Trauma remains the leading cause of mortality and morbidity in people under 40 years of age. Occupational accidents are responsible for a large percentage of these injuries and even deaths. In 2020, occupational accidents were directly affected by the SARS-CoV-2 pandemic, and a total of 505 528 work-related accidents were registered. Construction was the sector with the highest incidence. Fatal accidents accounted for 0.1%.1
Knowledge of the mechanism of injury, intensity, stigmata and associated injuries are essential to suspect the affected organs. Penetrating trauma (PT) includes low-energy (stabbing) and high-energy (projectiles) injuries.2
In the case of metal shards, these usually behave as a high-speed mechanism, similar to a projectile. We present 2 occupational accidents involving metal shards that demonstrate how the initial evaluation has important implications in morbidity and mortality, and how adequate therapeutic diagnostic planning is essential to avoid hidden injuries.
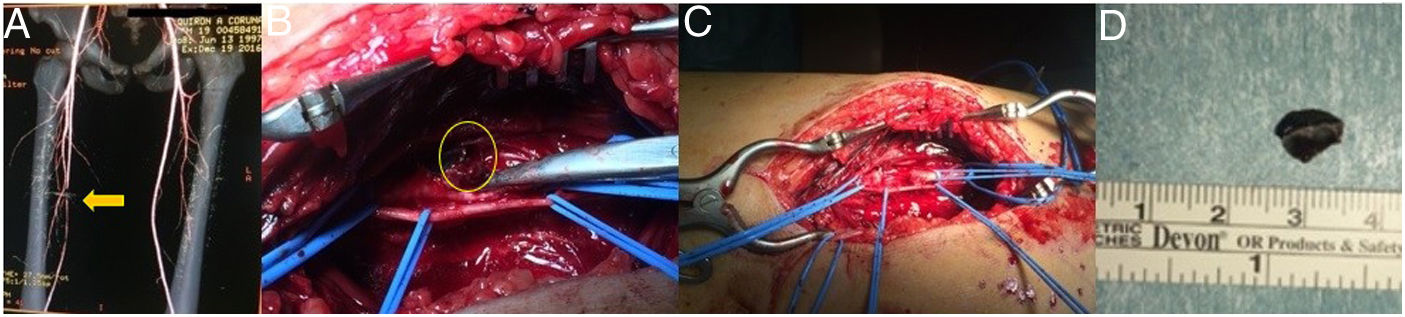
Case 1: A 19-year-old male was admitted by the Emergency Department and referred to our General Surgery Department with a diagnosis of cellulitis of the right thigh secondary to a foreign body. The patient had had a work accident involving shards from a mechanical saw. Examination revealed an incised wound with an entry orifice <1 cm on the inner side of the right thigh. Distal pulses were present. X-ray showed 2 subcentimeter splinters, and ultrasound found no alterations. The patient was admitted for surveillance and antibiotic therapy (iv amoxicillin clavulanate, 2 g/8 h). In the absence of fever, pain and progression of the cellulitis, the patient was discharged 48 h later. After 7 days, he was readmitted to the emergency department due to functional impotence and claudication. Abolition of the popliteal and distal pulse was observed, but femoral pulse was present. Doppler ultrasound detected a foreign body in the proximal middle third of the superficial femoral artery (SFA), with thrombosis. CT angiogram demonstrated a 7.5-mm metal body in contact with the SFA generating artifacts and preventing light assessment. Urgent surgery was indicated, which included: approach the SFA and extract the foreign body, thrombectomy and interposition of a 3 cm autologous femoro-femoral inverted saphenous graft. No postoperative complications were observed, and perfusion of the foot was recovered (Fig. 1).
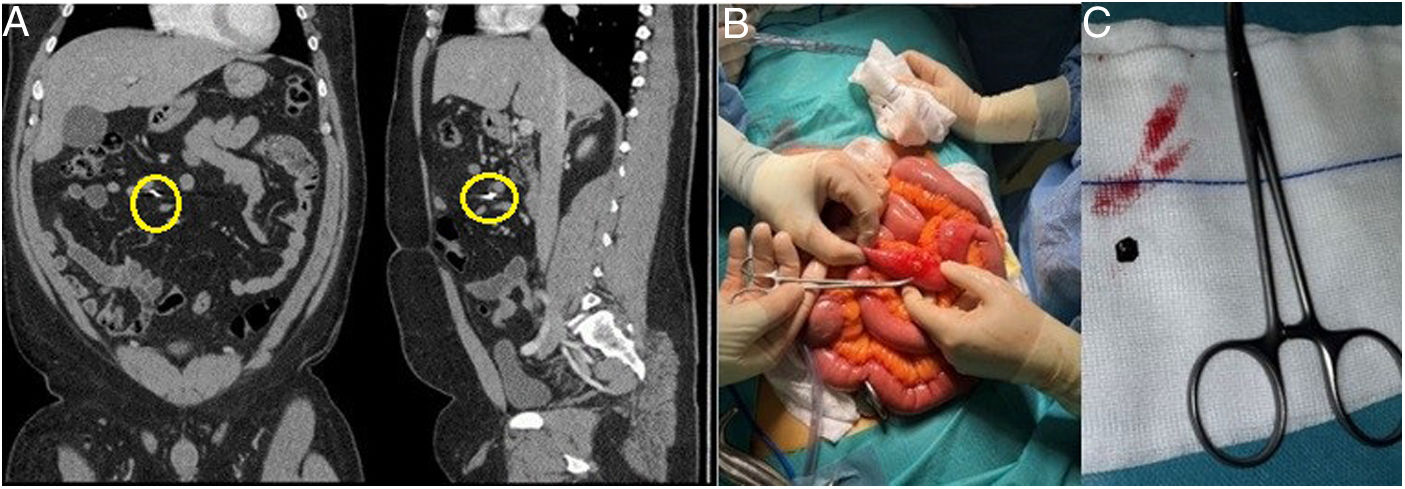
Case 2: A 41-year-old male came to the ER due to abdominal pain associated with the intra-abdominal penetration of metal shards from a fragment that accidentally detached from a work tool 6 h earlier. The patient was afebrile, with no nausea or vomiting, and hemodynamically stable (BP 112/75 mmHg; HR 82 bpm; SaO2 96%). Periumbilical cellulitis was observed around a punctate orifice. The abdomen was soft, depressible, slightly distended, with pain and selective guarding on palpation in the epigastrium. Lab work-up: Hb 15.1 g/dL, Hto 44.7%, Leukocytes 11.81 × 109/L (73.0% N), INR 1.06, Creatinine 0.99 mg/dL, Na+ 141.0 mEq/L, K+ 3.8 mEq/L. Chest X-ray was normal. Abdominal CT found a laceration of the right anterior rectus muscles with traumatic changes in the subcutaneous fat of the abdominal wall. A metallic projectile was observed in the mesenteric cavity, with no internal injuries to vital organs. Laparotomy was indicated. We observed the punctiform entry orifice in the right supraumbilical region, superficial cellulitis, and the projectile lodged in the middle mesoileum. A punctiform perforation was detected in the antimesenteric edge of the ileum, but no other injuries o free fluid were found. The foreign body was removed, and the perforation was sutured. The patient was discharged 6 days later, without complications (Fig. 2).
The initial approach to vascular trauma should follow the ATLS guidelines.3 It is important to evaluate the hard signs of vascular injury (active bleeding, expansive hematoma, thrill or absence of pulses), which indicate urgent surgery, and soft signs (non-pulsatile hematoma, neurological deficit, injury to a vascular pathway, weak distal pulse), which require supplementing the assessment with images.4 Early diagnosis and treatment are essential for limb preservation. For vascular repair, the injured vessel must be identified, proximal and distal control performed, followed by routine thrombectomy. If partial resection of the vessel is required, a tension-free repair should be conducted and, if excessive, an autologous graft or prosthesis is inserted. The gold standard technique involves using the saphenous vein of the leg contralateral to the trauma. If instability is detected, a vascular shunt is chosen for damage-control surgery. Patients require strict surveillance for signs of compartment syndrome if prophylactic fasciotomy was not performed.5
The management of abdominal penetrating trauma depends on the mechanism of injury, location, depth, number of wounds and hemodynamic stability. The projectiles cause parallel perforations, and the shock wave can cause injuries with greater tissue damage and necrosis. The small intestine is at greater risk of injury because it occupies a larger area of the abdomen. The AAST classifies wounds as non-destructive: grades I–II (<50% wall involvement) and III (>50% wall involvement without transection); or destructive: grades IV (complete dissection) and V (tissue loss/devascularization).6
In gunshot wounds, laparotomy has traditionally been considered mandatory. The WSES7 guidelines recommend non-operative management (NOM) in high-volume centers. Wound exploration to assess the entry orifice or laparoscopy can guide management towards NOM or laparotomy.8 In hemodynamically stable patients without abdominal pain or peritonism and a CT without lesions, NOM could be followed, but with a minimum of 48 h of observation. A negative CT scan should not be used as the sole determining factor for discharge. Candidates for direct laparotomy are those who present hard signs: instability, pain and peritonism, blood from the rectum, or intestinal content escaping through the wound.
This article demonstrates the importance of recording the mechanism of action of the trauma, together with physical examination and assessment of the injured anatomical area. Early diagnosis and treatment will prevent irreversible sequelae.
Conflict of InterestThe authors declare that they have no conflicts of interest.