The use of autoadhesive meshes with hooks that allow fixation without sutures is a therapeutic alternative to decrease recurrence and chronic pain after inguinal hernia repair. The aim of this study was to evaluate if this kind of mesh has any advantage in long term results in comparison with the classic Lichtenstein technique with sutures and polypropylene mesh.
Materials and methodsWe report a prospective and randomized study of patients who have been operated on for inguinal hernia between March of 2009 to March 2010, divided into 2 groups of 45 patients. In autoadhesive (AA) group, we included patients operated on with an autoadhesive mesh and in classic Lichtenstein (CL) group we included cases with an inguinal hernioplasty with sutured polypropylene mesh. We evaluated time of inactivity, complications, recurrences and grade of pain after 1 year.
ResultsThe mean age was 60 years in AA group and 49 in LC group. There were more men than women and there were no differences in co-morbidities between groups. The mean size of hernia orifice was 3cm in both groups and 60% of the hernias were indirect.
After 1 year, 77 patients were evaluated, 39 in LC group and 38 in AA group. 86.8% and 87.2% of them were asymptomatic. The mean time of recovery of daily activities was 15 days in both groups. There were neither recurrences nor severe chronic pain in the AA group. The mean of grade of pain was 0 (range: 0–4) in AA group and 0 (range: 0–5) in LC group. In this group, there was one recurrence and one patient was taking analgesics for intense pain. Neither mortality nor other long term complications were found.
ConclusionThe use of autoadhesive and parcial reabsorbible meshes in inguinal hernia repair has no effect on recovery of daily activities, postoperative pain and long term complications compared with hernioplasty with polypropylene mesh fixed with monofilament suture.
Las mallas autoadhesivas se plantean como una alternativa para disminuir el dolor crónico y las recidivas en la hernioplastia inguinal. Pretendemos determinar si el empleo de estas mallas representa algún beneficio en el resultado a largo plazo en comparación con la técnica clásica de Lichtenstein fijando la malla con suturas.
Material y métodosEstudio prospectivo y aleatorizado de pacientes intervenidos de hernia inguinal entre marzo de 2009 y marzo del 2010, incluyendo en el grupo autoadhesivo (AA) 45 individuos en los que se realizó la hernioplastia con malla autoadhesiva y en el grupo Lichtenstein clásico (LC) otros 45 utilizando una malla de polipropileno fijada con sutura monofilar. Se evaluaron tiempo de inactividad, posibles complicaciones, recidivas y grado de dolor al año de la intervención.
ResultadosLa edad media del grupo AA fue de 60 años frente a los 49 del grupo LC. En ambos, la mayor parte eran varones sin diferencias en las comorbilidades asociadas, siendo el tamaño medio del defecto herniario de 3cm; en torno al 60% de las hernias eran indirectas. Al año de la intervención, 39 pacientes fueron evaluados en el grupo LC y 38 en el AA. La mediana del tiempo de recuperación de la actividad diaria normal fue de 15 días en ambos grupos. En el grupo AA, el 86,8% estaban asintomáticos, ninguno presentó recidiva herniaria ni precisó tomar analgésicos de forma continua, siendo la mediana del grado de dolor de 0. En el grupo LC, el 87,2% permanecían asintomáticos, un paciente (2,6%) presentó una recidiva y un paciente (2,6%) requería la toma continua de analgésicos por dolor intenso, siendo la mediana de dolor de 0. No hubo mortalidad ni otras complicaciones a largo plazo.
ConclusiónEl empleo de mallas autoadhesivas y parcialmente reabsorbibles en la reparación de la hernia inguinal no presenta diferencias significativas en recuperación, dolor ni complicaciones postoperatorias a largo plazo frente a la hernioplastia con malla de polipropileno fijada con sutura monofilar.
Inguinal hernia disease is one of the surgical entities with the greatest incidence at present, representing a large number of surgical interventions and high healthcare costs. Advances made both in prosthetic material as well as different wall reconstruction techniques strive to improve post-operative well-being and diminish the number of long-term recurrences and neuralgias due to the technique. The use of self-adhesive mesh is an example of these advances as they avoid using sutures, which supposedly cause the chronic pain1 associated with inguinal hernioplasty procedures. In a previous study by our group published in this journal,2 we presented the short-term results of a technique using this type of mesh with shorter intraoperative placement time of the prosthesis and total surgical time compared with the conventional technique.
As a continuation of that paper, we present this new study, with the aim to determine whether the use of self-adhesive and partially absorbable mesh would be more beneficial in inguinal hernia repair using the Lichtenstein technique compared with traditionally used mesh that are attached with monofilament sutures with regard to the results for inactive time/sick leave, pain and long-term complications.
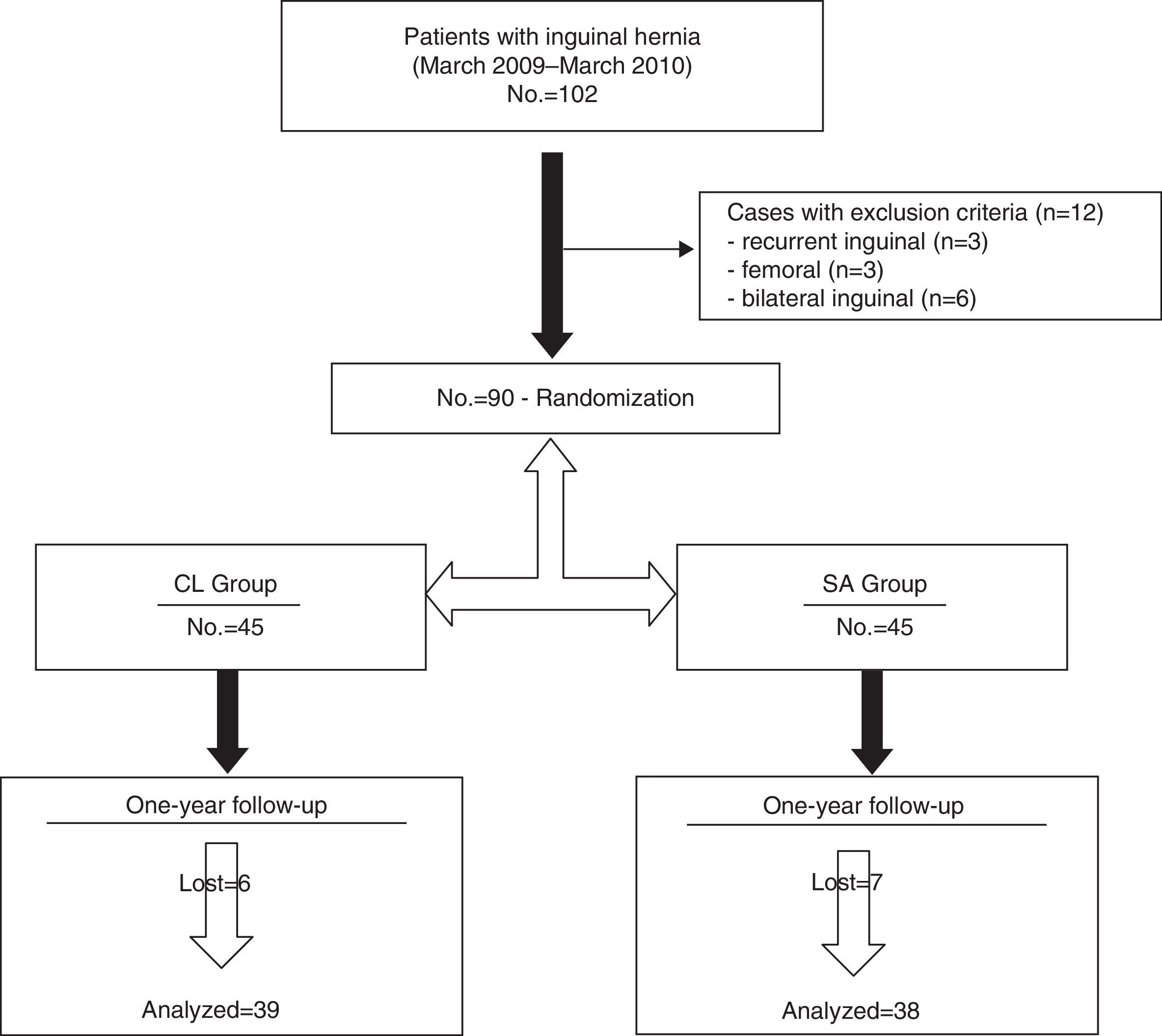
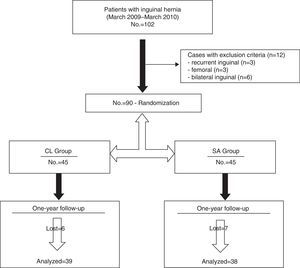
Materials and MethodsWe have carried out a prospective, randomized and comparative study of patients who underwent inguinal hernia repair performed by our team between March 2009 and March 2010 (Fig. 1).
The patients were randomly divided into 2 groups of 45 individuals each by drawing a paper out of a bag that had either “SA” (self-adhesive) or “CL” (classic Lichtenstein) written on it just moments before surgery.2 Patients in group SA underwent inguinal hernia repair with a preformed self-adhesive polypropylene and polylactic acid mesh (Parietene Progrip™ Self-Fixating mesh by Covidien®), while patients in group CL underwent Lichtenstein hernioplasty with low-density polypropylene mesh (Microval®) that was attached with non-absorbable monofilament sutures. Excluded from the study were those patients with recurring, bilateral or femoral hernias and those who underwent emergency hernia repair (Fig. 1).
In the preoperative study, we collected different epidemiologic variables and comorbidities, while cataloging the anatomical type of hernia according to the Gilbert classification. In all cases, the same antibiotic prophylaxis was administered: preoperatively, 30min before the skin incision (750mg intravenous cefuroxime and, in patients with allergies, 200mg intravenous ciprofloxacin) and all the patients were operated on under intradural anesthesia without infiltrating the surgical wound in any of the cases with local anesthesia.
Both the patients in group SA and those from group CL were operated on by the same surgeon and surgical team with experience in abdominal wall surgery. In both groups, the same operative steps were followed and the only technical difference was the mesh fixation method. In the case of group SA patients, the mesh was placed on the posterior wall of the inguinal canal, surpassing the pubic symphysis and reaching the iliopubic tract with no sutures. Meanwhile, in group CL, mesh fixation involved a continuous suture of monofilament 3/0 to the inguinal ligament and interrupted stitches to the tendon, in accordance with the technique described by Lichtenstein.3 In both groups, if there was evidence of weakness of the posterior wall of the inguinal canal or direct hernia, a continuous suture with monofilament 3/0 was used for the repair. The nerve fibers that had been identified were preserved and manipulated as little as possible during the intervention, although we did not systematically search for or identify them. In cases in which the mesh was fixed with sutures, we did take special care that none of these stitches encompassed nerve branches in the area.2
Postoperative analgesia was the same in both groups (paracetamol and ibuprofen, using tramadol as rescue analgesia) and patients were discharged after starting to walk, when oral intake was tolerated and no complications were observed.2
We evaluated sick leave (or time until normal daily activities were resumed in non-employed patients), possible complications and degree of pain using the visual analog scale (VAS),2 with physical exploration and personal interview 1 year after surgery. The statistical analysis was done with the SPSS 17.0 program for Windows, considering a P value less than .05 statistically significant. The Chi-squared test was used to compare the qualitative variables and the Mann–Whitney U was used for the quantitative variables.
ResultsA total of 90 patients were included in this study, and each of the two study groups had 45 individuals (Fig. 1).
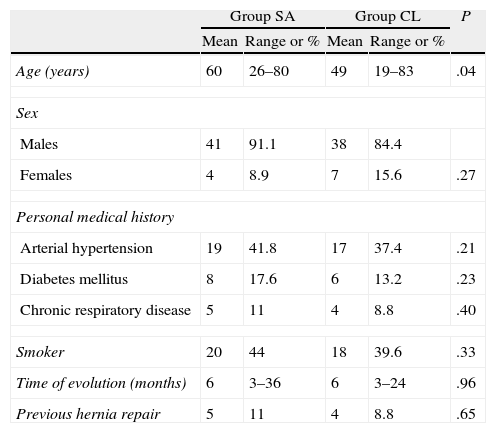
The mean age of group SA was 60 (range: 26–80) versus 49 (range: 19–83) in the CL group. In both, the majority of the patients were male (91 and 84.4%, respectively), with no significant differences in the associated comorbidities between the groups (Table 1). In group SA, 44% were smokers and 39.6% were in group CL (Table 1).
Characteristics of the Patients Included in Each Group.
| Group SA | Group CL | P | |||
| Mean | Range or % | Mean | Range or % | ||
| Age (years) | 60 | 26–80 | 49 | 19–83 | .04 |
| Sex | |||||
| Males | 41 | 91.1 | 38 | 84.4 | |
| Females | 4 | 8.9 | 7 | 15.6 | .27 |
| Personal medical history | |||||
| Arterial hypertension | 19 | 41.8 | 17 | 37.4 | .21 |
| Diabetes mellitus | 8 | 17.6 | 6 | 13.2 | .23 |
| Chronic respiratory disease | 5 | 11 | 4 | 8.8 | .40 |
| Smoker | 20 | 44 | 18 | 39.6 | .33 |
| Time of evolution (months) | 6 | 3–36 | 6 | 3–24 | .96 |
| Previous hernia repair | 5 | 11 | 4 | 8.8 | .65 |
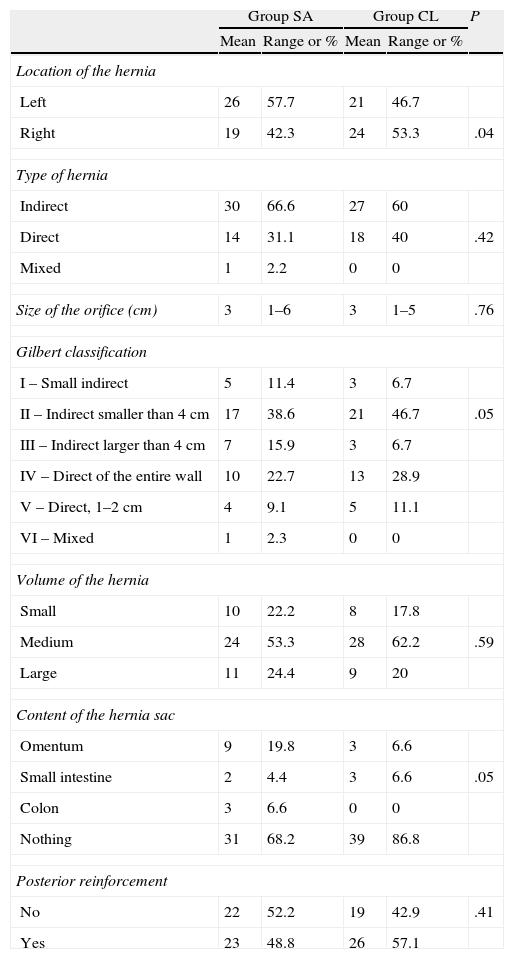
The average time of evolution of the hernia was 6 months in the 2 groups. Hernias on the left side were more frequent in group SA (57.7%), while right side hernias were more prevalent in the CL group (53.3%) (Table 2). In both groups, the average size of the hernia defect was 3cm in diameter. Indirect hernias were shown by 66.6% of the patients in group SA and 60% of CL. As for the anatomic type of the hernia in accordance with the Gilbert classification, types II and IV were the most prevalent in both groups (Table 2). The posterior wall was reinforced with a suture of 3/0 monofilament in 52.2% and 57.1% of the patients of groups SA and CL, respectively (Table 2).
Characteristics of the Hernias and Intraoperative Findings.
| Group SA | Group CL | P | |||
| Mean | Range or % | Mean | Range or % | ||
| Location of the hernia | |||||
| Left | 26 | 57.7 | 21 | 46.7 | |
| Right | 19 | 42.3 | 24 | 53.3 | .04 |
| Type of hernia | |||||
| Indirect | 30 | 66.6 | 27 | 60 | |
| Direct | 14 | 31.1 | 18 | 40 | .42 |
| Mixed | 1 | 2.2 | 0 | 0 | |
| Size of the orifice (cm) | 3 | 1–6 | 3 | 1–5 | .76 |
| Gilbert classification | |||||
| I – Small indirect | 5 | 11.4 | 3 | 6.7 | |
| II – Indirect smaller than 4cm | 17 | 38.6 | 21 | 46.7 | .05 |
| III – Indirect larger than 4cm | 7 | 15.9 | 3 | 6.7 | |
| IV – Direct of the entire wall | 10 | 22.7 | 13 | 28.9 | |
| V – Direct, 1–2cm | 4 | 9.1 | 5 | 11.1 | |
| VI – Mixed | 1 | 2.3 | 0 | 0 | |
| Volume of the hernia | |||||
| Small | 10 | 22.2 | 8 | 17.8 | |
| Medium | 24 | 53.3 | 28 | 62.2 | .59 |
| Large | 11 | 24.4 | 9 | 20 | |
| Content of the hernia sac | |||||
| Omentum | 9 | 19.8 | 3 | 6.6 | |
| Small intestine | 2 | 4.4 | 3 | 6.6 | .05 |
| Colon | 3 | 6.6 | 0 | 0 | |
| Nothing | 31 | 68.2 | 39 | 86.8 | |
| Posterior reinforcement | |||||
| No | 22 | 52.2 | 19 | 42.9 | .41 |
| Yes | 23 | 48.8 | 26 | 57.1 | |
The intra- and postoperative complication rates were analyzed in our previous study, with no differences shown between the techniques.2 The average hospital stay was 15h in both groups, with no significant differences between them (P=.85).
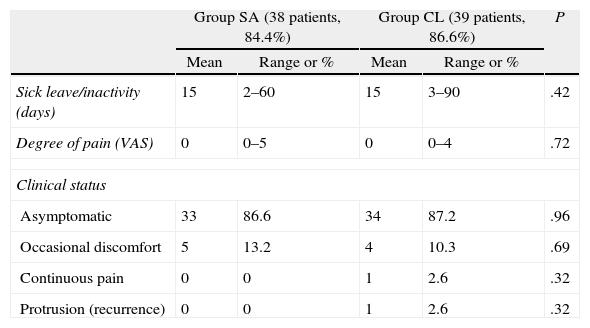
One year after the procedure, a total of 77 patients were evaluated and monitored: 39 in the CL group (86.6%) and 38 in the SA group (84.4%) (Fig. 1). The mean sick leave or time transpired until returning to normal daily activity in non-employed patients or retirees was 15 days in both groups (P=.42) (Table 3).
Sick Leave/Inactivity and Clinical Follow-Up 1 Year After Hernioplasty.
| Group SA (38 patients, 84.4%) | Group CL (39 patients, 86.6%) | P | |||
| Mean | Range or % | Mean | Range or % | ||
| Sick leave/inactivity (days) | 15 | 2–60 | 15 | 3–90 | .42 |
| Degree of pain (VAS) | 0 | 0–5 | 0 | 0–4 | .72 |
| Clinical status | |||||
| Asymptomatic | 33 | 86.6 | 34 | 87.2 | .96 |
| Occasional discomfort | 5 | 13.2 | 4 | 10.3 | .69 |
| Continuous pain | 0 | 0 | 1 | 2.6 | .32 |
| Protrusion (recurrence) | 0 | 0 | 1 | 2.6 | .32 |
86.8% of the patients from group SA and 87.2% of those from group CL remained asymptomatic 1 year after surgery. Out of the 38 patients followed up in group SA, 5 (13.2%) reported having occasional mild discomfort and none presented hernia recurrence nor needed continuous analgesia, and the average degree of pain in this group was 0 (range: 0–4) (Table 3). Out of the 39 patients followed-up in the CL group, only one patient (2.6%) presented hernia recurrence, and the average pain score as evaluated by the VAS was 0 (range: 0–5). Three patients (7.6%) reported occasional mild pain and one patient (2.6%) complained of more intense pain that required continuous analgesia (Table 3). There was no mortality or any other type of complications in the patients examined 1 year after the intervention.
DiscussionChronic pain and hernia recurrence are the complications that are of greatest concern in the long-term after inguinal hernioplasty. In order to try to prevent them or reduce their incidence, different techniques and materials have been developed.
Chronic pain rates are variable, reaching percentages of more than 50%. The pain can be so incapacitating that patients cannot perform daily activities in up to 10% of cases, according to some Danish and Canadian studies.4,5 These numbers are higher than those reported in more recent studies6 and in those of our group.
There are contradictory data in the literature about which surgical approach should be performed with the nerve branches in the inguinal region during hernia repair in order to reduce both immediate and chronic pain associated with the technique. A recent meta-analysis shows that the preservation of the ilioinguinal nerve reduces the incidence of the loss of sensitivity in the inguinal area, but it does not lead to a reduction in chronic pain or in local numbness when compared with their resection.7 While some authors defend the identification of the different nerves and their preservation,8 others advocate their resection to reduce the degree of chronic pain associated with these procedures.9 We are in favor of preserving the identified nerve fibers and manipulating them as little as possible during the intervention, but we do not systematically search for or identify them, although we do take special care that none of our stitches encompass any nerve branches in the area when attaching the mesh with sutures.
With the aim to reduce the cases of neuralgia, new methods of mesh fixation have been developed that try to avoid the use of conventional sutures, such as surgical glues and self-adhesive mesh like those used in our study. In some studies, more pain and more sensation of foreign body have been shown 1 year after the intervention in patients where the mesh was attached with monofilament sutures when compared with the group where surgical glue was used instead.10 Self-adhesive mesh is made of polypropylene and polylactic acid and does not require sutures to the pubis, inguinal ligament or posterior wall thanks to the absorbable microhooks that hold it to the tissue it is contact with. This represents another alternative that could supposedly reduce postoperative pain11 without increasing the number of complications or relapses, as some series argue.12 In our study, however, we have seen no evidence of significant differences in long-term pain or in recurrences between the two patient groups.
In a study previously published by our group, the overall surgical time and self-adhesive mesh placement time were significantly shorter compared with the group where the conventional polypropylene mesh was attached with monofilament suture, with no significant difference in hospital stay, complications or pain during the early post-op period of the patients in both groups.2
Since the appearance of prosthetic materials for inguinal hernia surgery, recurrence rates have been dropping to the current rate of 2% in the long term, according to the international literature.13 Furthermore, most of these recurrences occurred within the first 2 years after surgery.14,15 In our series, only one patient presented recurrence 1 year after the intervention and, although we consider that the number of patients is not sufficient to be able to establish a solid conclusion, other multicenter series have also reported that the recurrence percentage with this type of self-adhesive mesh is low.16
The period of convalescence after surgery is variable and difficult to evaluate in the medical literature due to the variability of study concepts and designs. In general, there is no consensus that longer periods of inactivity reduce the risk of recurrence, so it is usually recommended that patients return to their daily activities as soon as possible.17 In our case, the patients recovered normal activity about 15 days after surgery, depending on their clinical condition and occupation, with no predetermined schedule. In other studies, the average recovery time before returning to domestic activities after hernia repair surgery is 7 days and 21 days before going back to work.17
Self-adhesive mesh is more expensive than the polypropylene mesh that is conventionally used,2 and no significant differences were observed in our study regarding recovery time, pain or recurrences. Thus, any possible benefit of the use of this type of mesh comes down to merely the reduction in surgical time and the ease with which the prosthesis is implanted. Therefore, we conclude, based on the results of our study, that the use of self-adhesive mesh in inguinal hernioplasty using the Lichtenstein technique is a safe method in the long term. Prospective studies with larger patient groups are needed to clarify its possible advantages over the use of polypropylene mesh with monofilament suture fixation.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bruna Esteban M, Cantos Pallarés M, Artigues Sánchez de Rojas E, Vila MJ. Estudio prospectivo y aleatorizado de los resultados a largo plazo de la hernioplastia inguinal con malla autoadhesiva frente a la técnica convencional con malla de polipropileno y sutura de fijación. Cir Esp. 2014;92:195–200.