Peliosis hepatis (PH) is an uncommon condition characterized by the presence of multiple cavities or blood-filled pseudocysts with varying morphology and size. Its clinical presentation ranges from the absence of symptoms to serious complications (hepatic failure, portal hypertension, cholestasis, and intraperitoneal hemorrhage due to liver rupture). We do not know the exact incidence of liver rupture secondary to PH, but in the literature only 20 cases have been published.1 We present a case of hemoperitoneum due to spontaneous liver rupture secondary to PH.
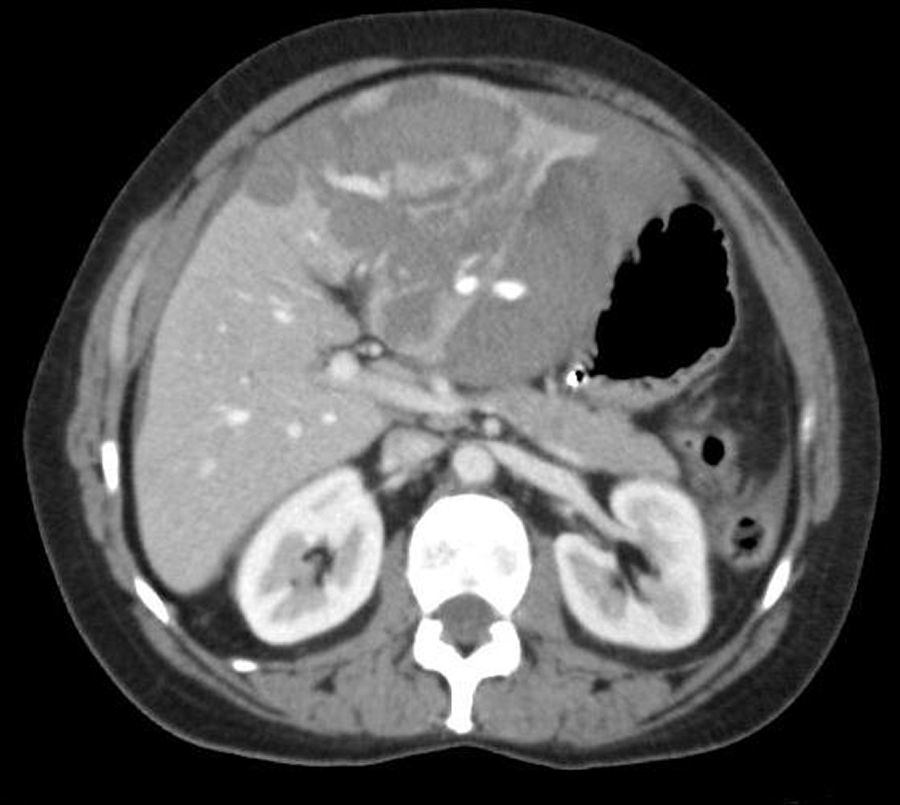
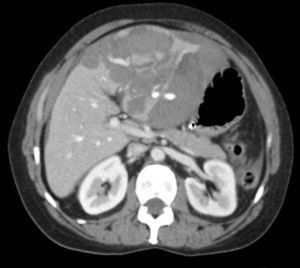
We present the case of a 52-year-old woman who came to our Emergency Department due to sudden-onset abdominal pain in the epigastrium 4h before. Her personal history included COPD and treatment with oral contraception. Physical examination showed peritoneal irritation in the epigastric area. Lab work revealed leukocytosis with neutrophilia, hemoglobin 12.8g/dl, normal coagulation times and a pattern of cholestasis. Abdominal CT scan (Fig. 1) demonstrated a round mass that occupied practically the entire left lateral section of the liver that was predominantly subcapsular and approximately 10cm in diameter, with hypo- and isodense areas, poorly defined, with inner vascular structures and areas of probable bleeding. Abundant free abdominal fluid was observed, which was predominantly perihepatic.
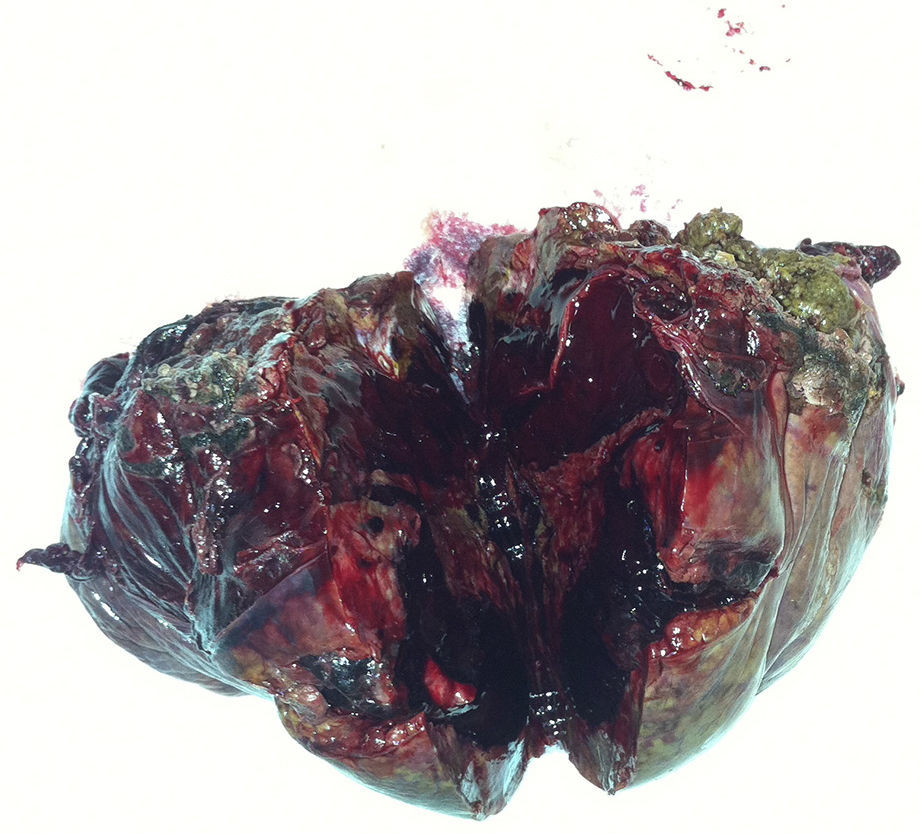
Given these findings, an urgent laparotomy was performed. The intraoperative findings included: hemoperitoneum of 2L secondary to a ruptured subcapsular hepatic mass located in segments ii–iii. A left lateral segmentectomy was performed (Fig. 2). The immediate postoperative period transpired with no complications and the patient was discharged from the hospital on the 8th day post-op. The pathology study of the surgical specimen reported it to be PH.
Peliosis is a rare pathology, with a prevalence of 0.13%. It mainly affects organs of the reticuloendothelial system (liver, spleen, bone marrow, and lymph nodes). Although it has been described in children,2 it usually affects patients in the fifth or sixth decades of life, with no clear predilection for either sex.3 It has been seen in association with the use of certain drugs (mainly anabolic steroids and oral contraceptives), tuberculosis, hematologic diseases, and neoplasms.4 Cases of PH have been described in HIV-positive patients,5 and it has been proposed that the virus may have a cytopathic effect on the sinusoidal endothelial cells. There have been reports of spontaneous regression of the disease after the suppression of steroids or after treatment of the associated infectious disease.5,6
The exact pathogenesis of PH is unknown. It is characterized by the presentation of cystic spaces full of blood that can be between a few millimeters and several centimeters in size, with no preferred intrahepatic location. Yanoff et al. described 2 morphologic PH patterns: parenchymal and phlebectatic.7 In the parenchymal form, the blood-filled space is outlined by hepatocytes and is associated with hemorrhagic necrosis of the parenchyma. In the phlebectatic type, the blood-filled space is outlined by endothelium, with aneurysmal dilatation of the central vessel. However, other authors postulate that there is only one morphologic PH pattern that initiates with focal necrosis of the parenchyma, transforming into a hemorrhagic area (parenchymal pattern) that can progress toward fibrosis and an endothelial covering (phlebectatic pattern) or toward healing with the formation of fibrin, thrombosis, and sclerosis of vascular spaces.8
The clinical presentation is variable and may be asymptomatic with focal liver lesions diagnosed as a finding on radiological testing. Or, it may debut as hepatomegaly or liver dysfunction and, less frequently, it can present complications such as liver failure, cholestasis, portal hypertension or hemoperitoneum secondary to spontaneous rupture. The natural evolution of PH is unknown; the lesions may resolve spontaneously or lead to serious complications.9
Computed tomography with contrast demonstrated the PH lesions as heterogenous and hypodense areas compared with the normal parenchyma. In the arterial phase, there may be non-perfused areas with vasodilation and large lesions that present a center with contrast uptake. In the portal phase, they present centrifugal progression with accumulation of the contrast in these areas in the late phase, becoming isodense as the evaluation progresses. These lesions do not exert a mass effect, which differentiates them from metastatic or tumor lesions. Subcapsular hematomas may also be observed in different stages of evolution and, in those cases with active bleeding, extravasation of the contrast may be seen.5 The differential diagnosis should be done mainly with adenoma, hemangioma, nodular hyperplasia, and hypervascular metastases.5
On MRI, multiple foci have been documented with increased signal in the T2-weighted sequences and a variable signal in the T1 sequences, which presumably reflect different stages of the hemorrhage. It is also possible for the MRI to be normal in cases of uncomplicated peliosis.10
The treatment of PH varies depending on the triggering cause. Regression of the disease has been described after the related drug use has stopped or after the treatment of associated diseases.2,8 Our case could be associated with the prolonged use of oral contraceptives. In those cases in which PH presents with complications such as intraabdominal bleeding, the treatment is liver resection. Early diagnosis of PH and the appropriate etiologic treatment can avoid possible complications.
In conclusion, PH is a rare condition that should be considered in the differential diagnosis of liver lesions and in the acute presentation of intraabdominal hemorrhage.
Please cite this article as: Veguillas Redondo P, Ramia Angel JM, Kuhnhart Barrantes A, Cobos Mateos JM, Garcia-Parreño J. Rotura hepática secundaria a peliosis hepática. Cir Esp. 2014;92:499–501.