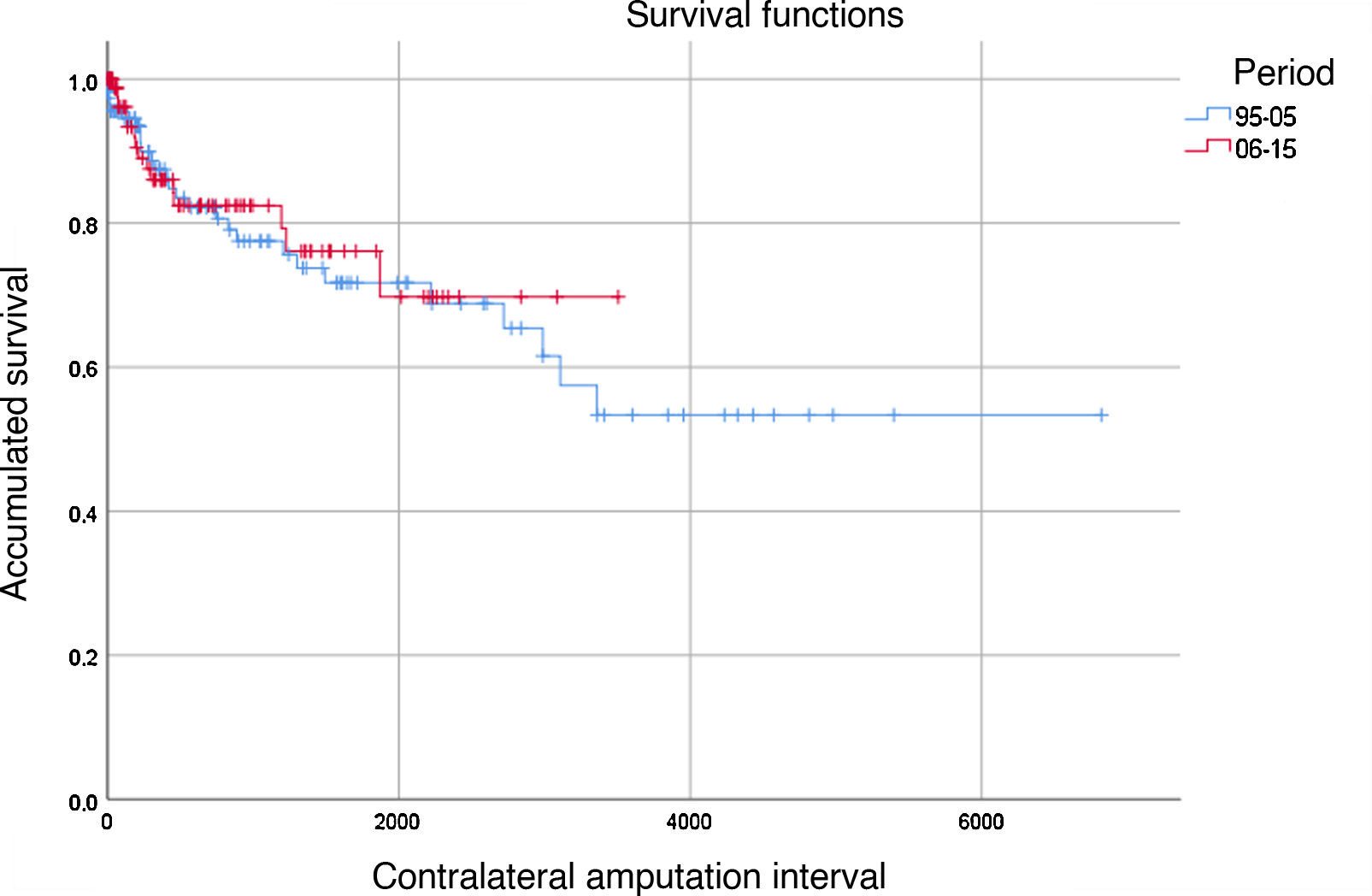
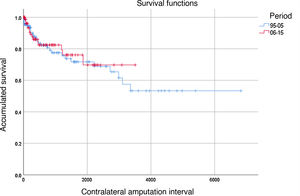
Contralateral Amputation. Out of the total of 209 operated patients, 42 required major amputation of the contralateral lower extremity during follow-up, representing 20.1% of the total (30 BKA and 12 supracondylar amputations). The ‘absence of amputation’ rates of the contralateral limb were 88%, 82% and 72% after one, 2 and 5 years in the period 1996-2005 and 86%, 82% and 76% in the period 2006–2015, respectively; no statistically significant differences were observed between the two periods (Fig. 3). Risk factors associated with contralateral major amputation included hemodialysis (HR=3.548; P<.001), previous AVC (HR=2.526; P=.007) and dementia, which was marginally significant (HR=2.630; P=.052).
DiscussionThis study analyzes the clinical characteristics and functional results of patients who underwent BKA over a period of 2 decades. Since BKA is usually associated with a more complex postoperative convalescence than above-knee amputation, identifying factors associated with a poor prognosis in terms of survival, prosthetic use, or future need for major contralateral amputation can contribute to better patient selection, thereby avoiding unrealistic rehabilitation expectations.7
By comparing the clinical characteristics of the patients in the 2 decades of study, we observed how comorbidity has generally increased in all the variables studied. Diabetes mellitus is especially relevant (although without reaching statistical significance) due to the etiological implications, as is chronic kidney failure in a hemodialysis program since, in addition to having almost doubled, it has been shown to be a significant prognostic factor for both survival and the risk of contralateral amputation. The high prevalence of comorbidities in these patients is in line with results from previous series3,6,8; the same is true of critical limb ischemia, associated or not with infection, being the main causal factor.5,9
We observed a significant increase in revascularization procedures prior to amputation between the two periods, going from 31.6% to 54.3% of patients. It should be noted that this increase has occurred at the expense of endovascular revascularization techniques, which have gone from being practically anecdotal in the first period to exceeding the number of open surgery procedures in the second. This fact reflects a probable increase in the indications for revascularization in patients with critical ischemia, associated or not with diabetic foot syndrome, and there is currently the possibility to treat patients endovascularly who were not previously candidates for surgery. This increase in surgical interventionism is probably also related to the 22% drop between the 2 decades of the number of patients who have required BKA as the end-point of their process. The increase in previous ipsilateral transmetatarsal amputations between periods was also significant. We believe that this could also be indicative that there are currently more possibilities of revascularization and of being able to subsequently carry out less aggressive amputation options.
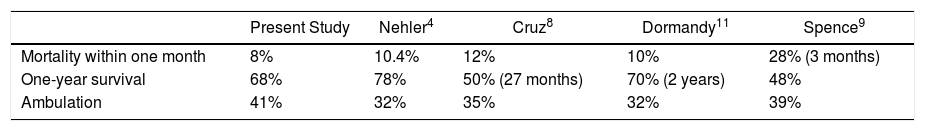
Analyzing survival, we observed how short- and mid-term life expectancies were low, and just over one-third of patients were alive after 5 years. Furthermore, despite having rehabilitation programs, slightly more than 40% of the patients managed to walk with their prosthesis. These data only emphasize the palliative nature of this type of procedure, which is also related to the significant comorbidity that this population presents. Although these data may seem dismal, they are in line with other reports published to date (Table 3) both in terms of mortality rate and ambulation.
Classically, it has been considered that, in patients candidates for major amputation of a limb, it is important to preserve the knee due to the lower energy expenditure associated with the use of a prosthesis after BKA compared to above-knee amputation,10 resulting in a higher usage rate of prostheses.5,6 Therefore, the main objective of performing BKA is for the patient to achieve independent mobility. However, as demonstrated in this study and in the previous publications, less than half of patients achieve mobility with prostheses. Additionally, in many cases, the palliative tendency of this type of amputation is also evident given the high immediate postoperative and one-year postoperative mortality rates. Therefore, preoperative criteria are necessary to help identify patients with the worst prognosis, in whom the final outcome of prosthetic use is unattainable; for these individuals, it might be advisable to propose more palliative approaches from the outset. For instance, above-knee amputation may be a less complex alternative with lower postoperative morbidity that should be considered.3,8 Due to the limitations of our study, it would be risky and unreliable to try to establish a score to discriminate these cases. But it does indicate factors for poor vital and functional prognosis, such as hemodialysis, dementia, contralateral amputation, or a history of CVA. These elements can assist the clinician and patients while making a therapeutic decision in the critical situation of an amputation.
On the other hand, BKA is often performed in patients with both limbs at risk, either due to critical limb ischemia or diabetes. The high rate of hemodialysis patients requiring major contralateral amputation is discussed by Glaser et al.,6 reporting 11.5% within 5 years of the initial major amputation.
The main limitations of the present study are its retrospective, single-center nature and the limited patient sample. Although it provides an overall idea of how the history of amputee patients has evolved and the potential influencing factors, new studies would be required to reliably propose prognostic tests or scores.
Although the number of BKA has decreased over the last decade, probably due to the advent of endovascular revascularization techniques, patients who continue to require this procedure show a poor functional and/or survival prognosis in the medium term, which has remained unchanged in the last 10–20 years. Certain factors associated with poor vital or functional prognosis may help reassess the indication for surgery in some of these patients. Hence, this would identify patients who would benefit from BKA with acceptable rehabilitation results, while also identifying patients who would benefit from a more palliative type of amputation.
FundingThis study has received no specific funding from public, commercial or non-profit organizations.
Conflict of InterestsNone.
Please cite this article as: Marcos García L, Mateos Torres E, Velescu A, Díaz Duran C, Lacambra Peñart M, Clará Velasco A. Historia natural del paciente sometido a una amputación infracondílea: análisis de la supervivencia y protetización durante 2 décadas. Cir Esp. 2020;98:403–408.