The axillary lymph node dissection (ALND) histologic analysis remains the most accurate method for assessing lymph node metastases. However, sentinel lymph node biopsy (SLNB) has been proved as a valid technique in the case of patients with node negative clinically and radiologically avoiding ALND1–3.
Currently the neoadjuvant chemotherapy (NAC) can lead to pathological complete response (pCR) in up to 41% of patients4,5. However, the feasibility of performing a SLNB following NAC in patients initially presenting with biopsy proven node positive breast cancer remains on controversy. Several trials evaluated the use of SLNB to assess axillary response after NAC and potentially changed practice patterns6–9.
This study aims to evaluate SLNB as a safe diagnostic test for assessing the presence of residual metastatic disease after NAC, avoiding ALND in negative selective SLNB patients by the measurement of the false negative rate (FNR) and the receiver operating curve (ROC) analysis.
From January 2014 to December 2019 a cohort of 85 female patients with an invasive breast cancer positive-node (T0-4, N1-2) with a median age of 51 years (29–74 years) were included. Our study excluded patients with distant metastases. The study was performed in a single tertiary cancer centre.
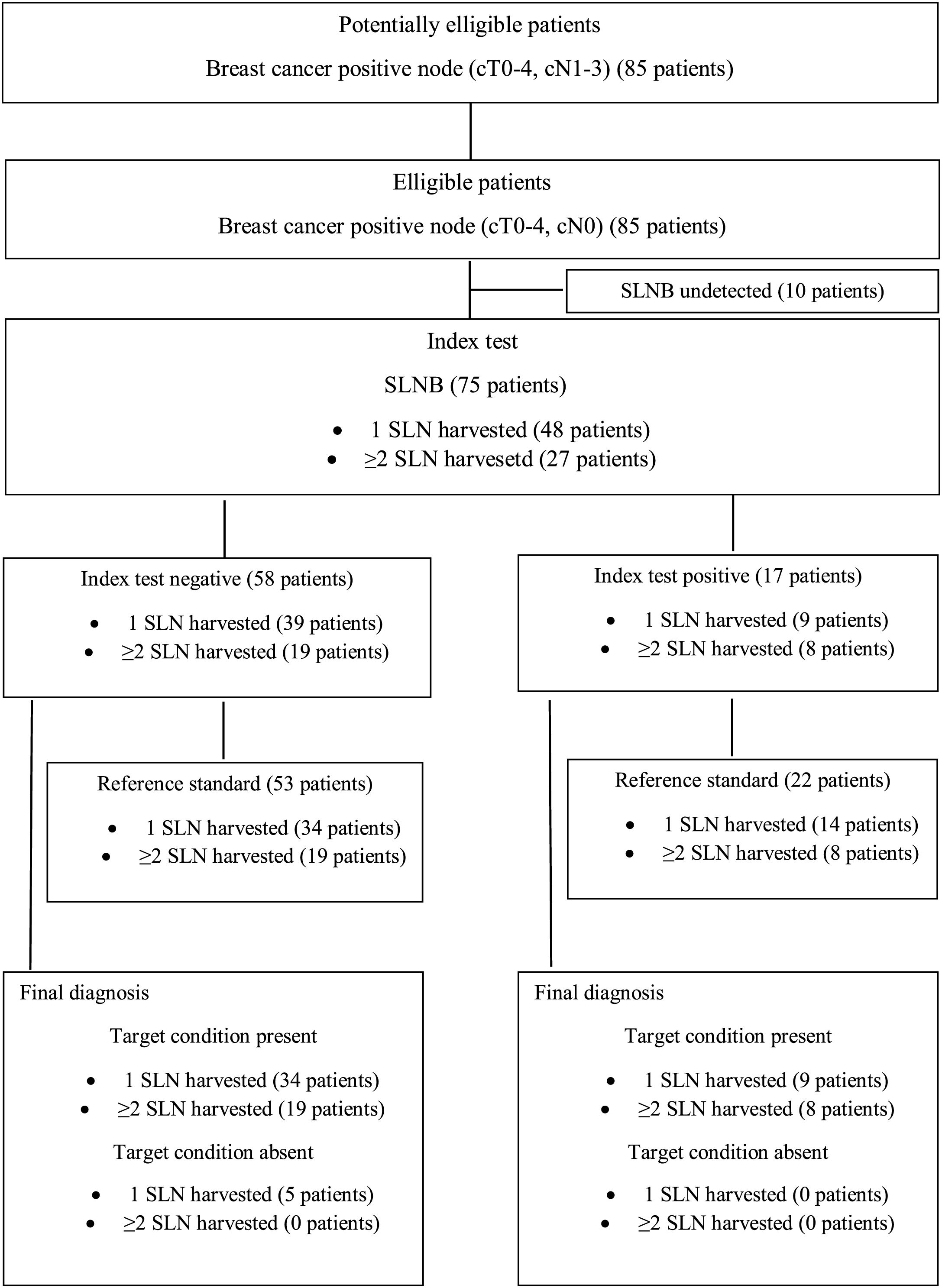
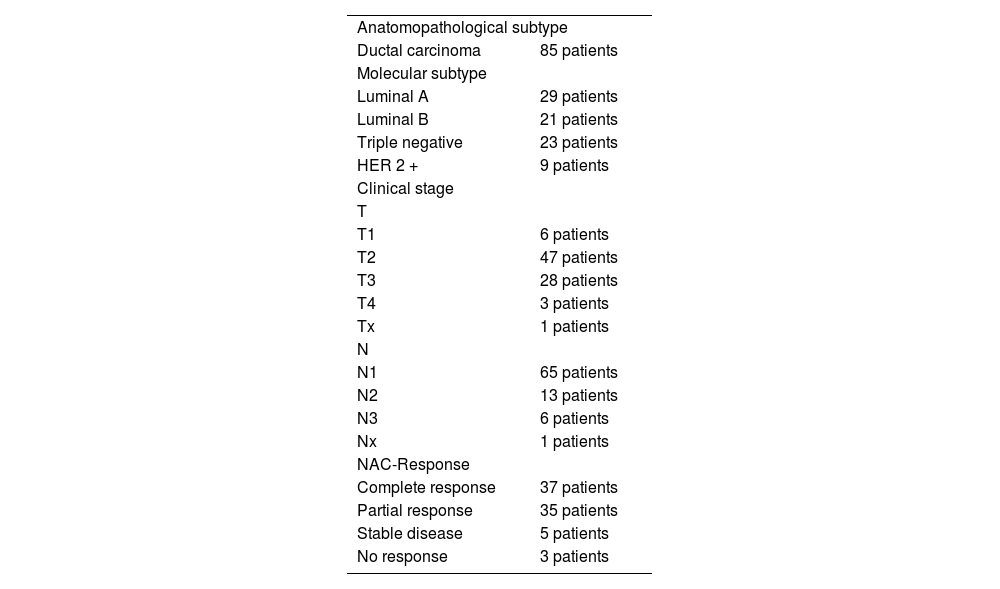
According to American Joint Committee Cancer (AJCC) classification a higher percentage of T2 (48 patients) followed by T3 (28 patients) was identified while N1 was mainly determined (66 patients) (Table 1). The histological subtype analysis showed ductal invasive carcinoma in every patient (Table 1). The immunohistochemical markers and consequently molecular subtype were determined and showed a higher percentage of luminal A subtype (29 patients) followed by luminal B subtype (21 patients), triple negative (23 patients) and HER2+ (9 patients) (Table 1). Clinical evaluation of the neoadjuvant chemotherapy response was determined by MR; complete response was registered in 37 patients, partial response in 35 patients, a stable disease in 5 patients and no response in 3 patients (Table 1). In relation to NAC approach, 41 patients received Cyclophosphamide + Adriamycin + Fluorouracil regimen plus Paclitaxel (39 patients) or Paclitaxel + Carboplatin (2 patients) while 44 patients received Adriamycin + Fluorouracil regimen plus Paclitaxel (17 patients), Paclitaxel + Trastuzumab + Pertuzumab (14 patients), Paclitaxel + Trastuzumab (8 patients) or Paclitaxel + Carboplatin (5 patients). All patients underwent surgical intervention, either mastectomy (34 patients) or tumorectomy (50 patients) plus SLNB plus ALND whatever the intraoperative result of SLN revealed. However, SLNB was analysed only in 75 patients as SLN was undetected in 10 patients.
Tumor characteristicics.
| Anatomopathological subtype | |
| Ductal carcinoma | 85 patients |
| Molecular subtype | |
| Luminal A | 29 patients |
| Luminal B | 21 patients |
| Triple negative | 23 patients |
| HER 2 + | 9 patients |
| Clinical stage | |
| T | |
| T1 | 6 patients |
| T2 | 47 patients |
| T3 | 28 patients |
| T4 | 3 patients |
| Tx | 1 patients |
| N | |
| N1 | 65 patients |
| N2 | 13 patients |
| N3 | 6 patients |
| Nx | 1 patients |
| NAC-Response | |
| Complete response | 37 patients |
| Partial response | 35 patients |
| Stable disease | 5 patients |
| No response | 3 patients |
Among patients with SLNB only 1 SLN was harvested in 48 patients while ≥2 SLN were harvested in 27 patients. On the other hand, the histopathological analysis showed complete remission in 53 patients (53 SLNB+ and 0 SLNB−) and residual disease in 30 patients (17 SLNB+ and 5 SLNB−) (Fig. 1)10. Among patients with 1 SLN harvested FNR, and sensitivity registered up to 35.7% and 64.3% respectively while among patients with ≥2 SLN harvested FNR, and sensitivity rates registered up to 0 and 100%. Additionally, the capacity of the SLNB to differentiate between patients with a pathologically positive or negative ALND was tested using a receiver operating curve characteristic (ROC) analysis. The ROC analysis registered an area under the curve (AUC) of 0,821 (95% confidence interval (CI) 0.662−0.981; p < 0.01) for 1 SLN harvesting group and an AUC of 100% (95% confidence interval (CI) 1-1; p < 0.01) for ≥2 SLN harvesting group which suggests SLNB is a valuable discriminator to prove ALND pathological results.
Our analysis showed a FNR drop from 35.7% to 0 if ≥2 SLN were obtained compared to only one SLN harvested. SN FNAC trial reported FNR decreased from 18% to 5% while accuracy increased from 87% to 97% if ≥2 SLN were obtained compared to only one SLN removed7. In the ACOSOG Z1071 trial the number of FN is lower for more than 3 nodes compared to 2 nodes6. The SENTINA trial reported a FNR of 24% for women who had one SLN removed and 18% for those who had ≥2 SLN8. Based on these trials, harvesting only one SLN is associated with a high FNR (SN FNAC 18%, ACOSOG Z1071 31%, SENTINA 24%), for this reason harvesting more ≥2 SLN should be recommended.
The SLNB after NAC in biopsy-proven node positive patients could be a valid alternative management to complete ALND. The identification of at least 2 sentinel nodes and further optimization of techniques by using the dual localization technique routine imaging of the axilla after NAC and marking the positive node with a marker clip and subsequent removal of the clipped node in addition to the SLNB, have shown lower FNR and higher accuracy
Our study has several limitations. Data were collected retrospectively, and the total number of patients was relatively small. Even more there were missing data on following variables: NAC-response (5 patients), molecular subtype (3 patients) and surgical intervention (1 patient). However, relevant results were found through our analysis and further studies are being supported in our hospital to change treatment patterns.
Authors’ contributionConception and design: Merayo Alvarez M.
Acquisition of data: Merayo Alvarez M, Alonso Martínez B, Calvo Rodríguez D.
Data analysis and interpretation: Merayo Alvarez M. Ortiz del Olmo D.
Manuscript writing: Merayo Alvarez M.
Final approval of manuscript: Alonso Martínez B, Llaneza Fogueras M A.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestAll authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.